Leadership and Management E-Portfolio Template
Student Name:
Course Name:
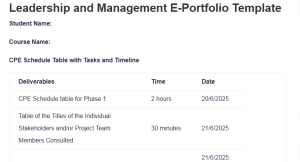
CPE Schedule Table with Tasks and Timeline
| Deliverables | Time | Date |
| CPE Schedule table for Phase 1 | 2 hours | 20/6/2025 |
| Table of the Titles of the Individual Stakeholders and/or Project Team Members Consulted | 30 minutes | 21/6/2025 |
| Needs Assessment Template | 2 hours | 21/6/2025: Leadership and Management E-Portfolio Template |
| SWOT Analysis Template | 2 hours | 21/6/2025 |
| Impact Analysis Template | 2 hours | 21/6/2025 |
| Phase 1 Go React Video Reflections (3 screenshots) | 1 hour | 22/6/2025 |
| Phase 1 Written Summary | ||
| Total: | 9.5 hours |
Table of the Titles of the Individual Stakeholders and/or Project Team Members Consulted
| Stakeholder/Project Team Member | Titles |
| S.H. | Inpatient Director |
| M. O. | Inpatient Director |
| P.T. | ER Director |
| N.N. | Nurse Educator |
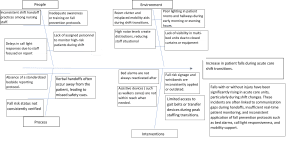
Needs Assessment
SWOT Analysis
| Factors to Maximize | Factors to Mitigate |
| Strengths | Weaknesses |
|
1. Strong Leadership Support: Hospital leadership actively supports fall prevention initiatives, which provide strategic direction and resource allocation for change efforts. 2. Existing Fall Prevention Protocols: The hospital already uses fall-risk assessments, wristbands, and signage, providing a foundation for integrating bedside shift reporting into care routines (Turner et al., 2022). 3. Patient-Centered Culture: The organization emphasizes patient safety and engagement, which aligns well with bedside reporting that involves patients in their care. 4. Interdisciplinary Collaboration: Nurses, aides, and quality improvement teams already collaborate on safety efforts, fostering a team-based approach to implementation. |
1. Inconsistent Handoff Practices: Variability exists in how staff currently conduct reports, leading to inconsistent communication and missed fall-risk cues (Heng et al., 2022). 2. Resistance to Change: Some staff may be hesitant to alter shift handoff routines, especially when under time constraints, impacting adoption rates. 3. Time Pressures During Shift Changes: Staff are often pressed for time at shift change, making it difficult to incorporate thorough patient-centered handoffs without workflow adjustments. 4. Limited Education and Training on New Protocols: Not all staff are trained in bedside reporting or its relevance to fall prevention, which may cause confusion or errors during handoffs. |
| Opportunities | Threats |
|
1. System-Wide Standardization: The benefits of its successful implementation may include standardization of bedside reporting at all units, which may help to enhance care continuation and prevention of falls throughout the hospital. 2. Enhanced Patient Engagement: Engagement in bedside reporting enables patients to raise their voices in order to be heard and enhances the awareness of fall prevention. 3. Improved Patient Satisfaction Scores: Handoff that makes safety activities visible and promotes transparent communication may result in increased HCAHPS scores and positive patient feedback (Jun et al., 2020). 4. Access to Evidence-Based Tools: The organization can use validated toolkits and EBP models (such as AHRQ Fall Toolkit) to guide implementation and staff training (Dykes et al., 2020). |
1. Noncompliance With Protocol: During heavy duty times, staff can decide not to read bedside reports selectively, negating the goal of establishing consistency and safety in the intervention. 2. Increased Shift Duration: Conducting complete bedside reporting can cost time during shift changes, contributing to overtime or congestion in the work process. 3. Potential Patient Discomfort: Patients can have feelings of being uncomfortable with the staff conversing at the bedside, particularly when confidential matters are discussed (Wensley et al., 2020). 4. Resource Limitations: Limited staffing levels or high patient acuity during shift changes could reduce the feasibility of consistently executing bedside handoffs. |
D156 Task 1 Impact Analysis
Benefits
| Category | Benefit | Rating |
| Patient Safety | 1. Reduction in fall-related injuries, leading to improved recovery and fewer complications. | 3 |
| 2. Improved monitoring through direct visualization of patients during bedside shift handoffs. | 3 | |
| Staff Efficiency | 1. Enhanced communication among staff during transitions, reducing missed information and errors. | 3 |
| 2. Improved prioritization of patient care needs at the beginning of each shift. | 3 | |
| Total Benefits Score | 12 | |
Risks
| Category | Risk | Rating |
| Patient Safety | 1. Inconsistent implementation of bedside reporting may lead to lapses in patient monitoring. | 3 |
| 2. Potential discomfort for patients during bedside discussions, especially with sensitive information. | 2 | |
| Staff Efficiency | 1. Perceived increase in workload or handoff duration may lead to staff resistance. | 3 |
| 2. Additional time needed for bedside reports could lead to overtime or shift delays. | 2 | |
| Total Risks Score | 10 | |
Impact Ratio = 1.2____
Impact Ratio > 1, the benefits outweigh the risks.
Impact Ratio = 1, there is no difference between the benefits and the risks.
Impact Ratio < 1, the risks outweigh the benefits.
Video Screenshots
Phase 2 Video Reflection
Hello, my name is Deiokie Rambally. In this video reflection, I will discuss the results of my needs assessment, SWOT analysis, and impact analysis of my fall prevention initiative in the acute care setting. This initiative aims to address the increasing rate of patient falls during shift changes. In examining the causes of falls and reviewing the effectiveness of proposed solutions, I have also gained a deeper understanding of the conditions that contribute to patient safety and the necessary steps to enhance it.
Needs Assessment Reflection
In the needs assessment process, I employed the cause and effect diagram or the fishbone model to uncover what causes these patient falls to occur during shifts. There were mainly four domains: people domain, process domain, environment domain and interventions domain. The communication breakdowns and the preoccupation of staff with documenting information at shift change were apparent under the people category, leaving high-risk patients unattended. The analysis of the process showed discrepancies in the handoff procedures, and there was no standard procedure regarding re-evaluating the safety risk of patients.
Environmental issues were disorganized corridors and low lights that posed the probability of falling and slowed staff reaction to alerts. Finally, among the interventions, bed alarms, call lights, and fall-risk signages were not checked and used during handoffs consistently. These findings confirmed that the shift change process is an urgent area where improvements are necessary, and they promoted the adoption of bedside reporting as a specific approach where they should focus their efforts to impact the higher level of real-time patient monitoring and engagement.
SWOT Analysis Reflection
The SWOT analysis also considered the internal and external environment that might affect bedside shift reporting implementation. Some of the strengths were strong leadership support hospital culture involving patient safety, among other assets, and the existence of fall prevention protocols consistent with the proposed change. Nonetheless, weaknesses were also evident, one of which was staff resistance that stemmed due to fear that the new process would increase shift length and complexity, thus making their jobs harder, and lack of information concerning the purpose and implementation of bedside handoffs.
The opportunities included the possibility of wider adoption in the hospital, the enhancement of ensuring better standardization, and the impact on satisfaction by engaging the patients. Meanwhile, a few threats were discovered, such as irregular compliance, a certain level of discomfort when sharing sensitive data in the presence of patients and families, and transition delays due to limited time in already crowded transitions. Nevertheless, the SWOT analysis has revealed that the benefits could be attained by means of effective leadership, training and staff assistance.
Impact Analysis Reflection
The impact analysis enabled me to measure the advantages and the threats of having bedside reporting. I centered on two major categories, which are patient safety and staff efficiency. The main advantages of patient safety entailed the fall-related injury numbers being reduced remarkably and handoff patient monitoring consistency being improved, both rated high-impact changes.
To enhance staff efficiency, there were advantages such as improvement in communication between shifts and prioritization of care activities at the onset of each change. The overall score on benefits was 12, which means a high possibility of better results.
Regarding the risk, I noted the factors, including personnel reluctance to change, increased time of handoffs, and patient discomfort due to bedside conversations. They also were tallied and came to a risk score of 10. The impact ratio yielded was 1.2, indicating that there were positive benefits present as compared to the risks. This discussion confirmed the use of the intervention as effective and feasible, provided that there are sufficient levels of training and leadership support.
Conclusively, the results of the needs assessment, SWOT analysis, and impact analysis have offered crucial information on the most significant factors that determine falls and the effectiveness of implementing fall prevention plans. Leadership actively supports the project, and the bedside reporting initiative will enhance efficiency and enhance patient safety. Although there are still challenges, the proposed solutions are expected to yield a positive impact, reducing the number of falls and improving the quality of patient care.
References
Dykes, P. C., Burns, Z., Adelman, J., Benneyan, J., Bogaisky, M., Carter, E., Ergai, A., Lindros, M. E., Lipsitz, S. R., Scanlan, M., Shaykevich, S., & Bates, D. W. (2020). Evaluation of a patient-centered fall-prevention tool kit to reduce falls and injuries. JAMA Network Open, 3(11), 1–10. https://doi.org/10.1001/jamanetworkopen.2020.25889
Heng, H., Kiegaldie, D., Slade, S. C., Jazayeri, D., Shaw, L., Knight, M., Jones, C., Hill, A.-M., & Morris, M. E. (2022). Healthcare professional perspectives on barriers and enablers to falls prevention education: A qualitative study. PLOS ONE, 17(4), e0266797. https://doi.org/10.1371/journal.pone.0266797
Jun, J., Stern, K., & Djukic, M. (2020). An integrative review of the interventions for improving patients’ experiences revealed in quality improvement projects. Journal of Patient Experience, 7(6), 882–892. https://doi.org/10.1177/2374373520925271
Turner, K., Staggs, V. S., Potter, C., Cramer, E., Shorr, R. I., & Mion, L. C. (2022). Fall prevention practices and implementation strategies. Journal of Patient Safety, 18(1), 236–242. https://doi.org/10.1097/pts.0000000000000758
Wensley, C., Botti, M., McKillop, A., & Merry, A. F. (2020). Maximising Comfort: How Do Patients Describe the Care That Matters? A Two-stage Qualitative Descriptive Study to Develop a Quality Improvement Framework For Comfort-related Care in Inpatient Settings. BMJ Open, 10(5), E033336. https://doi.org/10.1136/bmjopen-2019-033336
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
D156 Business Case Analysis ( Beginning of Capstone ): Task 1 – E portfolio
TOPIC APPROVED BY PROFESSOR – FALL PREVENTION IN ACUTE CARE
- ALL INTERVENTIONS MUST BE EVIDENCED BASED
This course builds the foundation for all the other tasks to follow in my capstone
I have included a sample Eportfolio to show what the final assignment should look like
Leadership and Management E-Portfolio Template
I have also included the professors information/ guidance of the assignment for task 1 and task 2. Task 2 will follow after task 1 is completed
CPE RECORD GIVES THE DIRECTIONS FOR THE EPORTFOLIO
PLEASE SEND TRANSCRIPT FOR THE GO REACT VIDEO ( I WILL DO THE RESPONSES TO PEERS)
SUPPORTING DOCUMENTS: (I’ve included all the attachments listed below in the link)
- Leadership and Management E-Portfolio Template
- Impact Analysis Template.docx
- SWOT Analysis Template.docx
- GoReact Instructions.docx
- Needs Assessment Template.docx