Recommending an Evidence-Based Practice Change
Hello, and welcome to today’s presentation on Recommending an Evidence-Based Practice Change.
Our healthcare organization is a private health facility that provides both inpatient and outpatient services, focusing on mental health. It is focused on psychiatric and behavioral health, which is essential for the effective treatment of patients with eating disorders like binge eating disorder and bulimia nervosa. It is a client-centered culture with complex approaches and responsibilities, which are delivered in an integrated model of patient-care approaches such as physical and psychological-emotional. Employees are empowered to be involved in decision-making regarding practice and/or treatment decisions. Various leadership encourages clinical improvements and backs any efforts that embrace EBP principles. Nevertheless, the level of preparedness for structured practice change is moderate. Leadership is supportive, though disparities still exist among the different staff groups, some of which are reluctant to embrace a new treatment regime. Education and change management practices must also be targeted to increase staff engagement in implementing effective changes for evidence-based practices in the organization.
In the current context, the treatment of BED and BN comprises psychotherapy, especially CBT, but does not entail the use of drugs regularly. Still, findings show that integrating CBT with pharmacotherapy for other treatments, like GLP-1 receptor agonists, further improves the results (Aoun et al., 2024). These findings contribute to high relapse rates, patient dissatisfaction, and poor long-term patient outcomes or recovery patterns. The lack of integration of care provision ensures that the psychological, as well as the physiological, aspects of eating disorders remain poorly responded to. Researchers have found that combining treatments yields higher remission rates and metabolic enhancements compared to a single-treatment approach. Hence, the targeted opportunity is presenting the proposal of an integrated model of psychotherapy with pharmacological treatments for the patient’s overall health. Based on the evidence, this could significantly decrease relapse, enhance engagement, and enable better health rates in all patients.
The problem is relevant for adult patients with BED and BN in outpatient and inpatient psychiatric settings. Some of the key stakeholders include nursing staff, psychiatrists, psychologists, dietitians, leadership teams, and patients (Pehlivan et al., 2022). This will be especially important to ensure the active participation of stakeholders in the implementation and continuation of the change. Challenges include staff resistance to using pharmacological interventions for the treatment of disorders that may primarily have been managed by psychotherapy alone. Patients receiving pharmacotherapies like glycogen-like protein-1 receptor agonists may develop psychiatric as well as metabolic side effects. Strong staff education and interdisciplinary approaches will be needed to address these risks. If a stakeholder’s concern is handled early and frequently, they are much more likely to support the project. Therefore, by adopting this change with caution and implementing it in such a way that ensures the clients’ safety in case of reaction, the extent of the project, as well as the project’s overall impact on the patient’s health status, will be enhanced.
The proposed EBP change aims at combining CBT with pharmacological therapies, particularly GLP-1 receptor agonists, for patients with BED and BN. Studies show that CBT helps handle these cognitive and emotional factors related to eating disorders, while pharmacological medications such as the GLP-1 agonist help in managing appetite and metabolic regulation, which aids in minimizing binge episodes and the general management of the patient’s weight. These approaches target the biological, psychological, and social aspects of BED/BN, hence improving the remission and recovery outcomes (Monteleone et al., 2022). Specific treatment plans would involve individualized adjustments to therapy and medications based on their severity, associated illnesses, and the patient’s choice. This model adheres to the American Psychiatric Association-approved practice guidelines and the most recent trend in the field. Integrating the described model will make our organization one of the most progressive and patient-oriented eating disorder center providers regarding the treatment spectrum.
Knowledge transfer is critical to successfully adopting the integrated care model. The first step will include conducting formal training sessions where all the involved staff will be guided through the valuable information on CBT combined with pharmacotherapy. Real interdisciplinary collaboration will be fostered by implementing consolidated elements of care networks for BED/BN (Grilo & Juarascio, 2023). It will be further recommended that a clear clinical protocol should be developed and implemented outlining patient inclusion, and procedures to be followed in the treatment process, monitoring, and follow-up. An initial trial will occur in one eating disorder treatment unit, and data will primarily be gathered on the impact of the intervention on the patients as well as feedback from staff. Feedback from surveys and focus groups will help to identify problems in the process and adjust plans for further steps before the scale-up. It is critical to regularize feedback cycles to enhance consistent practice change. Implementation needs to be adaptive, sustainable, and based on proof that it works so that more patient benefits can be seen in the long run.
Effective dissemination ensures that the evidence-based change achieves organizational awareness, acceptance, and adoption. An internal evidence-based practice workshop will be conducted to ensure all stakeholders are reached, including research, the pilot study, and clinical practice protocols. Interdisciplinary presentations during the formal grand rounds will also add to the interactions between physicians, nurses, and therapists across departments. Some summarized findings will be disseminated more thoroughly, including the conclusions outlined in the hospital’s internal nursing magazine. External dissemination will involve presented abstracts at professional mental health and nursing conferences. Face-to-face interventions such as workshops and grand rounds are essential as they promote interaction and communication and formally establish interprofessional relationships among the stakeholders (Koreshe et al., 2023). The use of only passive means does not suffice to foster practice change. Consequently, the use of multiple modes of communicating information makes a specialty of reaching out to different audiences so that knowledge inculcation becomes effective and is put into practice.
The primary outcome will be measured by the decreased binge eating episodes of the patients, as mentioned by the patients themselves and the health practitioners. Secondary objectives will be correlated with BMI increases and body weight stabilization, measured using standard tools (Koreshe et al., 2023). We anticipate that patients in combined psychotherapy and pharmacotherapy will have a higher percentage of attendance in their sessions and better medication refill rates. Outcomes regarding the level of patient satisfaction shall be measured with patient surveys undertaken after the treatment process. Also, we expect reduced readmission to hospital rates and relapse incidences among BED/BN patients. Lastly, the project will assess changes in interdisciplinary collaboration by receiving surveys from the staff about the communication and coordination of care in the teams. Each of them will be compared pre and post-implementation to measure the impact of the evidence-based change in practice using best models.
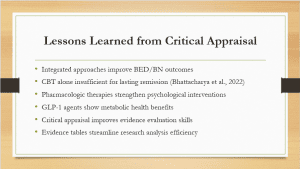
From the critical appraisal, I understood that there is evidence in practice that integrated approaches lead to better outcomes for EB and BN. Cognitive Behavioral Therapy alone, although helpful, is not enough to guarantee remission in the long run (Bhattacharya et al., 2022). Pharmacological treatments, especially GLP-1 agonists, present other physiological benefits that support and enhance the results of psychological therapy. Critical appraisal using an appropriate standard checklist helped me identify high-quality studies essential for effective evidence-based practice. The Evaluation Table was useful in structuring extensive and detailed information and aiding in comparing data from one study to the other. Altogether, this process enriched my knowledge of the relationship between the quality of evidence, adequacy of methods, and practical relevance of the obtained knowledge for practice. Critique is a tool in evaluation and a means to promote safe, efficient, and patient-oriented treatment decisions.
Aoun, L., Almardini, S., Saliba, F., Haddadin, F., Mourad, O., Jdaidani, J., Morcos, Z., Saidi, I. A., Sanayeh, E. B., Saliba, S., Almardini, M., & Zaidan, J. (2024). GLP-1 receptor agonists: A novel pharmacotherapy for binge eating (Binge eating disorder and bulimia nervosa)? A systematic review. Journal of Clinical & Translational Endocrinology, 35, 100333. https://doi.org/10.1016/j.jcte.2024.100333
Bhattacharya, S., Goicoechea, C., Heshmati, S., Carpenter, J. K., & Hofmann, S. G. (2022). Efficacy of cognitive behavioral therapy for anxiety-related disorders: A meta-analysis of recent literature. Current Psychiatry Reports, 25(1), 19–30. https://doi.org/10.1007/s11920-022-01402-8
Grilo, C. M., & Juarascio, A. (2023). Binge-Eating disorder interventions: Review, current status, and implications. Current Obesity Reports, 12(3), 406–416. https://doi.org/10.1007/s13679-023-00517-0
Koreshe, E., Paxton, S., Miskovic-Wheatley, J., Bryant, E., Le, A., Maloney, D., National Eating Disorder Research Consortium, Touyz, S., & Maguire, S. (2023). Prevention and early intervention in eating disorders: findings from a rapid review. Journal of Eating Disorders, 11(1). https://doi.org/10.1186/s40337-023-00758-3
Monteleone, A. M., Pellegrino, F., Croatto, G., Carfagno, M., Hilbert, A., Treasure, J., Wade, T., Bulik, C. M., Zipfel, S., Hay, P., Schmidt, U., Castellini, G., Favaro, A., Fernandez-Aranda, F., Shin, J. I., Voderholzer, U., Ricca, V., Moretti, D., Busatta, D., . . . Solmi, M. (2022). Treatment of eating disorders: A systematic meta-review of meta-analyses and network meta-analyses. Neuroscience & Biobehavioral Reviews, 142, 104857. https://doi.org/10.1016/j.neubiorev.2022.104857
Pehlivan, M. J., Miskovic-Wheatley, J., Le, A., Maloney, D., Consortium, N. E. D. R., Touyz, S., & Maguire, S. (2022). Models of care for eating disorders: findings from a rapid review. Journal of Eating Disorders, 10(1). https://doi.org/10.1186/s40337-022-00671-1
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Recommending an Evidence-Based Practice Change
Evidence-Based Project, Part 4: Recommending an Evidence-Based Practice Change
The collection of evidence is an activity that occurs with an endgame in mind. For example, law enforcement professionals collect evidence to support a decision to charge those accused of criminal activity. Similarly, evidence-based healthcare practitioners collect evidence to support decisions in pursuit of specific healthcare outcomes.
Recommending an Evidence-Based Practice Change
In this Assignment, you will identify an issue or opportunity for change within your healthcare organization and propose an idea for a change in practice supported by an EBP approach.
Resources
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
- Hoffman, T. C., Montori, V. M., & Del Mar, C. (2014). The connection between evidence-based medicine and shared decision makingLinks to an external site.. Journal of the American Medical Association, 312(13), 1295–1296. doi:10.1001/jama.2014.10186
- Kon, A. A., Davidson, J. E., Morrison, W., Danis, M., & White, D. B. (2016). Shared decision making in intensive care units: An American College of Critical Care Medicine and American Thoracic Society policy statementLinks to an external site.. Critical Care Medicine, 44(1), 188–201. doi:10.1097/CCM.0000000000001396
- Opperman, C., Liebig, D., Bowling, J., & Johnson, C. S., & Harper, M. (2016). Measuring return on investment for professional development activities: Implications for practiceLinks to an external site.. Journal for Nurses in Professional Development, 32(4), 176–184. doi:10.1097/NND.0000000000000483
- Schroy, P. C., Mylvaganam, S., & Davidson, P. (2014). Provider perspectives on the utility of a colorectal cancer screening decision aid for facilitating shared decision makingLinks to an external site.. Health Expectations, 17(1), 27–35. doi:10.1111/j.1369-7625.2011.00730.xThe Ottawa Hospital Research Institute. (2019). Patient decision aidsLinks to an external site.. Retrieved from https://decisionaid.ohri.ca/
To Prepare:
- Reflect on the four peer-reviewed articles you critically appraised in Module 4, related to your clinical topic of interest and PICOT.
- Reflect on your current healthcare organization ( mental health hospital) and think about potential opportunities for evidence-based change, using your topic of interest and PICOT as the basis for your reflection.
- Consider the best method of disseminating the results of your presentation to an audience.
The Assignment: (Evidence-Based Project)
Part 4: Recommending an Evidence-Based Practice Change
Create an 8- to 9-slide narrated PowerPoint presentation with speaker notes in which you do the following:
- Briefly describe your healthcare organization, including its culture and readiness for change. (You may opt to keep various elements of this anonymous, such as your company name.)
- Describe the current problem or opportunity for change. Include in this description the circumstances surrounding the need for change, the scope of the issue, the stakeholders involved, and the risks associated with change implementation in general.
- Propose an evidence-based idea for a change in practice using an EBP approach to decision making. Note that you may find further research needs to be conducted if sufficient evidence is not discovered.
- Describe your plan for knowledge transfer of this change, including knowledge creation, dissemination, and organizational adoption and implementation.
- Explain how you would disseminate the results of your project to an audience. Provide a rationale for why you selected this dissemination strategy.
- Describe the measurable outcomes you hope to achieve with the implementation of this evidence-based change.
- Be sure to provide APA citations of the supporting evidence-based peer reviewed articles you selected to support your thinking.
- Add a lessons learned section that includes the following:
- A summary of the critical appraisal of the peer-reviewed articles you previously submitted(attached in files below)
- An explanation about what you learned from completing the Evaluation Table within the Critical Appraisal Tool Worksheet Template (1-3 slides)(attached in files below)