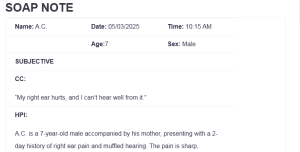
SOAP NOTE
| Name: A.C. | Date: 05/03/2025 | Time: 10:15 AM |
| Age:7 | Sex: Male | |
| SUBJECTIVE | ||
| CC:
“My right ear hurts, and I can’t hear well from it.” |
||
| HPI:
A.C. is a 7-year-old male accompanied by his mother, presenting with a 2-day history of right ear pain and muffled hearing. The pain is sharp, intermittent, and worsens at night. His mother reports associated symptoms of low-grade fever (maximum 100.8°F), increased irritability, and decreased appetite: SOAP NOTE. No vomiting or diarrhea. No recent trauma. The patient had a cold about one week ago, which has mostly resolved, except for a lingering runny nose. No history of similar episodes requiring surgical intervention. No known exposure to sick contacts in school. |
||
| Medications:
Children’s Tylenol (acetaminophen) 160 mg/5mL, 5 mL every 6 hours as needed for fever and pain. |
||
| PMH
Allergies: No known drug allergies
Medication Intolerances:
None reported
Chronic Illnesses/Major traumas
None reported
Hospitalizations/Surgeries
No history of hospitalizations or surgeries
No history of diabetes, HTN, asthma, cancer, TB, thyroid, psychiatric, or kidney disorders. |
||
| Family History
No history of recurrent ear infections. A.C.’s father has hypertension, and the mother is healthy. No family history of TB, cancer, or hereditary hearing loss. |
||
| Social History
Lives with both parents and one younger sibling. Attends elementary school. Up to date on vaccinations. No tobacco, alcohol, or drug exposure. Safe home environment. |
||
| ROS | |
| General
Mild fatigue and irritability, low-grade fever. |
Cardiovascular
No chest pain or palpitations. |
| Skin
No rash, bruising, or lesions. |
Respiratory
No cough or shortness of breath; residual nasal congestion. |
| Eyes
No visual disturbances. |
Gastrointestinal
Decreased appetite, no vomiting or diarrhea. |
| Ears
Right ear pain, decreased hearing, no drainage. |
Genitourinary/Gynecological
Normal urination. |
| Nose/Mouth/Throat
Mild nasal congestion, sore throat resolved. |
Musculoskeletal
No pain or swelling. |
| Breast
No concerns reported |
Neurological
No dizziness, syncope, or seizures. |
| Heme/Lymph/Endo
No night sweats, gland swelling, or endocrine complaints. |
Psychiatric
No depression, anxiety, or sleep disturbance apart from illness. |
| OBJECTIVE | |
| Weight 24 kg BMI 16.4
|
Temp 100.8°F | BP 102/64 |
| Height 124 cm
|
Pulse 92 bpm | Resp 20 bpm |
| General Appearance
Well-nourished child in mild distress due to ear pain. Alert and interactive. |
||
| Skin
Warm, dry, intact. No lesions or rash. |
||
| HEENT
Head is normocephalic, atraumatic, and without lesions. Eyes: PERRLA. EOMs intact. No conjunctival injection. Ears: The right tympanic membrane is erythematous, bulging, and without normal light reflex; limited mobility on pneumatic otoscopy. Left tympanic membrane normal. No discharge noted. Nose: Clear mucus and slight swelling of the nasal mucosa. Wet oral mucosa. Tonsils are not erythematous or swollen. |
||
| Cardiovascular
Regular rate and rhythm. No murmurs or gallops. |
||
| Respiratory
Clear to auscultation bilaterally. No wheezing or rales.
|
||
| Gastrointestinal
Soft, non-distended. Normal bowel sounds. No tenderness or masses.
|
||
| Breast
Breast is free from masses or tenderness, no discharge, no dimpling, wrinkling or discoloration of the skin.
|
||
| Genitourinary
Bladder is not distended, normal urination. |
||
| Musculoskeletal
Normal gait. No joint swelling or pain. |
||
| Neurological
Alert, appropriate affect. Normal speech and coordination. |
||
| Psychiatric
Appropriate behavior for age. No concerns noted. |
||
| Lab Tests
Not required for routine acute otitis media unless complications are suspected.
|
| Special Tests
Pneumatic otoscopy confirms decreased tympanic membrane mobility on the right side.
|
| Diagnosis |
| Differential Diagnoses
o 1- Acute Otitis Media (AOM) – Right Ear (ICD-10 Code: H66.91) The diagnosis is most probably Acute Otitis Media because this condition presents symptoms such as right-sided earache, low-grade fever, hearing loss, and tympanic membrane (TM), which appears to be bulging with no light reflex. These signs manifest after a severe viral upper respiratory illness, which is a frequent reason for AOM because of eustachian tube dysfunction and consequent fluid retention in the middle ear (Danishyar & Ashurst, 2023). This patient is presenting with a sudden onset of pain and fever, and on pneumatic otoscopy, the diagnosis of AOM would seem to be most likely. o 2- Otitis Media with Effusion (OME) (ICD-10 Code: H65.91) OME is more common in children and presents with middle ear effusion but without signs of acute infection. It may follow AOM or viral infection and is mostly recognized by hearing loss or fullness in the ear as opposed to pain or fever (Searight et al., 2023). In this case, there is ear pain, fever, and inflammation of the TM, which cannot be explained by the OME diagnosis only. While middle ear fluid might be present, the inflammatory signs indicate an active infection rather than a sterile effusion. o 3- Otitis Externa (OE) ICD-10 Code: H60.91 Otitis externa or “swimmer’s ear” involves inflammation of the external auditory canal. It is commonly associated with ear pain worsened by manipulation of the tragus or pinna and may involve canal swelling or discharge (Medina-Blasini & Sharman, 2023). This patient lacks such features: the pain is localized internally, and the canal is patent and non-tender, making OE a less likely differential in this case. Diagnosis o Acute Otitis Media (Right Ear) (ICD-10 Code: H66.91) The final diagnosis arrived at is Acute Otitis Media of the right ear. This is supported by a bulging erythematous TM with reduced mobility, a history of a recent URI, fever, and otalgia. The pneumatic otoscopy that reveals purulent middle ear effusion enhances this diagnosis and strengthens the conviction of its accuracy
|
| Plan/Therapeutics |
| o Plan:
§ Further testing Routine laboratory testing is not required for uncomplicated AOM. Additional diagnostics may be considered if the patient does not improve after 48–72 hours or presents with signs of complications such as mastoiditis or persistent high fever.
§ Medication First-line treatment is high-dose amoxicillin at 90 mg/kg/day, divided into two doses. For this child, weighing approximately 24 kg, the recommended dose is 540 mg twice daily. The appropriate prescription is Amoxicillin 400 mg/5 mL oral suspension, dosed at 6.75 mL BID for 10 days (Akhavan et al., 2023). To manage fever and pain, Acetaminophen 160 mg/5 mL, dosed at 5 mL every 6 hours as needed, is advised.
§ Education The caregiver should be thoroughly educated on the importance of completing the full course of antibiotics, even if symptoms improve before completion. Warning signs requiring immediate reassessment include persistent fever beyond 72 hours, increasing ear pain, swelling behind the ear, or signs of systemic illness. Preventative advice includes minimizing water entry into the affected ear, practicing good hand hygiene, and avoiding exposure to second-hand smoke, all of which can reduce recurrence risk. It is also helpful to explain the typical course of AOM and set expectations regarding recovery.
§ Non-medication treatments Supportive care includes using warm compresses over the affected ear to ease discomfort, ensuring the child stays hydrated, and promoting rest. Sleeping with the head elevated may also help relieve pressure in the middle ear and improve drainage. |
| Evaluation of Patient Encounter
The child tolerated the physical examination without complication. The caregiver demonstrated an understanding of the diagnosis and treatment plan, including medication administration, symptom monitoring, and appropriate use of supportive measures. A follow-up appointment is scheduled for 10 days or sooner if there is no improvement or worsening of symptoms. The family expressed confidence in managing care at home based on the instructions provided.
|
References
Akhavan, B. J., Vijhani, P., & Khanna, N. (2023). Amoxicillin. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482250/
Danishyar, A., & Ashurst, J. V. (2023, April 15). Acute otitis media. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470332/
Medina-Blasini, Y., & Sharman, T. (2023, July 31). Otitis externa. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK556055/
Searight, F. T., Singh, R., & Peterson, D. C. (2023, May 20). Otitis media with effusion. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538293/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
| Name: | Date: | Time: |
| Age: | Sex: | |
| SUBJECTIVE | ||
| CC:
Reason given by the patient for seeking medical care “in quotes” |
||
| HPI:
Describe the course of the patient’s illness, including when it began, character of symptoms, location where the symptoms began, aggravating or alleviating factors; pertinent positives and negatives, other related diseases, past illnesses, surgeries or past diagnostic testing related to present illness. |
||
| Medications: (list with reason for med ) | ||
| PMH
Allergies:
Medication Intolerances:
Chronic Illnesses/Major traumas
Hospitalizations/Surgeries
“Have you every been told that you have: Diabetes, HTN, peptic ulcer disease, asthma, lung disease, heart disease, cancer, TB, thyroid problems or kidney disease or psychiatric diagnosis.” |
||
| Family History
Does your mother, father or siblings have any medical or psychiatric illnesses? Anyone diagnosed with: lung disease, heart disease, htn, cancer, TB, DM, or kidney disease. |
||
| Social History
Education level, occupational history, current living situation/partner/marital status, substance use/abuse, |
||
| ETOH, tobacco, marijuana. Safety status | |
| ROS | |
| General
Weight change, fatigue, fever, chills, night sweats, energy level |
Cardiovascular
Chest pain, palpitations, PND, orthopnea, edema |
| Skin
Delayed healing, rashes, bruising, bleeding or skin discolorations, any changes in lesions or moles |
Respiratory
Cough, wheezing, hemoptysis, dyspnea, pneumonia hx, TB |
| Eyes
Corrective lenses, blurring, visual changes of any kind |
Gastrointestinal
Abdominal pain, N/V/D, constipation, hepatitis, hemorrhoids, eating disorders, ulcers, black tarry stools |
| Ears
Ear pain, hearing loss, ringing in ears, discharge |
Genitourinary/Gynecological
Urgency, frequency burning, change in color of urine.
Contraception, sexual activity, STDS
Fe: last pap, breast, mammo, menstrual complaints, vaginal discharge, pregnancy hx
Male: prostate, PSA, urinary complaints |
| Nose/Mouth/Throat
Sinus problems, dysphagia, nose bleeds or discharge, dental disease, hoarseness, throat pain |
Musculoskeletal
Back pain, joint swelling, stiffness or pain, fracture hx, osteoporosis |
| Breast
SBE, lumps, bumps or changes |
Neurological
Syncope, seizures, transient paralysis, weakness, paresthesias, black out spells |
| Heme/Lymph/Endo
HIV status, bruising, blood transfusion hx, night sweats, swollen glands, increase thirst, increase hunger, cold or heat intolerance |
Psychiatric
Depression, anxiety, sleeping difficulties, suicidal ideation/attempts, previous dx |
| OBJECTIVE | |
| Weight BMI | Temp | BP |
| Height | Pulse | Resp |
| General Appearance
Healthy appearing adult female in no acute distress. Alert and oriented; answers questions appropriately. Slightly somber affect at first, then brighter later. |
||
| Skin
Skin is brown, warm, dry, clean and intact. No rashes or lesions noted. |
||
| HEENT
Head is normocephalic, atraumatic and without lesions; hair evenly distributed. Eyes: PERRLA. EOMs intact. No conjunctival or scleral injection. Ears: Canals patent. Bilateral TMs pearly grey with positive light reflex; landmarks easily visualized. Nose: Nasal mucosa pink; normal turbinates. No septal deviation. Neck: Supple. Full ROM; no cervical lymphadenopathy; no occipital nodes. No thyromegaly or nodules. Oral mucosa pink and moist. Pharynx is nonerythematous and without exudate. Teeth are in good repair. |
||
| Cardiovascular
S1, S2 with regular rate and rhythm. No extra sounds, clicks, rubs or murmurs. Capillary refill 2 seconds. Pulses 3+ throughout. No edema. |
||
| Respiratory
Symmetric chest wall. Respirations regular and easy; lungs clear to auscultation bilaterally. |
||
| Gastrointestinal
Abdomen obese; BS active in all 4 quadrants. Abdomen soft, non-tender. No hepatosplenomegaly. |
||
| Breast
Breast is free from masses or tenderness, no discharge, no dimpling, wrinkling or discoloration of the skin. |
||
| Genitourinary
Bladder is non-distended; no CVA tenderness. External genitalia reveals coarse pubic hair in normal distribution; skin color is consistent with general pigmentation. No vulvar lesions noted. Well estrogenized. A small speculum was inserted; vaginal walls are pink and well rugated; no lesions noted. Cervix is pink and nulliparous. Scant clear to cloudy drainage present. On bimanual exam, cervix is firm. No CMT. Uterus is antevert and positioned behind a slightly distended bladder; no fullness, masses, or tenderness. No adnexal masses or tenderness. Ovaries are non-palpable. (Male: both testes palpable, no masses or lesions, no hernia, no uretheral discharge. ) (Rectal as appropriate: no evidence of hemorrhoids, fissures, bleeding or masses—Males: prostrate is smooth, non-tender and free from nodules, is of normal size, sphincter tone is firm). |
||
| Musculoskeletal
Full ROM seen in all 4 extremities as patient moved about the exam room. |
||
| Neurological
Speech clear. Good tone. Posture erect. Balance stable; gait normal. |
||
| Psychiatric
Alert and oriented. Dressed in clean slacks, shirt and coat. Maintains eye contact. Speech is soft, though clear and of normal rate and cadence; answers questions appropriately. |
||
SOAP NOTE
| Lab Tests
Urinalysis – pending Urine culture – pending Wet prep – pending |
| Special Tests |
| Diagnosis |
| Differential Diagnoses
o 1- o 2- o 3- Diagnosis o |
| Plan/Therapeutics |
| o Plan:
§ Further testing § Medication § Education § Non-medication treatments |
| Evaluation of patient encounter |

