Pilot Plan Template – Root-Cause Analysis
Create a pilot plan in response to the VOC report found in the course using this template.
Perform a root-cause analysis by doing the following:
- Critique the continuous quality improvement (CQI) team’s five whys analysis by explaining how it could have been conducted more effectively.
|
The Five Whys analysis is a straightforward yet powerful tool for identifying the root causes of a problem by repeatedly asking the question “Why?” until the fundamental cause is uncovered. However, the CQI team’s application of this analysis could have been more effective in the following ways:
|
- Discuss whether the “why” cycle has been performed to a logical end in which additional questions would not change the response.
|
In a well-conducted Five Whys analysis, the cycle should reach a point where asking additional “Why?” questions no longer adds value or uncovers new information. However, in this case, the cycle may have stopped prematurely. The root causes of doctor-patient communication issues could involve factors like time constraints, insufficient training, or even a cultural gap, which may require asking deeper questions about hospital practices and individual staff behaviors. As for pain management, addressing the issue of patient dissatisfaction involves understanding not just the administration of pain relief but also the patient triage process, nurse responsiveness, and protocol adherence. Therefore, the CQI team should have continued to dig deeper into both systemic and cultural issues until all root causes were fully identified. Additionally, it’s critical that the team continuously cross-checks findings with data (e.g., VOC survey data) and real-time observations to ensure the Five Whys method reaches a logical conclusion. |
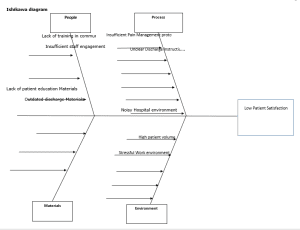
- Using the template below, create an Ishikawa diagram using the information from the SIPOC Process diagram from Task 1 and the five whys analysis.
- Explain the effectiveness of using the Ishikawa diagram to synthesize the results from multiple information sources.
|
The Ishikawa diagram provides an effective tool to visualize how multiple factors contribute to low patient satisfaction. It allows for a comprehensive view of the problem, highlighting the interdependencies between people, processes, materials, and environmental factors. Synthesizing information from both the SIPOC diagram and the Five Whys analysis helps pinpoint areas requiring immediate intervention and informs the development of improvement strategies. |
- Discuss the assumptions that you made about the organization, its processes, or both to complete the Ishikawa diagram.
|
- Using the information from the root-cause analysis in part A (e.g., the five whys analysis and the Ishikawa diagram) and the previously completed project charter from Task 1, do the following:
- Identify three opportunities for improvement.
|
1. |
Doctor-Patient Communication |
|
2. |
Pain Management |
|
3. |
Clarity of Post-Discharge Information |
- Recommend one improvement strategy for each of the three opportunities identified in part B1.
| Opportunity | Improvement Strategy |
| Doctor-Patient Communication | Implement a comprehensive communication training program for all physicians and nursing staff that includes techniques for empathetic listening, cultural competency, and treatment transparency (Ha & Longnecker, 2010). The program should include role-playing and feedback mechanisms to ensure effective implementation. |
| Pain Management | Standardize pain assessment protocols across all departments, using tools like the Visual Analog Scale (VAS) or Numeric Rating Scale (NRS) to ensure that pain management is proactively addressed. This includes training for nurses and physicians on timely pain relief administration, particularly in triage situations (Ahmadi et al., 2016). |
|
Clarity of Post-Discharge Information |
Develop personalized discharge instructions for every patient, considering their individual medical conditions and needs. This should be complemented by a post-discharge follow-up system, where patients receive a call or text to clarify any doubts about their care (Jack et al., 2009). |
- Create an improved process flowchart that represents what an ideal process might look like considering the current Shelbyville Medical Center model from Task 1.
+——————————-+
| Patient Admission |
| (Triage) |
+——————————-+
|
v
+———————————————+
| Initial Assessment |
| (Identify Caregiver, Set Goals, etc.) |
+———————————————+
|
v
+———————————————+
| Daily Rounds & Education |
| (Teach-back, Medication Review, etc.) |
+———————————————+
|
v
+———————————————+
| Discharge Planning |
| (Schedule Meetings, Provide Checklists, |
| Confirm Next Steps) |
+———————————————+
|
v
+———————————————+
| Discharge Meeting |
| (Review Instructions, Confirm |
| Understanding) |
+———————————————+
|
v
+———————————————+
| Final Discharge |
| (Provide Materials, Arrange Follow-Up) |
+———————————————+
|
v
+———————————————+
| Post-Discharge Follow-Up |
| (Phone Call to Confirm Understanding)|
+———————————————+
- Create a pilot implementation plan based on information obtained in parts A and B:
| Pilot Plan | |
| Three process changes that will potentially affect the causal factors driving low patient satisfaction | 1. Doctor communication training
2. Standardized pain management protocol 3. Personalized post-discharge instructions and follow-up
|
| Affected departments or services | Medical and Nursing Staff
Emergency Care, Pain Management, Nursing Nursing, Patient Education, Discharge Coordination |
| Timeline of the projected pilot implementation plan for the process changes | 3-6 months with monthly progress reviews and evaluations. Implementation begins in 1 month. |
| Key metrics relevant to the three process changes that will be measured | 1. Doctor-Patient Communication Satisfaction Score (Goal: ≥82%)
2. Pain Management Satisfaction Score (Goal: ≥85%) 3. Patient Understanding of Discharge Instructions (Goal: ≥60%) |
| Explain how improvement from the baseline will be defined | Improvement will be defined as a percentage increase in patient satisfaction and understanding in all areas of focus. The baseline is taken from the current VOC data. |
| Discuss resources that will be needed to complete the pilot implementation plan, including people, time, and projected costs and how the identified resources are effective and beneficial. | – Personnel: Doctors, Nurses, Discharge Coordinators
– Time: 3-6 months for full implementation – Costs: Estimated $50,000 for training, process redesign, and resource allocation |
| Describe training necessary to complete the pilot implementation plan, including the participants and materials required | – Participants: All doctors, nurses, and discharge coordinators.
– – Materials: Training manuals, communication workshops, pain management guidelines. |
| Recommend an actionable strategy, well supported with evidence, to transition any new improvements into daily operational practice | Ensure ongoing monitoring of the process changes and create feedback loops to adjust training as needed. Integrate improvements into hospital policies. |
- Conduct an impact assessment of your pilot implementation plan by discussing how the proposed plan may affect the following dimensions and including factors related to the-current state, the transition state, and future state.
| Dimension | Impacts |
| Employees at the organization | Improved communication and workflow will enhance job satisfaction and reduce burnout. Training will empower staff to deliver better care and patient interactions. |
| The community that the organization
serves |
Improved patient satisfaction will result in better health outcomes and potentially reduce the need for readmissions, improving community trust in the hospital. |
| Information management at the organization | Enhanced discharge and patient education protocols will require better data tracking systems to ensure accuracy and follow-up. |
APA Sources:
Ahmadi, A., Bazargan-Hejazi, S., Zadie, Z. H., Euasobhon, P., Ketumarn, P., Karbasfrushan, A., Amini-Saman, J., & Mohammadi, R. (2016). Pain management in trauma: A review study. Journal of Injury and Violence Research, 8(2). https://doi.org/10.5249/jivr.v8i2.707
Jack, B. W., Chetty, V. K., Anthony, D., Greenwald, J. L., Sanchez, G. M., Johnson, A. E., … & Culpepper, L. (2009). A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Annals of Internal Medicine, 150(3), 178–187. https://doi.org/10.7326/0003-4819-150-3-200902030-00007
Ha, J. F., & Longnecker, N. (2010). Doctor-patient communication: A review. Ochsner journal, 10(1), 38-43. https://www.ochsnerjournal.org/content/10/1/38
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Pilot Plan Template – Root-Cause Analysis
Introduction
A pilot plan is designed to support your understanding of tools used in the analyze and improve phases of the define, measure, analyze, improve, and control (DMAIC) model. In this task, you will implement the pilot-testing stage of an improvement project. You will also critique the continuous quality improvement (CQI) team’s cause analysis (found in the course) and create a proposed process flowchart revision. The information and insights gained from this task will be used in Task 3, the final report. You should complete Task 1: Initial Report, prior to beginning this task.
Pilot Plan Template – Root-Cause Analysis
Scenario
During the analyze and measure project phases, Shelbyville Medical Center’s CQI team begins to actively engage in potential solutions aligned with the scope and aims detailed in the project charter. One of the first steps that the team members take is performing a root-cause, or cause-and-effects, analysis. They use a five whys format to conduct this analysis.
After completing the five whys analysis, members of the CQI team determine that one of the causal factors of low patient satisfaction is that work tasks are not being divided efficiently at triage. The team suggests implementing procedural workflow training that would support more efficient file processing.
Requirements
Your submission must represent your original work and understanding of the course material. Most performance assessment submissions are automatically scanned through the WGU similarity checker. Students are strongly encouraged to wait for the similarity report to generate after uploading their work and then review it to ensure Academic Authenticity guidelines are met before submitting the file for evaluation. See Understanding Similarity Reports for more information.
Grammarly Note:
Professional Communication will be automatically assessed through Grammarly for Education in most performance assessments before a student submits work for evaluation. Students are strongly encouraged to review the Grammarly for Education feedback prior to submitting work for evaluation, as the overall submission will not pass without this aspect passing. See Use Grammarly for Education Effectively for more information.
Microsoft Files Note:
Write your paper in Microsoft Word (.doc or .docx) unless another Microsoft product, or pdf, is specified in the task directions. Tasks may not be submitted as cloud links, such as links to Google Docs, Google Slides, OneDrive, etc. All supporting documentation, such as screenshots and proof of experience, should be collected in a pdf file and submitted separately from the main file. For more information, please see Computer System and Technology Requirements.
You must use the rubric to direct the creation of your submission because it provides detailed criteria that will be used to evaluate your work. Each requirement below may be evaluated by more than one rubric aspect. The rubric aspect titles may contain hyperlinks to relevant portions of the course.
Create a pilot plan in response to the “Voice of the Customer” (VOC) report found in the course. Complete the attached “Pilot Plan Template,” by doing the following:
A. Perform a root-cause analysis by doing the following:
1. Critique the CQI team’s five whys analysis by explaining how it could have been conducted more effectively.
a. Discuss whether the “why” cycle has been performed to a logical end in which additional questions would not change the response.
2. Create an Ishikawa diagram using the information from the suppliers, inputs, process, outputs, and customers (SIPOC) Process diagram from Task 1, and the five whys analysis.
a. Explain the effectiveness of using the Ishikawa diagram to synthesize the results from multiple information sources.
b. Discuss the assumptions that you made about the organization, its processes, or both to complete the Ishikawa diagram.
B. Using the information from the root-cause analysis in part A (the five whys analysis and the Ishikawa diagram) and the previously completed project charter from Task 1, do the following:
1. Identify three opportunities for improvement.
2. Recommend one improvement strategy for each of the three opportunities identified in part B1.
3. Create an improved process flowchart that represents what an ideal process might look like considering the current Shelbyville Medical Center model from Task 1.
4. Create a pilot implementation plan based on information obtained in parts A and B by doing the following:
a. Discuss three process changes that will potentially affect the causal factors driving low patient satisfaction.
b. Identify the affected departments or services.
c. Identify the timeline of the projected pilot implementation plan for the process changes identified in part B4a.
d. Identify which key metrics will be measured.
i. Explain how improvement from the baseline will be defined.
e. Discuss the resources that will be needed to complete the pilot implementation plan, including people, time, and projected costs.
f. Describe the training necessary to complete the pilot implementation plan, including the participants and materials required.
g. Recommend an actionable strategy to transition any new improvements into daily operational practice.
C. Conduct an impact assessment of your pilot implementation plan by discussing how the proposed plan may affect the following:
1. employees at the organization
2. the community that the organization serves
3. information management at the organization
D. Acknowledge sources, using in-text citations and references, for content that is quoted, paraphrased, or summarized.
E. Demonstrate professional communication in the content and presentation of your submission.
Use the following resources to complete the Pilot Plan.
Required textbook
Healthcare Performance Improvement: A Lean Six Sigma Approach prepares healthcare administrators to meet the challenges of a changing marketplace through the Lean Six Sigma method of quality improvement.
Required PDF
Miller’s Impact Assessment Framework provides an in-depth guide to assessing the potential impact of quality improvement on the multiple dimensions of the organization.