Patient Logs
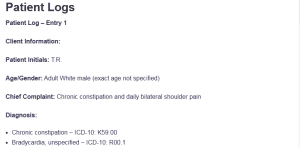
Patient Log – Entry 1
Client Information:
Patient Initials: T.R.
Age/Gender: Adult White male (exact age not specified)
Chief Complaint: Chronic constipation and daily bilateral shoulder pain
Diagnosis:
- Chronic constipation – ICD-10: K59.00
- Bradycardia, unspecified – ICD-10: R00.1
- Pain in right shoulder – ICD-10: M25.511
- Pain in left shoulder – ICD-10: M25.512: Patient Logs
Procedure:
- Comprehensive GI and cardiovascular history and physical exam
- Musculoskeletal assessment of bilateral shoulders
- Abdominal palpation and bowel habit evaluation
- Pain severity rating and range of motion testing
- Physical therapy follow-up review
Treatment Plan and Notes:
T.R., a White male, presented with a 7-year history of chronic constipation, occurring about once weekly. He manages symptoms with increased water intake and denies blood in stool, GI evaluations, or abdominal surgery. Cardiac MRI showed bradycardia (HR 40s), but he remains asymptomatic and untreated. He also reports daily bilateral shoulder pain (3/10), attributed to a 2016-2017 fall when he broke his leg and landed on both shoulders.
No treatment was initially sought. Pain is aggravated by lifting and is described as sharp and aching. He is currently undergoing physical therapy and uses no medications. The exam revealed mild tenderness and limited motion.
Referred to GI and advised to keep a bowel diary. Lifestyle and non-pharmacologic strategies were reinforced.
Patient Log – Entry 2
Client Information:
Patient Initials: M.J.
Age/Gender: 45-year-old White male
Chief Complaint: Follow-up for severe anemia and ongoing GI symptoms
Diagnosis:
- Iron deficiency anemia – ICD-10: D50.9
- Irritable bowel syndrome – ICD-10: K58.0
- Celiac disease – ICD-10: K90.0
- Barrett’s esophagus – ICD-10: K22.70
- Major depressive disorder, recurrent – ICD-10: F33.1
- Generalized anxiety disorder – ICD-10: F41.1
- History of alcohol and substance abuse – ICD-10: F10.20
Procedure:
- Post-hospitalization follow-up after EGD and colonoscopy with biopsy
- Review of GI symptoms: bloating, diarrhea, constipation, abdominal pain
- Mental health screening and substance use history
- Medication reconciliation and lab monitoring for anemia
- Nutritional and dietary counseling (gluten-free adherence review)
Treatment Plan and Notes:
M.J. presented for follow-up after hospitalization for severe anemia, during which he had an EGD and colonoscopy with biopsy. He reports ongoing bloating, alternating diarrhea and constipation, and abdominal pain. His history includes anemia, IBS, newly diagnosed celiac disease (2024), Barrett’s esophagus (2020), depression, anxiety, and alcohol/substance use.
He takes ferrous sulfate 325mg BID, vitamin D 5000U daily, and pantoprazole 40mg daily. Despite adherence, GI symptoms persist. He was counseled on strict gluten-free compliance and gradual fiber increase.
A Dietitian referral was made. He declined behavioral health services. A CBC and iron panel were ordered. Follow-up is planned in four weeks.
Patient Log – Entry 3
Client Information:
Patient Initials: S.B.
Age/Gender: 35-year-old White male
Chief Complaint: Chronic lower back pain worsened by heavy lifting
Diagnosis:
- Chronic low back pain – ICD-10: M54.5
- Scoliosis, unspecified – ICD-10: M41.9
- Muscle spasm – ICD-10: M62.830
Procedure:
- Comprehensive lumbar spine musculoskeletal exam
- Pain severity rating (7/10) and functional impairment review
- Neurological exam: sensation, reflexes, motor function
- Postural and gait assessment
- Review of prior imaging (MRI ×3)
Treatment Plan and Notes:
S.B. presented with chronic lower back pain, described as “punching,” with daily muscle spasms rated 7/10. The pain is aggravated by heavy lifting and interferes with daily tasks such as car repairs. The patient has a known history of scoliosis and reports no prior back injuries, surgeries, or engagement in physical therapy. During the examination, sensation was present and normal on both sides, so there were no symptoms of nerve damage in the spinal nerve roots or difficulty with bowel or bladder control.
There was mild tightness and guarding in the lower back muscles, yet gait and posture did not change. Up to now, there have been three MRIs without any therapy given after. The patient was educated about starting a routine physical therapy, taking care when lifting, and doing mild daily stretches.
The doctor sent a note to physical therapy, wanting the patient to follow up, and suggested taking NSAIDs for any pain as needed. The patient was advised to return in four weeks so the doctor could assess his progress and suggest more pain relief strategies.
Patient Log – Entry 4
Client Information:
Patient Initials: C.J.
Age/Gender: 64-year-old White male
Chief Complaint: Daily right arm and leg pain
Diagnosis:
- Pain in right upper limb – ICD-10: M79.601
- Pain in right lower limb – ICD-10: M79.605
- Peripheral neuropathy – ICD-10: G62.9
Procedure:
- Comprehensive neuromuscular assessment of right upper and lower limbs
- Pain scale rating (5/10) and description documentation
- Functional assessment for daily activities and work tasks
- Review of current non-pharmacological pain management (stretching)
- Screening for neurological deficits and motor function
Treatment Plan and Notes:
C.J., a teacher who also runs a tractor-trailer, complained of a continuous ache in his right arm and leg that he rated as 5/10. He experiences peripheral neuropathy and relieves the symptoms by stretching regularly. He states that he did not take any drugs from the pharmacy or pharmacy counter. On physical examination, motor strength and sensation were intact, with no focal neurological deficits.
Gait was normal, and joint mobility was preserved. Pain appeared to be neuropathic and functionally limiting but stable. Education focused on ergonomics and stretching techniques for symptom relief. The patient was advised to maintain regular movement, avoid prolonged static postures, and continue current non-pharmacologic interventions.
Referral to neurology was offered for further evaluation if symptoms worsen or interfere with work. Follow-up is planned in four weeks to monitor stability and discuss additional pain control strategies if needed.
Patient Log – Entry 5
Client Information:
Patient Initials: H.L.
Age/Gender: 50-year-old White female
Chief Complaint: Follow-up for skin rash and recent fall down stairs
Diagnosis:
- Dermatitis, unspecified – ICD-10: L30.9
- Elevated liver enzymes – ICD-10: R74.0
- Rib pain following fall – ICD-10: S29.011A
- Acute low back pain – ICD-10: M54.5
Procedure:
- Skin inspection of the upper arm and abdominal regions
- Review of laboratory liver panel
- Pain severity assessment (rated 10/10)
- Musculoskeletal evaluation of back and ribs
- Medication reconciliation and fall risk screening
Treatment Plan and Notes:
H.L. presented for a follow-up visit regarding two ongoing concerns: an itchy rash and pain following a fall down 10 stairs. She described the rash as affecting her upper arm and stomach, for which she has been self-treating with OTC hydrocortisone, reporting partial relief. A physical exam revealed erythematous, non-weeping patches without open lesions. Concurrently, she reported severe intermittent back and rib pain rated 10/10, managed with OTC Tylenol 500mg.
No prescription medications are currently taken. A musculoskeletal exam showed tenderness on palpation over the thoracic spine and right lateral ribs, with no signs of deformity or crepitus. A recent lab panel revealed elevated liver enzymes; follow-up LFTs were ordered, and possible hepatotoxicity from prolonged acetaminophen use was discussed.
She was advised to limit Tylenol, apply cold compresses to sore areas, and monitor for increased pain or respiratory symptoms. Dermatology and hepatology referrals were provided to address the rash and liver enzyme elevation, respectively.
Patient Log – Entry 6
Client Information:
Patient Initials: R.D.
Age/Gender: 40-year-old White male
Chief Complaint: Follow-up for uncontrolled hypertension
Diagnosis:
- Essential (primary) hypertension – ICD-10: I10
- Obstructive sleep apnea – ICD-10: G47.33
Procedure:
- Blood pressure monitoring and trend review
- Medication adherence and dosing evaluation
- Cardiovascular risk factor screening
- Sleep history and CPAP compliance discussion
- Symptom check: dizziness, lightheadedness, fatigue
Treatment Plan and Notes:
R.D. returned for a follow-up regarding elevated blood pressure readings despite current antihypertensive treatment. He has a history of hypertension and obstructive sleep apnea and is currently taking Losartan 10mg once daily. He denied any dizziness or lightheadedness and reported good general energy levels. Blood pressure measured during the visit was mildly elevated.
A review of medication usage revealed consistent adherence. Discussion centered on the potential need for dose adjustment or the addition of a second antihypertensive agent. Lifestyle factors such as sodium intake, weight, stress, and physical activity were addressed.
The patient was advised to monitor BP at home twice daily and maintain a log. CPAP compliance was reviewed; he reported regular nightly use. A repeat panel was ordered to evaluate renal function and electrolytes. Follow-up is scheduled in two weeks to reassess BP response and determine if medication titration is warranted.
Patient Log – Entry 7
Client Information:
Patient Initials: J.M.
Age/Gender: 59-year-old White male
Chief Complaint: Severe left knee pain with daily flare-ups
Diagnosis:
- Pain in left knee – ICD-10: M25.562
- Congestive heart failure – ICD-10: I50.9
- Essential (primary) hypertension – ICD-10: I10
Procedure:
- Musculoskeletal examination of left knee joint
- Pain scale assessment (rated 10/10)
- Functional assessment of gait and range of motion
- Medication review and NSAID usage discussion
- Activity limitation review and cardiovascular precaution screening
Treatment Plan and Notes:
J.M. presented for follow-up concerning persistent left knee pain, described as sharp and throbbing, with daily flare-ups lasting the entire day. He rated the pain 10/10, noting that it worsens with reaching, hanging, prolonged sitting, or standing. He denied any history of recent trauma, falls, or surgical interventions to the knee. Pain is currently self-managed with alternating use of Tylenol and ibuprofen.
Physical examination showed joint tenderness without visible swelling or deformity and limited flexion due to discomfort. Given his history of congestive heart failure and hypertension, extended use of NSAIDs was discouraged due to potential renal and cardiac risks. Referral to orthopedics was initiated for imaging and further evaluation.
A topical NSAID was considered as an alternative for localized relief. The patient was advised to minimize prolonged joint strain and to begin using a knee brace for support during weight-bearing activity. Follow-up is scheduled in three weeks for reassessment (Hsu & Siwiec, 2023).
Patient Log – Entry 8
Client Information:
Patient Initials: D.L.
Age/Gender: 72-year-old Black male
Chief Complaint: Sharp pain and lump in the right groin
Diagnosis:
- Inguinal hernia, unspecified side, without obstruction or gangrene – ICD-10: K40.90
- Groin pain – ICD-10: R10.2 (Mitrousias et al., 2023).
Procedure:
- Abdominal and groin inspection and palpation
- Hernia assessment: location, size, reducibility
- Pain scale and symptom onset review
- Review of emergency department visit and pending surgical consult
- Medication review (NSAID use)
Treatment Plan and Notes:
D.L. presented with right groin pain that began the previous Sunday, accompanied by a palpable lump. He reported being seen in the emergency department two weeks ago and was diagnosed with a hernia requiring surgical repair. He is currently awaiting a urology consultation. Pain is described as sharp and intermittent, with no associated nausea, vomiting, or bowel symptoms.
He is managing the discomfort with over-the-counter ibuprofen. A physical exam confirmed a non-reducible mass in the right inguinal region, consistent with a likely inguinal hernia. No signs of strangulation or acute distress were observed.
The patient was counseled on limiting lifting or straining and was advised to seek immediate care if symptoms worsen. Continued NSAID use was permitted short-term, pending surgical intervention. Urology follow-up and pre-op labs were confirmed for coordination of care.
Patient Log – Entry 9
Client Information:
Patient Initials: A.N.
Age/Gender: 28-year-old Black female
Chief Complaint: Follow-up for management of sickle cell anemia
Diagnosis:
- Sickle-cell anemia without crisis – ICD-10: D57.1
Procedure:
- Review of recent symptoms and frequency of pain episodes
- Vital signs and cardiopulmonary screening (SOB, chest pain, nausea)
- Medication reconciliation: pain and bowel regimen
- Functional assessment and hydration status discussion
- Preventive care review (vaccination, crisis prevention)
Treatment Plan and Notes:
A.N. presented for routine follow-up for sickle cell anemia management. She denied any current shortness of breath, chest pain, nausea, or vomiting. Pain levels were stable, not requiring emergency intervention. Her care team has recommended oxycodone 10mg every six hours when needed for pain and MiraLAX to help with bowel movements.
The patient noted that she has been taking her prescribed medicines and has not had any recent episodes of pain. During the physical exam, the patient’s vitals were stable, and no signs of dehydration or problems with the heart and lungs were found. Her training covered the guidelines on hydration, early symptoms of a problem, and why it is important to rest in between assignments.
It was shown in her medical records that she completed the vaccination for flu and pneumococcal infections. The patient was requested to return after two months, although a quicker follow-up would be required if anything serious happened. It was recommended to collect data on pain and temperatures to notice any changes and guide in handling issues later (Martinez et al., 2020).
Patient Log – Entry 10
Client Information:
Patient Initials: W.B.
Age/Gender: 74-year-old White male
Chief Complaint: Follow-up for hypertension management
Diagnosis:
- Essential (primary) hypertension – ICD-10: I10
- Edema, bilateral lower extremities – ICD-10: R60.0
Procedure:
- Blood pressure measurement and trend review
- Physical exam: assessment of bilateral lower extremity edema
- Cardiopulmonary auscultation (lung sounds clear)
- Medication reconciliation (Amlodipine 5mg daily)
- Symptom review: dizziness, orthostatic symptoms
Treatment Plan and Notes:
W.B. received a yearly hypertension check-up, and the condition was recognized in 2005. It is recommended that he take Amlodipine 5mg by mouth once each day. He stated that he was not having any episodes of dizziness or lightheadedness. At the time of the check-up, his blood pressure was 151/77 mmHg, and there was pitting edema on both of his lower legs.
Lung sounds were clear bilaterally, with no signs of fluid overload in the chest. He reported consistent medication adherence and no recent changes to his lifestyle or diet. The presence of bilateral edema was discussed as a potential side effect of Amlodipine, and the addition of a low-dose diuretic or switching to an alternative calcium channel blocker may be considered.
Lab work was ordered to assess renal function and electrolytes before medication changes. He was advised to elevate his legs when sitting and limit sodium intake. A follow-up appointment was scheduled in two weeks to reassess edema and blood pressure control (Wang et al., 2023).
Patient Log – Entry 11
Client Information:
Patient Initials: B.C.
Age/Gender: 64-year-old White male
Chief Complaint: Chronic middle and lower back pain since 2011
Diagnosis:
- Chronic low back pain – ICD-10: M54.5 (Nicol et al., 2023)
Procedure:
- Comprehensive lumbar and thoracic musculoskeletal exam
- Pain severity and flare-up frequency assessment
- Functional impact evaluation (sitting, standing, walking)
- Review of imaging (prior X-ray), physical therapy, and chiropractic care
- Medication and back brace use confirmation
Treatment Plan and Notes:
B.C. presented for follow-up of chronic back pain since 2011, rated 5/10 daily with flare-ups to 8/10 four times weekly. Pain worsens with prolonged sitting, standing, or walking. He uses a back brace and takes Tylenol and ibuprofen as needed. No history of injury, surgery, or bowel/bladder issues.
The exam showed mild tenderness and reduced flexibility. He continues physical therapy and chiropractic care. The patient was advised to maintain conservative management and follow up in four weeks.
Patient Log – Entry 13
Client Information:
Patient Initials: M.S.
Age/Gender: 54-year-old White male
Chief Complaint: Chronic diarrhea with daily bloating
Diagnosis:
- Functional diarrhea – ICD-10: K59.1
- Abdominal bloating – ICD-10: R14.0 (Oh et al., 2022).
Procedure:
- Detailed GI symptom review and bowel habit evaluation
- Medication reconciliation (Tums, Pepto-Bismol)
- Dietary history and lifestyle factor assessment
- Abdominal exam for tenderness, masses, and bowel sounds
- Referral consideration for GI consultation
Treatment Plan and Notes:
M.S., a machinist, reported chronic diarrhea with 5-6 loose stools daily and bloating. He denied blood in stool and GI surgery. He uses Tums and Pepto-Bismol for relief. His exam was unremarkable.
A food and symptom diary and a trial low-FODMAP diet were recommended. He was advised on hydration and fiber intake. GI referral was suggested if symptoms persist. Follow-up is in three weeks to reassess bowel patterns and treatment response.
Patient Log – Entry 14
Client Information:
Patient Initials: F.T.
Age/Gender: 57-year-old Black male
Chief Complaint: Routine follow-up for chronic medical conditions
Diagnosis:
- Hypertension – ICD-10: I10
- Morbid obesity – ICD-10: E66.01
- Peripheral neuropathy – ICD-10: G62.9
- Multiple myeloma – ICD-10: C90.00
- Post-tonsillectomy status – ICD-10: Z90.89
Procedure:
- Review of chronic disease status and current symptoms
- Medication reconciliation: Lasix, Lisinopril, Jardiance, Atorvastatin
- Cardiovascular and neurological assessment
- Review of specialist coordination with cardiology
- BMI and weight management counseling
Treatment Plan and Notes:
F.T. presented for a routine visit to monitor his chronic conditions. He reports stable blood pressure readings at home, no acute symptoms, and adherence to his current medications. He is followed by cardiology and oncology for hypertension and multiple myeloma, respectively. Peripheral neuropathy symptoms were mild and unchanged.
Vitals were stable; BMI calculation confirmed morbid obesity. The patient was educated on the importance of a balanced, low-sodium, heart-healthy diet and encouraged to participate in low-impact physical activity as tolerated. The need for regular labs and oncology follow-up was reinforced. A scheduled return visit is in one month to reassess BP, lab results, and medication efficacy (Butel-Simoes et al., 2023).
Patient Log – Entry 15
Client Information:
Patient Initials: N.P.
Age/Gender: 33-year-old White male
Chief Complaint: Follow-up for chronic rotator cuff pain
Diagnosis:
- Chronic rotator cuff tear – ICD-10: M75.101 (May & Garmel, 2023).
Procedure:
- Shoulder range of motion and functional assessment
- Pain severity and flare-up frequency review
- Review of home care regimen (ice use, chiropractor)
- Review of medication history (none currently used)
Treatment Plan and Notes:
N.P. presented with chronic shoulder pain from a 2011 rotator cuff tear. He described the pain as achy, rated 5/10, with flare-ups occurring four times weekly. He uses ice for relief and attends chiropractic care. He is currently not on any medication.
A physical exam showed a reduced range of motion and tenderness over the supraspinatus tendon without acute inflammation. He was advised to continue chiropractic sessions and begin rotator cuff exercises. Surgery was deferred. Follow-up is scheduled in six weeks.
Patient Log – Entry 16
Client Information:
Patient Initials: A.K.
Age/Gender: 48-year-old male
Chief Complaint: Follow-up visit for migraine and anemia
Diagnosis:
- Migraine, unspecified, not intractable – ICD-10: G43.909
- Iron deficiency anemia – ICD-10: D50.9
Procedure:
- Headache frequency and trigger review
- Neurological assessment for migraine-related symptoms
- Medication reconciliation: Claritin, Acyclovir, Nasonex, Vitamin D, Iron, Imitrex
- Energy level and anemia-related fatigue screening
- Nutrition and supplement timing discussion
Treatment Plan and Notes:
A.K. presented for a follow-up visit regarding migraines and anemia. He reports experiencing one migraine per month, typically managed with Imitrex at onset. No visual auras, photophobia, or prolonged episodes were noted. The neurologic exam was unremarkable.
He currently takes Claritin, Acyclovir, Nasonex, Vitamin D, iron supplements, and Imitrex as needed. He denied recent dizziness, fatigue, or new symptoms. Counseling was provided on spacing iron supplementation from calcium-containing foods and pairing it with vitamin C for optimal absorption.
He was also advised to maintain hydration, regular sleep patterns, and avoid skipping meals to prevent migraines. A CBC and ferritin panel were ordered to monitor anemia status. Follow-up in one month to review labs and assess ongoing symptom control (Pescador Ruschel & De Jesus, 2024).
Patient Log – Entry 17
Client Information:
Patient Initials: D.B.
Age/Gender: 54-year-old White male
Chief Complaint: Chronic back pain following a fall and fracture in the 1990s
Diagnosis:
- Chronic low back pain – ICD-10: M54.5
- Personal history of healed vertebral fracture – ICD-10: Z87.310
Procedure:
- Lumbar spine assessment and musculoskeletal exam
- Pain intensity and flare-up documentation (6/10 daily, weekly exacerbation)
- Postural assessment and aggravating factor review
- Medication reconciliation (Tylenol and Ibuprofen)
- Screening for red flags (neurological or bowel/bladder symptoms)
Treatment Plan and Notes:
D.B. returned for a follow-up of chronic back pain from a spinal fracture in the 1990s. He reports daily throbbing pain (6/10) with weekly flare-ups from prolonged sitting, standing, or lying. He denies bowel or bladder issues. An exam revealed lumbar tenderness and full range of motion.
The patient was advised on posture, NSAID caution, and movement breaks and was referred to physical therapy. Follow-up is in four weeks to reassess symptoms and consider further evaluation.
References
Butel-Simoes, L. E., Haw, T. J., Williams, T., Sritharan, S., Gadre, P., Herrmann, S. M., Herrmann, J., Ngo, D. T. M., & Sverdlov, A. L. (2023). Established and emerging cancer therapies and cardiovascular system: Focus on hypertension-mechanisms and mitigation. Hypertension (Dallas, Tex.: 1979), 80(4), 685–710. https://doi.org/10.1161/HYPERTENSIONAHA.122.17947
Hsu, H., & Siwiec, R. M. (2023, June 26). Knee osteoarthritis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507884/
Martinez, R. M., Osei-Anto, H. A., & McCormick, M. (2020). Complications of sickle cell disease and current management approaches. In www.ncbi.nlm.nih.gov. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK566466/
May, T., & Garmel, G. M. (2023, June 26). Rotator cuff injury. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547664/
Mitrousias, V., Chytas, D., Banios, K., Fyllos, A., Raoulis, V., Chalatsis, G., Baxevanidou, K., & Zibis, A. (2023). Anatomy and terminology of groin pain: Current concepts. Journal of ISAKOS Joint Disorders & Orthopaedic Sports Medicine, 8(5), 381–386. https://doi.org/10.1016/j.jisako.2023.05.006
Nicol, V., Verdaguer, C., Daste, C., Bisseriex, H., Lapeyre, É., Lefèvre-Colau, M.-M., Rannou, F., Rören, A., Facione, J., & Nguyen, C. (2023). Chronic low back pain: A narrative review of recent international guidelines for diagnosis and conservative treatment. Journal of Clinical Medicine, 12(4), 1685. https://doi.org/10.3390/jcm12041685
Oh, J. E., Chey, W. D., & Spiegel, B. (2022). Abdominal bloating in the United States: Results of a survey of 88,795 Americans examining prevalence and healthcare seeking. Clinical Gastroenterology and Hepatology, 73(78). https://doi.org/10.1016/j.cgh.2022.10.031
Pescador Ruschel, M. A., & De Jesus, O. (2024, July 5). Migraine headache. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560787/
Wang, J.-G., Palmer, B. F., Anderson, K. V., & Sever, P. (2023). Amlodipine in the current management of hypertension. Journal of Clinical Hypertension, 25(9). https://doi.org/10.1111/jch.14709
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Patient Log
Throughout this course, you will also keep a log of patient encounters using Meditrek. AGPCNP students must record at least 100 encounters with GYN patients; FNP students must record at least 125 encounters with patients (100 GYN and 25 OB patients) by the end of this practicum.
The patient log must include the following:
- Client Information
- Diagnosis
- Procedure (Note: Make sure that, as you perform procedures at your practicum site, you also note those on your printed-out Clinical Skills List.)
- Treatment Plan and Notes
Scenario 1
Client is a white male that present with hx of multiple complication. Chronic constipation that began around 7 years ago. Denies hx of stomach surgeries or procedures. Has not had any scans of stomach done previously or seen any GI MD. No hx of coloscopy or EGD procedure.
Patient says that he increases water intake to decrease exacerbation occurrences. Currently has constipation about once per week. Denies blood in stool. Has not had to miss work.
Cardiac MRI was done previously. Report a slow heart rate, in which his baseline was in the 40s. Not currently not on any medications related to heart disease. Denies infections of heart, or heart valve conditions.
Denies missing work due to these conditions. Bilateral shoulder pain in 2016-2017 due to being on crutches. Fell 25ft and broke leg. Landed on shoulder during fall but was not address by MD.
Denies previous surgeries or procedures. Currently doing PT related to shoulders. Shoulders pain is daily, rated 3/10.
Pain aggravating by lifting, describes pain as aching and sharp. Denies taking any OTC medications or prescriptions.
Scenario 2
Client is 45 years old white male
- Follow up visit for anemia, was hospitalized 2 weeks ago for severe anemia, EGD, colonoscopy with biopysy done at hospital.
- S: boating, diarrhea, constipation, stomach pain
- PHM: Anemia, IBS, celiac disease 2024, alcohol and substance abuse, baretts esophagus 2020, Depression, Anxiety
- Medication
- Ferrous sulfate 325mg po BID
- Vitamin D 5000U po daily
- Pantoprazole 40mg po daily
- Pancreactic enzymes
Scenerio 3
Client is 35 years old white male
- Present for lower back pain, pain is worsen with heavy lifting, daily pain, rated 7/10, describes as punching. Daily muscle spasm, Sensation intact bilaterally. Pain affect daily activity. Take longer to do things, Unable to do heavy lifting and work on cars.
- PPHM: scoliosis
- Denies loss of bowel bladder control
- Denies back injury, surgery or procedure, or PT
- MRI done x3 in the past
Scenario 4
Client is 64 years old white male
- Follow up for right arm and right leg pain, pain daily, rated pain 5/10, describes as dull aching.
- PHM: Neuropathy
- Denies any prescriptions or OTC
- Manges pain with stretching.
- Occupation: teacher, driving tractor trailer
Scenario 5
Client is 50 years old white female
- Follow up visit for skin rash and fall
- Skin: rash on upper arm, stomach, itchy. Uses OGTC hydrocortisone with relief
- Lab shows increase liver enzyme
- Fall: fell down 10 stairs, sore in back and ribs intermittent, rated pain 10/10. Take OTC Tylenol 500mg for pain.
- Denies any prescriptions
Patient Logs
Scenario 6
Client is 40 years old white male
- Follow up visit for Hypertension, elevated Blood pressure despite with meds
- PMHL Sleep apnea, Hypertension
- Denies dizziness, lightheadedness
- Medications
- Losartan 10mg po daily
Scenario 7
Client is 59 years old male white male
- Follow up visit for Left knee pain, rated pain 10/10, describes as sharp, throbbing, flare up 7 days a week for 24 hours.
- Aggravate: reaching, hanging, prolong sitting or standing.
- Pain manages with Tylenol, ibuprofen
- Denies fall or injuries, denies procedure or surgery
- PHM, CHF, HTN
Scenario 8
Client is 72 years old black male
- Present for right groin sharp pain, lump noted. Pain started last Sunday
- Last seen in ED 2 weeks ago, need hernia repair.
- Have appointment for urology consultation
- Take Ibuprofen for pain
Scenario 9
Client is 28 years old black female
- Follow up appointment for sickle cell anemia
- Denies SOB, chest pain, Nausea, vomiting
- Medication: oxycodone 10mg po Q 6 hrs. PRN, MiraLAX
Scenario 10
Client is 74 years old white male
- Follow up appointment for hypertension
- PHM: Hypertension 2005
- Denies Dizziness, Lightheadedness
- Noted edema 2+ bilateral lower extremities, lung sound clear, today BP 151/77
- Medication: Amlodipine 5mg po daily
Scenario 11
Client is 64 years old white male
- Follow up for middle lower back pain from 2011, rated 5/10 pain daily, describes as sore, achy.
- Aggravation: prolong sitting, standing, walking
- Flare up 4 times a week lasting 24-48 hours, pain severity 8/10
- Have a back brace,
- Denies injuries, procedure or surgery
- X-ray done previously
- Currently doing PT and chiropractor
- Medication: Tylenol and Ibuprofen
- Denies loss of bowel and bladder control
Scenario 13
Client is 54 years old white male
- Follow up visit for chronic diarrhea
- 5-6 loose stools daily, bloating
- Denies bloody stool
- Denies GI surgery
- Medication: tums, Pepto-Bismol
- Occupation: machinist
Scenario 14
- Client is 57 years old black male
- Routine visit
- PHM: Hypertension, morbid obesity, neuropathy, tonsillectomy, multiple myeloma
- Medications: Lasix, Lisinopril, Jardiance, Atorvastatin
- Follow by Cardiologist
Scenario 15
- Client is 33 years old white male
- Follow up visit for torn rotator cuff from 2011
- Rated daily pain 5/10 pain describes as achy
- Flare up 4 x a weeks
- Use ice for pain
- Currently doing chiropractor
- No medications
Scenario 16
- Client is 48 years old male
- Follow up visit for migraine, anemia
- 1 episode of migraine x1 a month
- Medication: Claritin, Acyclovir, Nasonex, Vit D, Iron, Imitrex
Scenario 17
Client is 54 years old white male
- Follow up visit for back pain
- fall and fracture back in 1990s
- Daily pain 6/10, throbbing pain. Flare up 1 time a week
- Denies loss of bowel and bladder control
- Aggravate: prolong lying, standing, sitting
- Medication: Ibuprofen, Tylenol