Unit 2 Journal: The Patient Interview
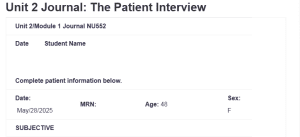
| Unit 2/Module 1 Journal NU552 | |||
| Date Student Name
Complete patient information below. |
|||
| Date: May/28/2025 | MRN: | Age: 48 | Sex: F |
| SUBJECTIVE | |||
| CC: well visit
|
|||
| HPI:
A.N.O, a 48-y/o Caucasian female, present for a well-woman exam. She notes that she is feeling generally well and has no major complaints except for some fatigue, joint pains, and constipation. She notes that she has strictly adhered to her medications as instructed: Unit 2 Journal: The Patient Interview. She reports no new symptoms since the last visit. However, she reports that for the last 2 weeks, the joint pains have developed from mild to a bit moderate, ranging between a scale of 3 and 4, but she can do her usual activities. |
|||
| Medications: HCTZ 50 mg QD. Synthroid brand. 0.75 mg QD
|
|||
| Allergies: NKDA
|
|||
| Past Medical History:
HTN, Hypothyroidism. Cholecystectomy 2019 |
|||
| Family History:
HTN- Father Mother both living Depression- Sister DM2- Grandfather-deceased. Brother. |
|||
| Social History:
Retail Sales Married 2 children/teens. Non-smoker Drinks 1-3 wine glass per week No illicit drug use |
|||
| ROS | |||
| General: No notable weight loss or gain in the last 6 months, reports mild fatigue and joint pains, no history of fever or chills | Peripheral Vascular
No history of swelling on face, hands, and feet. Reports one time she experienced leg cramps. |
||
| Skin: No rashes or lesions, history of dry skin | Urinary | ||
| HEENT: Denies headaches, dizziness, lightheadedness, ear pain, or nasal congestion. No reported vision changes or hearing loss | Genitalia/Reproductive
No reported issues or concerns |
||
| Neck: Denies any neck pain, sore throat, swelling, or difficulty swallowing.
|
Musculoskeletal: Reports mild joint pain, no history of joint stiffness | ||
| Breasts: No history of breast lumps, tenderness, or discharge | Neurological: Denies fainting and seizures. No history of sudden weakness or paralysis. No changes in sensation. | ||
| Respiratory
Denies SOB, dyspnea, or cough. |
Hematologic: No reported ease of bruising or bleeding | ||
| Cardiovascular
History of HTN. Denies chest pain |
Endocrine: History of hypothyroidism | ||
| Gastrointestinal
Reports constipation and mild abdominal pain; denies nausea and vomiting |
Psychiatric: No reported episodes of anxiety or depressive symptoms | ||
| Patient interview processes must consider and recognize aspects of diversity, inclusion, gender, culture, and ethnicity as they are central to ethical decision-making (Juntunen et al., 2023). Considering the culture, which is usually tied to the ethnicity of a patient, and their gender during the patient interview ensures the quality of communication is high (Tran, 2021), and also ensures that the care is modelled around the patient; hence, the delivery of patient-centered care.
Such considerations also create an inclusive care environment which can lead to the patient getting more engaged in the care process, better experiences, and higher patient satisfaction with care (Timmermans, 2020).
|
|||
References
Juntunen, C. L., Crepeau-Hobson, F., Riva, M. T., Baker, J., Wan, S., Davis, C., & Caballero, A. M. (2023). Centering equity, diversity, and inclusion in ethical decision-making. Professional Psychology: Research and Practice, 54(1), 17–27. https://doi.org/10.1037/pro0000488
Timmermans, S. (2020). The engaged patient: The relevance of patient–physician communication for twenty-first-century health. Journal of Health and Social Behavior, 61(3), 259–273. https://doi.org/10.1177/0022146520943514
Tran, B. Q. (2021). Strategies for effective patient care: Integrating quality communication with the patient-centered approach. Social and Personality Psychology Compass, 15(1), e12574. https://doi.org/10.1111/SPC3.12574
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Apply a systematic approach with critical thinking to a subjective focused or comprehensive patient history intake interview, taking into consideration gender, culture, and ethnicity and ethical decision making.
The Patient Interview
In this competency assessment you will submit a Kaltura video and subjective note, demonstrating your skill in completing a subjective patient interview. Use this Journal Template.
You will use a live person volunteer, not a patient, and conduct the interview as a professional medical provider. Prepare in advance with your questions and knowledge of the components. Be sure to read the required readings and watch the videos assigned in the readings.
Your final production video will be about 5 minutes, and should not exceed 6 minutes; so your preparation and succinctness in the process and moving the patient through the interview is important. Your communication should be clear and concise; smoothly transitioning.
Unit 2 Journal: The Patient Interview
This is an existing patient and much of the health history can be reviewed rather than initially collected. The patient’s family history and medical history would have been assessed on prior visits. You should briefly confirm the record and include it in the documentation. Have your questions ready as you conduct the interview.
Health preventive screenings should be addressed on a well-visit. All components of the subjective interview should be included in the documentation. The review of systems, ROS, interview process and topic names can be somewhat different based on EMR. It is important to be adaptable to minor changes in EMRs, templates and format based on medical facility use and preference.
Finally as a part of this assignment include how the nurse practitioner considers gender, culture, ethnicity and ethical decision making during the patient interview process for this case and in general. Include 3 evidence-based resources. Be sure to include OLDCARTS in the HPI.
This assignment is the subjective part of the medical visit. You are not touching the patient.

