Nursing Service Line for The Diabetes Management and Teaching Program
Proposed Nursing Service Idea
The proposed nursing service line is the Diabetes Management and Teaching Program, to be managed by a nurse and established in Cypress, Texas, at a local community health center. The goal of this service is to deliver patient-specific diabetes education for adults over 18 years of age diagnosed with type 1 or type 2 diabetes. The service topics will include insulin injections, procedures for blood glucose measurement, diet comprehension, and medication regimens to increase glycemic control and minimize complications (Romero-Castillo et al., 2022). These services will be provided individually and in groups, face to face, and via telehealth to accommodate convenience. The nurse-led care model promotes strong patient engagement and focuses on nurse-patient relationships and patient self-management of the disease. This program recognizes the fact that Harris County has a high rate of diabetes, and patient educational services targeting minority groups are scarce.
Some of the leadership competencies that will enhance the success of this service include transformational leadership, which will ensure staff understand the service’s mission to educate patients and improve the innovative education provision. Servant leadership will help the nurses consider the interests of patients and employees while fostering togetherness and confidence (Canavesi & Minelli, 2021). Situational leadership will also be significant in relating to the dynamics of the teams and flexibly meeting patients’ needs (Wang et al., 2024). To ensure this diverse and effective care model is implemented, the care team shall comprise nurse practitioners, registered nurses, a registered dietician, and certified diabetes nurse educators. The team will also include administrative and community health staff to ensure patients are followed up on to meet all their needs (Torti et al., 2022). All members will participate in teamwork to ensure they offer diabetes education and consultation based on national and practice standards guidelines.
Importance
The Diabetes Management and Teaching service line is focused on only adults who are 18 years and above living in Cypress, Texas, in Harris County, and those newly diagnosed with type 1 or type 2 diabetes or those who lack adequate skills and knowledge in managing their condition. The state’s prevalence rate of diabetes is around 12% in Harris County, which is higher than the national rate, meaning that more intervention is required (Peralez, 2023). Some difficulties include uneducated patients, no access to follow-up treatment, and cultural practices hampering effective glucose management, insulin administration, and adherence to a proper diet. This nurse-led service bridges this gap because structured diabetes education meets healthcare priorities such as the Triple Aim: better population health, improved patient experience, and decreased cost (Dailah, 2024). Diabetes Self-Management Education and Support (DSMES) has been proven to reduce complications and hospitalization, and its services are reportable and reimbursable under chronic care management (CCM) codes (Powers et al., 2020). The program is relevant to both the patient and system levels for value-based, effective, and sustainable care.
Table 1: Market Analysis
| Target Population | Potential Referral Bases | Potential Competitors |
| Adults aged 18 years and older residing in Cypress, Texas (Harris County) with a diagnosis of type 1 or type 2 diabetes, especially those newly diagnosed or struggling with insulin use, blood sugar monitoring, and dietary management. | – Primary care providers (PCPs)
– Endocrinologists – Hospital discharge planners – Urgent care centers – Federally Qualified Health Centers (FQHCs) – School and workplace health clinics – Local public health programs (e.g., Harris County Public Health) – Employer wellness and chronic care programs |
– Memorial Hermann Cypress Hospital – Diabetes Education Program
– HCA Houston Healthcare North Cypress – Outpatient services – Houston Methodist Willowbrook – DSMES program – Virta Health, Omada Health, and Livongo – digital/telehealth diabetes management platforms offering remote coaching and app-based education |
Table 2: SWOT Analysis
| Strengths | Weaknesses | Opportunities | Threats |
| 1. On-site clinical space available within a community health facility in Cypress, TX | 1. Need to recruit and train additional staff certified in diabetes education (CDNEs) | 1. High diabetes prevalence in Harris County creates a strong demand for diabetes education and support services. | 1. Patient noncompliance with insulin or lifestyle modifications may reduce the effectiveness of services. |
| 2. Nurse-led, culturally responsive education model based on ADA and CMS guidelines. | 2. Limited initial funding for equipment, technology, and marketing. | 2. Potential partnerships with local PCPs, FQHCs, and public health agencies for referrals and outreach. | 2. Delays or denials in insurance reimbursement for DSMES or CCM services. |
| 3. Multilingual staff to meet the needs of the diverse Harris County population. | 3. Public awareness of the new service may be low during the early launch. | 3. Grant funding opportunities from agencies such as HRSA, CDC, and Texas DSHS for chronic disease education programs. | 3. Strong competition from local hospital-based programs and virtual diabetes management platforms like Virta or Omada. |
| 4. Integration with the existing EHR platform facilitates provider documentation and coordination. | 4. A small initial team size may limit scalability and increase staff workload early on. | 4. Alignment with national health priorities, including value-based care initiatives and chronic disease prevention strategies. | 4. Public health emergencies (e.g., COVID-19 resurgence) may disrupt in-person visits and patient participation. |
SWOT Analysis Results
The program’s internal strengths strongly align with external opportunities in Cypress, Texas. Having a clinic at the workplace eliminates the costs of setting up infrastructures and reduces the time to set up the service. This aligns with the potential of meeting the high diabetes need in Harris County, especially among the vulnerable population. Utilizing the nurse-led, culturally sensitive approach increases the level of patient trust while supporting the performance of value-based healthcare goals. Besides, a multilingual staff also ensures that a large population, predominantly Hispanic and black residents, benefit from the program (Brach & Fraser, 2022). These are also meaningful to develop strong strategic alliances with other local PCPs, FQHCs, and public health departments, which can contribute to constructing logical referral streams. Moreover, it supports the process of documentation and billing of patients incorporated in the electronic health record (EHR). Thus, the program is riveted for grant funding and chronic care reimbursement under CMS. Altogether, these strengths contribute to the ability to develop the program and meet the needs of society at the same time.
Program strengths will also play a significant role in reducing external threats. One sharp risk is patient nonadherence due to low health literacy or cultural misunderstanding. The team of multilingual and culturally sensitive instructors will further reduce the current situation by gaining the patient’s trust and providing individualized education (Haque et al., 2023). In addition, it is possible to make follow-up phone calls and telehealth visits to ensure patients follow through with the information given and their progress. Regarding insurance reimbursement, necessary staff will be trained in using DSMES and CCM for the use of EHRs to ensure efficiency in coding, which enhances the timely filing of claims. Potential threats from other online diabetes platforms and hospital-based programs are addressed by promoting patient-centered and community-oriented care.
Several internal weaknesses, such as staffing shortages and limited start-up funding, can be improved by leveraging external opportunities. The funding from HRSA, CDC, and the Texas DSHS may help support salaries, technology, and training. The intern support can be obtained through partnerships with the schools of nursing, which ensures a ready source of workforce. Thus, the high local incidence of diabetes makes the service appealing to local PCPs, implying more patients and revenue (Dragomanovich & Shubrook, 2021). Materials provided by public health organizations in the form of education and bilingual toolkits are effective ways of reducing development costs. These solutions are in line with the healthy community aims and objectives in the long run and are sustainable. Also, offering group education sessions will ease the staff’s workload and cover many patients at once. Thus, by applying the existing resources, the program should be able to manage the identified weaknesses and strengthen growth.
The program will implement strategic outreach and flexible care models to reduce weaknesses while mitigating threats. Marketing collaborations with churches, schools, and clinics can resolve low community awareness. Increased awareness and confidence will be created through free diabetes tests and multilingual handouts (Sękowski et al., 2022). To avoid staff burnout, managing demand will be done by a small team incorporating group classes and a combination of telehealth. For such interruptions to public health, such as the current pandemic, the program will ensure the offering of online courses. Technology access issues would be managed by offering patient onboarding services. Staff training will continue to ensure that all the bills are correct, thus eliminating cases of denied claims.
Table 3a: Cost-Benefit Analysis – The Organization
| Logical Costs | Logical Benefits |
| Start-up costs: The initial investment is in diabetes education materials, glucose monitors, office furniture, and renovation of teaching space. | Improved community relations through outreach, prevention, and commitment to patient-centered care. |
| Accreditation fees: The cost of American Diabetes Association (ADA) recognition or AADE certification to qualify for DSMES billing. | Reduced readmission rates and hospital utilization due to better patient self-management and prevention of complications. |
| Liability insurance: Increased insurance premiums to cover new services, procedures, and staff roles introduced in the program. | Creation of a new service line generating revenue through DSMES and CCM reimbursement codes. |
Table 3b: Cost-Benefit Analysis – Day-to-Day Operations
| Logical Costs | Logical Benefits |
| Salary costs: Wages for one NP, two RNs, and one dietician delivering direct diabetes education and patient support. | New revenue source via reimbursable CPT codes, CCM billing, and potential for grant-supported outreach programs. |
| Monthly bills: Recurring costs for rent, electricity, water, internet, and telephone services at the education site. | Continuity of care through scheduled education sessions, follow-ups, and improved treatment adherence. |
| Supplies and teaching materials: Cost of glucose testing kits, printed handouts, meal planning tools, and visual aids for patient use. | Improved patient engagement and empowerment, resulting in better self-care and treatment outcomes. |
| Technology and software: Subscriptions for telehealth platforms, billing software, electronic health records, and secure messaging. | Efficient data documentation, patient tracking, and care coordination with external providers and insurance companies. |
| Marketing and outreach: Expenses for flyers, health fair booths, community campaigns, and referral materials. | Increased patient volume through awareness-building, community engagement, and improved relationships with referral sources. |
Table 4: Risk Assessment and Strategies
| Risks | Possible Results of the Risk | Strategies for Minimizing the Risks |
| 1. Patient noncompliance with diabetes education plans | Poor glycemic control increased ER visits and reduced the effectiveness of the service line. | Implement structured follow-ups via phone calls and telehealth check-ins. Use motivational interviewing to promote patient adherence. |
| 2. Limited staffing or staff turnover | Missed appointments, care delays, and patient dissatisfaction. | Offer retention bonuses, career development, and cross-train staff—partner with nursing schools for intern placement and workforce pipeline. |
| 3. Reimbursement delays or denials from insurers | Financial strain on the program, disrupted operations, and budget shortfalls. | Train staff on DSMES and CCM billing codes, use EHR-integrated billing software, and regularly audit submitted claims. |
| 4. Public health emergencies (e.g., COVID-19 surges) | Suspension of in-person services
Decreased patient access and engagement |
Develop a hybrid service model with both virtual and in-person options—train staff to pivot quickly to telehealth platforms as needed. |
| 5. Low community awareness of the program | Low enrollment, missed opportunities for impact, and lack of referrals. | Conduct targeted outreach via local clinics, churches, and employers. To increase visibility, host free screenings and bilingual education events. |
Financial Projections for the First Year
The Diabetes Management and Teaching service line will take place from Monday to Friday from 8 am to 5 pm for individuals with diabetes and will provide DSME and CCM. Service revenues will be income from Medicare, Medicaid, and other insurance using the Current Procedural Terminology (CPT) code of 98960 (individual DSME), 98961 (group DSME), and 99490 (CCM). The cost of a regular one-on-one DSME session is $120, while the group session is $80 per participant. Every patient will undergo at least two educations per quarter, including an individual consultation and a group or individual review. Others will be in the form of monthly charges per CCM patient with existing chronic illnesses.
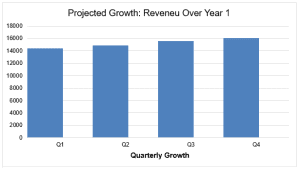
Financial projections are calculated on this calculated volume with an annual growth of 4% for each quarter starting 2nd quarter, which is a typical trend in the healthcare industry for new services. The program will begin with a pool of 60 new patients in Q1. This number is expected to grow by 4% in the subsequent quarters, depending on the physician recommendations, marketing campaigns, and community awareness. Therefore, 62 patients in Q2, 65 in Q3, and 67 in Q4 are astoundingly incurred due to hospitalization. Supposing that each patient participates in two sessions per quarter at the rate of $120 per session, the anticipated quarterly revenue is:
Q1: 60 patients × 2 sessions × $120 = $14,400
Q2: 62 patients × 2 × $120 = $14,880
Q3: 65 patients × 2 × $120 = $15,600
Q4: 67 patients × 2 × $120 = $16,080
The organization’s annual revenue is estimated at $60,960 for the first year of operation. These calculations do not include group education income, monthly CCM codes generating $40-$60 per patient monthly, and the possibility of grants from HRSA and CDC for chronic care programs. When approached with a well-planned patient volume expansion and service line development, the clinicians should be able to make the service line clinically necessary and financially feasible in its first year of operation.
Revenue Graph the First Year
Service Payers
The funding of the Diabetes Management and Teaching nursing service line shall come from Medicare, Medicaid, private insurance, and public health grants, as well as charges from the patients. It is required that Medicare and Medicaid cover DSME and CCM using codes like 98960 and 99490, as it is essential for older people and the low-income citizens of Cypress. These services are also supported by private insurers like Blue Cross Blue Shield, Aetna, and UnitedHealthcare, particularly under the value-based care models. More funding from the Health Resources and Services Administration (HRSA) and the Centers for Disease Control and Prevention (CDC) should be sought to support the efforts toward sustaining the program financially (Whitman et al., 2022). However, the service will provide relatively inexpensive services to uninsured or underinsured patients; at the same time, such patients will pay enough to subsidize the service cost. Ideally, this diverse payer mix provides long-term sustainable funding, better program accessibility for patients, and fair payer contribution for patients with diabetes.
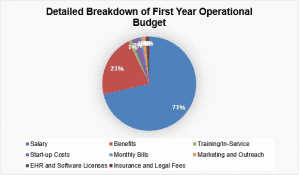
Table 5a: Operational Expense Budget
| Personnel Expenses | Description and Cost ($) of Each Type of Expense |
| 1. Salary | Nurse Practitioner ($115,000) + 2 RNs ($160,000) + 1 Dietician ($70,000) = $345,000 |
| 2. Benefits | 30% of $345,000 = $103,500 |
| 3. Other | Staff onboarding and continuing education = $5,000 |
Table 5b: Operational Expense Budget
| Other-than-Personnel (OTP) Expenses | Description and Cost ($) of Each Type of Expense |
| 1. Start-up Costs | Renovation, furniture, glucose monitors, demo kits, posters, and whiteboards = $15,000 |
| 2. Monthly Bills | Rent: $2,000/month
Utilities: $500/month Internet: $150/month Supplies: $400/month Total: $3050 |
| 3. Marketing and Outreach | Social media ads, flyers, referral materials, website hosting = $6,000 |
| 4. EHR and Software Licenses | Subscription for EHR, telehealth, secure messaging, billing platform = $3,500 |
| 5. Insurance and Legal Fees | Liability insurance, license renewals, and legal consulting = $2,500 |
Budget Pie Chart (one chart)
Table 6: Key Performance Indicators (KPIs)
| Service Plan KPIs | How will the KPI Data be Measured | Frequency of Evaluation | How will the KPI be Used for Future Decision-Making |
| One Structure KPI: Staff-to-Patient Ratio | Daily appointment schedules and EHR records will track how many patients each staff member sees. | Evaluate quarterly | Data will be used to determine when staffing levels need to be increased to maintain safe, high-quality care delivery. |
| One Process KPI: Number of Referrals to Service | Recorded on intake forms and referral logs from providers | Evaluate quarterly | If referral rates drop, marketing efforts and provider engagement strategies will be adjusted to boost referrals. |
| One Outcome KPI: Patient Satisfaction | Patients will automatically receive a survey link via email following each appointment. | Evaluate quarterly | Satisfaction scores will guide improvements in care delivery, staff communication, and patient education strategies. |
Measurement and Frequency of KPIs
Structure KPI – Staff-to-Patient Ratio
This KPI will be measured by reviewing daily appointment schedules and staffing assignments within the EHR system. Reports will be generated to calculate how many patients each nurse or educator sees daily. This data will be compiled and analyzed quarterly to determine staff workload balance and resource adequacy.
Process KPI – Number of Referrals to the Service
Referral counts will be measured by tracking intake forms and referral logs submitted by primary care providers and community partners. These logs will be maintained in a secure tracking database. Reports will be reviewed quarterly to evaluate provider engagement and visibility of the service line.
Outcome KPI – Patient Satisfaction
Satisfaction will be measured by emailing a post-visit survey to patients through the clinic’s patient engagement platform after each appointment. Survey completion data will be automatically collected and compiled in the EHR system. Satisfaction trends will be analyzed quarterly to assess the patient experience and identify areas for improvement.
KPI Data Analysis and Future Decision-Making
The data collected from each KPI will be analyzed quarterly to evaluate trends and guide future strategic and operational decisions. For the structure KPI (staff-to-patient ratio), quarterly reports will be used to assess whether current staffing levels support patient demand. If the ratio becomes too high (for instance, too many patients per educator), this will prompt hiring additional staff or reallocating duties to maintain care quality. For the process KPI (referral volume), declining or stagnant referral trends may indicate reduced visibility or weakened provider partnerships. In such cases, leadership will consider ramping up community outreach, improving communication with referring physicians, or revisiting marketing strategies. For the outcome KPI (patient satisfaction), survey responses will be categorized and reviewed for trends. If patients consistently report dissatisfaction with educational materials, staff interaction, or wait times, targeted training or workflow adjustments will be made to improve service quality and overall patient experience.
System-level Improvement
A key system-level strategy to support continuous improvement is the implementation of quarterly interprofessional performance review meetings. These meetings will bring together all involved staff, including nurse educators, the NP, dieticians, front-office support, and administrative leadership. During these sessions, KPI data will be discussed to know more about the challenges and strategies that have been applied and to design an action plan. It also improves students’ responsibility and oversight, enhancing interprofessional cooperation, shared decision-making, and quality improvement (Nurchis et al., 2022). When incorporated into the organization’s functioning, this approach to structuring the review process will ensure that the team stays mindful of its performance objectives as it responds to live situations concerning service delivery.
Table 7: Tasks and Timelines
| Task | One Task Owner by Title | Frequency of Task Status Meetings | Timeline Before Opening Service |
| 1. Finalize service line business plan and secure approval | Nurse Administrator | Week 1–2 | Weekly |
| 2. Hire and onboard staff (NP, RNs, dietician, admin support) | Human Resources Director | Week 2–4 | Twice weekly until positions are filled |
| 3. Train staff on DSME protocols and documentation requirements | Clinical Nurse Educator | Week 3–5 | Weekly |
| 4. Set up physical space (furnishing, signage, educational boards) | Facilities Manager | Week 3–6 | Bi-weekly |
| 5. Purchase and install medical and teaching equipment | Procurement Officer | Week 3–5 | Weekly |
| 6. Develop and translate patient education materials | Dietician and Cultural Liaison Nurse | Week 4–6 | Weekly |
| 7. Configure EHR templates and billing codes for DSMES and CCM | Health IT Specialist | Week 4–5 | Weekly |
| 8. Establish referral workflow with primary care providers | Program Coordinator | Week 5–6 | Weekly |
| 9. Launch a targeted marketing campaign to the community and providers | Outreach and Communications Manager | Week 6–7 | Weekly |
| 10. Conduct final pilot test and quality check before going live | Quality Improvement Officer | Week 7–8 | Twice during the final week |
Executive Summary
Proposed Nursing Service Idea
This proposal elaborates on the creation and operation of a Diabetes Management and Teaching nursing service line in Cypress, Texas (Harris County). The service is aimed at offering condition-focused, results-based teaching to clients aged 18 years and above with type 1 or type 2 diabetes (Castillo-Merino et al., 2023). Services will focus on diabetes self-management, including insulin use, blood sugar monitoring, dietary education, and chronic care coordination. The goal is to improve health outcomes, reduce complications, and support the community through accessible, culturally responsive care.
Market Analysis
A detailed market analysis identified a high need in Harris County, where the adult diabetes prevalence rate is 12%, exceeding national averages. The target population includes adults 18 and older, with referrals expected from local primary care providers, federally qualified health centers, and hospitals. Potential competitors include hospital-based DSME programs and online platforms, though the proposed service’s in-person, nurse-led approach offers unique value.
SWOT Analysis
The SWOT analysis revealed key strengths, including a dedicated nurse-led model, EHR integration, and multilingual staff. Opportunities include federal grant eligibility, payer reimbursement, and high community demand. Weaknesses such as initial staffing limitations and funding constraints will be addressed through phased implementation and grant applications (Hanson et al., 2022). Billing training and patient follow-ups will mitigate threats like reimbursement delays and patient noncompliance.
Cost-Benefit Analysis
A cost-benefit analysis projected first-year operational costs at $517,100, with revenue estimated at $60,960 (conservatively). Investment in this early phase, however, may not fully fund the business, and hence, it is plausible to rely on reimbursement by payers, grants, and increased patient access. Some of the benefits associated with the suggested solution include low chances of readmission, optimum patient health, and increased community satisfaction.
Risk Assessment
The risk assessment identified five key risks: staffing shortages, reimbursement issues, and low public awareness. Each risk is associated with a risk management plan comprising cross-coverage, EHR-integrated billing, or outreach to the community. Together, this service line addresses population health and performance goals and initiatives in value-based care.
References
Brach, C., & Fraser, I. (2022). Reducing disparities through culturally competent health care. Quality Management in Health Care, 10(4), 15–28. https://doi.org/10.1097/00019514-200210040-00005
Canavesi, A., & Minelli, E. (2021). Servant leadership and employee engagement: A qualitative study. Employee Responsibilities and Rights Journal, 34(4), 413–435.
Castillo-Merino, Y. A., Ospina-Ayala, C., Esquivel-Garzón, N., Rodríguez-Acelas, A. L., & Cañon-Montañez, W. (2023). educational interventions in adults with type 2 diabetes mellitus in primary health care settings. A scoping review. Investigacion Y Educacion En Enfermeria, 41(2), e15. https://doi.org/10.17533/udea.iee.v41n2e15.
Dailah, H. G. (2024). The influence of nurse-led interventions on diseases management in patients with diabetes mellitus: A narrative review. Healthcare, 12(3), 352. https://doi.org/10.3390/healthcare12030352
Dragomanovich, H. M., & Shubrook, J. H. (2021). Improving cultural humility and competency in diabetes care for primary care providers. Clinical Diabetes, 39(2), cd200063. https://doi.org/10.2337/cd20-0063
Hanson, K., Brikci, N., Erlangga, D., Alebachew, A., De Allegri, M., Balabanova, D., Blecher, M., Cashin, C., Esperato, A., Hipgrave, D., Kalisa, I., Kurowski, C., Meng, Q., Morgan, D., Mtei, G., Nolte, E., Onoka, C., Powell-Jackson, T., Roland, M., & Sadanandan, R. (2022). The Lancet Global Health Commission on financing primary health care: Putting people at the centre. The Lancet Global Health, 10(5), 715–772. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(22)00005-5/fulltext
Haque, M. Z., Faten Mohamed Ahmed, Khan, S., Muntakim, M., Khan, H. J., Azam, M., & Husain, M. (2023). Diabetes management and culturally sensitive care: An approach to care for Bangladeshi patients. Clinical Medicine Insights, 16. https://doi.org/10.1177/11795514231210139
Nurchis, M. C., Sessa, G., Pascucci, D., Sassano, M., Lombi, L., & Damiani, G. (2022). Interprofessional collaboration and diabetes management in primary care: A systematic review and meta-analysis of patient-reported outcomes. Journal of Personalized Medicine, 12(4), 643. https://doi.org/10.3390/jpm12040643
Peralez, I. (2023). Designing learning programs for a multigenerational workforce – Bookboon learning. Bookboonlearning.com. https://doi.org/10/2021/08
Powers, M. A., Bardsley, J. K., Cypress, M., Funnell, M. M., Harms, D., Hess-Fischl, A., Hooks, B., Isaacs, D., Mandel, E. D., Maryniuk, M. D., Norton, A., Rinker, J., Siminerio, L. M., & Uelmen, S. (2020). Diabetes self-management education and support in adults with type 2 diabetes: A consensus report of the American Diabetes Association, the Association of Diabetes Care and Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care, 43(7), 1636–1649. https://doi.org/10.2337/dci20-0023
Romero-Castillo, R., Pabón-Carrasco, M., Jiménez-Picón, N., & Ponce-Blandón, J. A. (2022). Diabetes management after a therapeutic education program: A qualitative study. Healthcare, 10(8), 1375. https://doi.org/10.3390/healthcare10081375
Sękowski, K., Grudziąż-Sękowska, J., Pinkas, J., & Jankowski, M. (2022). Public knowledge and awareness of diabetes mellitus, its risk factors, complications, and prevention methods among adults in Poland—A 2022 nationwide cross-sectional survey. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.1029358
Torti, J. M. I., Szafran, O., Kennett, S. L., & Bell, N. R. (2022). Interprofessional care of patients with type 2 diabetes mellitus in primary care: Family physicians’ perspectives. BMC Primary Care, 23(1). https://doi.org/10.1186/s12875-022-01688-w
Wang, X., Liu, Y., Peng, Z., Li, B., Liang, Q., Liao, S., & Liu, M. (2024). Situational leadership theory in nursing management: A scoping review. BMC Nursing, 23(1). https://doi.org/10.1186/s12912-024-02582-9
Whitman, A., De Lew, N., Chappel, A., Aysola, V., Zuckerman, R., & Sommers, B. (2022, April 1). Addressing social determinants of health: Examples of successful evidence-based strategies and current federal efforts. ASPE.hhs.gov. https://aspe.hhs.gov/sites/default/files/documents/e2b650cd64cf84aae8ff0fae7474af82/SDOH-Evidence-Review.pdf
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Nursing Service Line for The Diabetes Management and Teaching Program
Competencies
7064.1.1 : Determine Leadership Skills and Approaches
Nursing Service Line for The Diabetes Management and Teaching Program
The learner determines the effective leadership skills and approaches required to navigate a diverse staff in a changing healthcare environment.
7064.1.2 : Create Communication and Change Management Plans
The learner creates communication and change management plans to foster a culture of innovation.
7064.1.3 : Analyze Data for Progress Indicators
The learner analyzes data to measure progress in meeting organizational performance indicators in complex healthcare systems.
7064.1.4 : Determine Support Factors for Interprofessional Teams
The learner determines system-level factors necessary to support and empower interprofessional teams.
7064.1.5 : Validate Performance Measurement
The learner validates key performance indicators to measure the impact of nursing care on patient and population outcomes.
7064.1.6 : Propose Strategic Plan
The learner proposes a strategic business plan to start a nurse-managed practice.
Nurse leaders have many opportunities to develop innovative organizational projects. For this assessment, you will assume the role of a nurse leader who is interested in starting a new nursing service line. The proposed nursing service should meet the following criteria:
• can be any service that meets a demonstrated patient health need
• contains a major nurse-led component
• has the ability to generate revenue that is sustainable
Here are a few examples of the diverse opportunities for organizational growth:
• physical and mental health services provided through wellness centers
• vascular access care services
• diagnosis-specific support clinics
• nurse-directed medical day care services
• wound care services
• diabetes management services
• care coordination for supervising and evaluating interdisciplinary care services
• home health and hospice services
These varied examples demonstrate the impact that nurse leaders have on healthcare delivery.
In this task, you will use the attached “Nursing Service Line” template to develop your brief. Using an interprofessional focus, you will explain the need for the service and present the results of various business analyses to determine the feasibility of starting the new service line within an organization. Use the information provided in the course to determine an area of service and to complete the analyses required in this assessment.