Synthesis and Recommendations Tool
Appendix H
| EBP Question:
|
|||
| Strength | Number of Sources (Quantity) | Synthesized Findings With Article Number(s)
(This is not a simple restating of information from each individual evidence summary—see directions) |
|
| Level | Overall Quality Rating
(Strong, good, or low) |
||
| Level I
§ Experimental studies |
Strong | 2 | Articles [3] (Dietermann et al., 2021) and [6] (McHugh et al., 2021) provided high-quality quantitative evidence demonstrating that improved nurse-to-patient ratios result in statistically significant reductions in patient mortality, hospital readmissions, and medication errors. McHugh et al. (2021) examined the impact of nurse staffing legislation using panel data and prospective hospital outcomes, while Dietermann et al. (2021) applied multilevel regression modeling across diverse healthcare facilities to highlight nursing-sensitive outcomes. Both studies offer high internal validity and large sample sizes, making their findings generalizable and actionable for policy and practice: Synthesis and Recommendations Tool.
|
| Level II
§ Quasi-experimental studies
|
Good
|
3 | Articles [2] (Banda et al., 2022), [4] (Juvé-Udina et al., 2025), and [7] (Moriwaki et al., 2025) provide supportive quantitative findings linking high nursing workloads with adverse events such as increased medication errors, missed care, and patient safety concerns. Juvé-Udina et al. (2025) conducted a patient-unit level analysis, Moriwaki et al. (2025) analyzed administrative data, and Banda et al. (2022) explored the perspectives of ICU nurses. Despite some variation in methodology, all three studies converge on the conclusion that staffing shortages compromise timely care delivery and increase error likelihood. |
| Level III
§ Nonexperimental, including qualitative studies
|
Good | 5 | Articles [1] (Ashour et al., 2025), [5] (Li et al., 2024), [8] (Nantsupawat et al., 2021), [9] (Witczak et al., 2021), and [10] (Ziemek et al., 2024) represent qualitative and mixed-method evidence emphasizing how chronic understaffing negatively impacts nurse well-being, communication efficiency, and patient-centered care. Common themes include increased burnout, rationing of care, staff disengagement, and impaired teamwork. These studies underscore the human and systemic dimensions of staffing challenges, providing contextual richness and insight for leadership interventions. |
| Level IV
§ Clinical practice guidelines or consensus panels |
|
||
| Level V
§ Literature reviews, QI, case reports, expert opinion
|
|
||
| Where does the evidence show consistency? |
| There is consistent evidence across all levels of quantitative, qualitative, and mixed methods that improving nurse-to-patient ratios leads to better patient outcomes. Multiple studies confirmed reductions in adverse events, including medication errors, pressure ulcers, missed care, and mortality. Both Level I experimental studies and Level III qualitative evidence highlight that staffing is a direct determinant of safety and quality in care delivery. |
| Where does the evidence show inconsistency? |
| Inconsistencies arise mainly in the qualitative studies. While some emphasized the psychological impact of staffing (such as burnout and job dissatisfaction), others focused more on operational consequences like communication breakdowns. Furthermore, the studies varied in terms of sample sizes, settings (ICU versus general wards), and measurement tools, making direct comparisons complex. These inconsistencies, however, do not diminish the central finding that inadequate staffing compromises care. |
| Best evidence recommendations (taking into consideration the quantity, consistency, and strength of the evidence): |
| Healthcare organizations should prioritize nurse staffing reforms by adopting ratio policies that match patient acuity and volume. Monitoring tools should be implemented to evaluate nurse workload and missed care occurrences. Policies that incentivize retention, enhance communication, and reduce burnout will not only improve nurse satisfaction but also enhance patient safety outcomes. This multi-faceted strategy should be tailored to both acute and chronic care settings.
|
| Based on your synthesis, select the statement that best describes the overall characteristics of the body of evidence. |
| ☐ Strong & compelling evidence, consistent resultsà Recommendations are reliable; evaluate for organizational translation.
☒ Good evidence & consistent resultsà Recommendations may be reliable; evaluate for risk and organizational translation. ☐ Good evidence but conflicting resultsà Unable to establish best practice based on current evidence; evaluate risk, consider further investigation for new evidence, develop a research study, or discontinue the project. ☐ Little or no evidenceà Unable to establish best practice based on current evidence; consider further investigation for new evidence, develop a research study, or discontinue the project. |
References
Ashour, H. M. A.-A. A., Abou Hashish, E. A. O., & Awad, N. H. A. (2025). From awareness to action: Investigating the impact of big-five teamwork model awareness on rationing of nursing care and patient-centered care. BMC Nursing, 24(1). https://doi.org/10.1186/s12912-025-02711-y
Banda, Z., Simbota, M., & Mula, C. (2022). Nurses’ perceptions on the effects of high nursing workload on patient care in an intensive care unit of a referral hospital in Malawi: A qualitative study. BMC Nursing, 21(1). https://doi.org/10.1186/s12912-022-00918-x
Dietermann, K., Winter, V., Schneider, U., & Schreyögg, J. (2021). The impact of nurse staffing levels on nursing-sensitive patient outcomes: A multilevel regression approach. The European Journal of Health Economics, 22(5), 833–846. https://doi.org/10.1007/s10198-021-01292-2
Juvé-Udina, M.-E., Adamuz, J., González-Samartino, M., Tapia-Pérez, M., Jiménez-Martínez, E., Berbis-Morello, C., Polushkina-Merchanskaya, O., Zabalegui, A., & López-Jiménez, M.-M. (2025). Association between nurse staffing coverage and patient outcomes in a context of prepandemic structural understaffing: A patient‐unit‐level analysis. Journal of Nursing Management, 2025(1). https://doi.org/10.1155/jonm/8003569
Li, G., Wang, W., Pu, J., Xie, Z., Xu, Y., Shen, T., & Huang, H. (2024). Relevant factors affecting nurse staffing: A qualitative study from the perspective of nursing managers. Frontiers in Public Health, 12. https://doi.org/10.3389/fpubh.2024.1448871
McHugh, M., Aiken, L., Sloane, D., Windsor, C., Douglas, C., & Yates, P. (2021). Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: A prospective study in a panel of hospitals. The Lancet, 397(10288), 1905–1913. https://doi.org/10.1016/S0140-6736(21)00768-6
Moriwaki, M., Tanaka, M., Kakehashi, M., Koizumi, M., Horiguchi, H., & Hayashida, K. (2025). Influence of nursing time and staffing on medication errors: A cross-sectional analysis of administrative data. Nursing Reports, 15(1), 12. https://doi.org/10.3390/nursrep15010012
Nantsupawat, A., Poghosyan, L., Wichaikhum, O., Kunaviktikul, W., Fang, Y., Kueakomoldej, S., Thienthong, H., & Turale, S. (2021). Nurse staffing, missed care, quality of care and adverse events: A cross‐sectional study. Journal of Nursing Management, 30(2), 447–454. https://doi.org/10.1111/jonm.13501
Witczak, I., Rypicz, Ł., Karniej, P., Młynarska, A., Kubielas, G., & Uchmanowicz, I. (2021). Rationing of nursing care and patient safety. Frontiers in Psychology, 12(1), 676970. https://doi.org/10.3389/fpsyg.2021.676970
Ziemek, J., Hoge, N., Woodward, K. F., Doerfler, E., Bradywood, A., Pletcher, A., Flaxman, A. D., & Iribarren, S. J. (2024). Hospital personnel perspectives on factors influencing acute care patient outcomes: A qualitative approach to model refinement. BMC Health Services Research, 24(1). https://doi.org/10.1186/s12913-024-11271-x
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
LITERATURE REVIEW
This week, you will begin a Literature Review Assignment, which will be due Day 7 of Week 10. For this three-part Assignment, you will search for evidence using the tools that are part of the Johns Hopkins Translation of Evidence Model.
Note: This Assignment is hypothetical in nature and is unrelated to your Practicum and DNP Project. However, the work you put in on this Assignment will help prepare you for the Practicum and DNP Project which will come later in your program.
Note: This is a three-part Assignment. By Day 7 of Week 10, you must complete and submit Appendices B, G, and H found in the Dang et.al. text.To Prepare
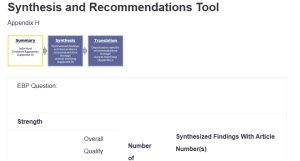
Synthesis and Recommendations Tool
- Review the Literature Review Assignment resources located in this week’s Learning Resources. Pay special attention to Chapters 19, 20, and 21 of the White et al. text; Chapters 4, 5, 6, and 11 of the Dang et al. text; and the articles addressing the PICOT format.
- Note: Be sure to review Appendices B, E, F, G, and H in the Dang et al. text. You will be required to complete and submit Appendices B, G, and H for this Assignment.
- Select an organization with which you are familiar and a practice or organization issue which needs addressing.
- Note: You may reuse organizations and/or issues that you selected earlier in this course or select new ones.
- Consider possible practice questions to address the issue you selected. Ask yourself:
- Why is it a problem?
- What has been done about it?
- What is the gap in practice?
- Select one practice question to develop using Appendix B.
- Note: The PICOT components will assist you in identifying search terms. Make sure your practice question is evidence-based, nursing focused, and has measurable outcomes.
- Using the Walden Library, search the evidence to identify 15 or more recent peer-reviewed articles (within the past 5 years) related to your practice question.
- Note: Use Appendices E and F to help you search, but you do not need to submit these for grading.
- Using Appendix H, grade the evidence and select the 10 articles with the strongest evidence ratings.
- Note: if you have more than 10 articles that you deem worthy, you can enter up to 15 into Appendix H.
- Using Appendix H, synthesize the 10 articles you selected.
- Using Appendix G, enter all relevant information about the 10 articles you selected and synthesized.
- Note: This is a three-part Assignment. By Day 7 of Week 10, you must complete and submit Appendices B, G, and H found in the Dang et.al. text.
For this three-part Assignment, you will submit three items as follows:
- Part 1: Submit your completed Appendix B, which demonstrates your fully developed practice question.
- Part 2: Submit your completed Appendix H, which demonstrates your grading and synthesizing of the evidence you identified. Note: You will complete Appendix H before Appendix G, despite being out of order alphabetically.
- Part 3: Submit your completed Appendix G, which lists the relevant information about the evidence you selected.