SOAP NOTE
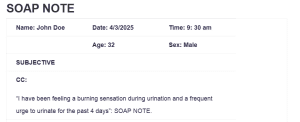
| Name: John Doe | Date: 4/3/2025 | Time: 9: 30 am |
| Age: 32 | Sex: Male | |
| SUBJECTIVE | ||
| CC:
“I have been feeling a burning sensation during urination and a frequent urge to urinate for the past 4 days”: SOAP NOTE. |
||
| HPI:
The patient reports experiencing a burning sensation when urinating and increased frequency over the past four days. He states that the symptoms started mildly but are worsening. He has not had fever, chills, or pain in the sides or back. His Sexual activity has also not changed, and he has had no new partners. There’s no history of kidney stones or urinary tract infections, nor recent surgeries or medical tests related to these symptoms. |
||
| Medications: Ibuprofen 400 mg as needed for pain (for occasional headaches). | ||
| PMH
Allergies: No known drug allergies.
Medication Intolerances: None
Chronic Illnesses/Major traumas: None
Hospitalizations/Surgeries: No past hospitalizations or surgeries.
The patient does not have any known history of Diabetes, HTN, peptic ulcer disease, asthma, lung disease, heart disease, cancer, TB, thyroid problems, or kidney disease or psychiatric diagnosis |
||
| Family History
His father has a history of Hypertension and heart disease. His mother has Type 2 Diabetes. His siblings have no significant medical or psychiatric illnesses |
||
| Social History | ||
|
John is an accountant with a degree in finance. He lives in the suburbs with his wife and their two children. He works full-time in a well-respected accounting firm. John’s family life is supportive, and he is able to maintain a good balance between work and personal time. He does not use tobacco, alcohol, or drugs, and maintains his health through regular jogging and cycling. John feels secure at home, with no issues related to domestic violence or safety concerns. He is also engaged in his community by attending local events and volunteering at a nearby shelter. |
|
| ROS | |
| General
No weight change, fatigue, fever, chills, night sweat. No abnormalities in energy level |
Cardiovascular
No Chest pain, palpitations, PND, orthopnea or edema |
| Skin
No delayed healing, rashes, bruising, bleeding or skin discolorations. No changes in lesions or moles |
Respiratory
No cough, wheezing, hemoptysis, dyspnea. No known history of pneumonia or TB |
| Eyes
No corrective lenses, blurring or visual changes. |
Gastrointestinal
No abdominal pain, N/V/D, constipation or hemorrhoids, No black tarry stools |
| Ears
No ear pain, hearing loss, ringing in ears or discharge |
Genitourinary/Gynecological
Burning sensation during urination, increased frequency of urination No change in urine color. No prostate or sexual activity concerns.
|
| Nose/Mouth/Throat
No Sinus problems, dysphagia, nose bleeds or discharge No dental disease, hoarseness or throat pain |
Musculoskeletal
No back pain, joint swelling, stiffness or pain. Fracture. |
| Breast
No lumps, bumps, or changes |
Neurological
No syncope, seizures, paralysis, weakness, or black out spells. |
| Heme/Lymph/Endo
There are no concerns about his HIV status. No history of bruising, no history of blood transfusions, night sweats, swollen glands, increased thirst or hunger, cold or heat intolerance. |
Psychiatric
No depression, anxiety, sleeping difficulties or suicidal ideation/attempts |
| OBJECTIVE | |
| Weight BMI | Temp | BP |
| Height | Pulse | Resp |
| General Appearance
He is a healthy appearing adult male in no acute distress. He is also alert and oriented as he answers questions appropriately. He was slightly somber at first, but brighter later. |
||
| Skin
He’s skin is brown, warm, dry, clean and intact. No rashes or lesions noted. |
||
| HEENT
Head is normocephalic, atraumatic and without sores, and hair is evenly spread. The eyes are clear, displaying PERRLA and EOMs (extraocular movements) intact, with no conjunctival or scleral injection. The ears are clear, eardrums are healthy gray with normal light reflections. The nasal lining is pink, structures are normal. The neck moves freely with no swollen lymph nodes or lumps and no thyroid enlargement. The mouth’s lining is pink and moist, the throat is normal, with no redness or pus, and the teeth are in good shape |
||
| Cardiovascular
S1, S2 with regular rate and rhythm. No extra sounds, clicks, rubs or murmurs. Capillary refill 2 seconds. Pulses 3+ throughout. No edema. |
||
| Respiratory
Symmetric chest wall. Respirations regular and easy; lungs clear to auscultation bilaterally. |
||
| Gastrointestinal
Abdomen soft and non-tender. No hepatosplenomegaly. |
||
| Breast
No wrinkling or discoloration of the skin. |
||
| Genitourinary
Bladder is non-distended; no CVA tenderness. External genitalia reveal normal distribution of coarse pubic hair; skin color is consistent with general pigmentation. There are no sores or discharge from the urethra. Both testicles are palpable with no lumps, sores, or hernias. |
||
| Musculoskeletal
Full ROM seen in all 4 extremities as patient moved about the exam room. |
||
| Neurological
The patient is alert and oriented. No signs of acute neurological distress. His gait is also normal, and speech is clear. |
||
| Psychiatric
The patient is alert and oriented and is dressed in clean clothes. He also maintains eye contact, his speech soft, but clear and of normal rate. He also answers questions appropriately. |
||
| Lab Tests
Urinalysis – pending Urine culture – pending Wet prep – pending |
| Special Tests; None |
| Diagnosis |
| Differential Diagnoses
1- Prostatitis: Prostatitis, acute or chronic, is the swelling of the prostate gland. This condition is often a result of bacterial infections, but it can still occur without bacterial infections. Symptoms include pelvic pain, pain during urination, frequent urination, and urgency. Additional symptoms include pain during ejaculation and lower back pain. However, John denies having pelvic pain and lower back pain, and has no history of prostate problems, making prostatitis a less likely primary diagnosis (Kaur & Kaur, 2021). 2- Bladder Cancer (Urothelial Carcinoma): Urothelial carcinoma is a form of bladder cancer that affects the lining of the bladder. It is more common in older men, particularly those who smoke or have been exposed to specific harmful chemicals. Patients with bladder cancer may see blood in their urine, feel the need to urinate more often during the day, get up at night to urinate, experience a sudden urge to urinate, or struggle with incontinence. Some might also feel pain in their sides. Although John Doe has symptoms like frequent urination, he does not report hematuria or a history of smoking, which are key indicators of bladder cancer, making blood cancer less likely the primary diagnosis (Ghoreifi, & Djaladat, (2024) 3- Urethritis: Urethritis involves inflammation of the urethra and is commonly caused by sexually transmitted infections like gonorrhea or chlamydia. It is more prevalent in sexually active men. Patients with urethritis may experience pain during urination, discharge from the urethra, and frequent urination. Itching or irritation at the urethral opening might also occur. In sexually active males, symptoms such as painful urination and urethral discharge point towards urethritis (Kaur & Kaur, 2021). John does not report urethral discharge, hence it is unlikely that urethritis is the primary diagnosis. Diagnosis Urinary tract infections (UTIs) often happen due to bacteria like Escherichia coli (E. coli) entering the urinary tract, which causes swelling and infection. John’s symptoms indicate he likely has a UTI because they started recently, he does not have a fever, and he is not at risk for more serious issues like kidney infections or bladder cancer. The most common treatment involves antibiotics such as trimethoprim-sulfamethoxazole, known as Bactrim. Tests, including urinalysis and urine culture, will confirm the diagnosis and help decide the best treatment. It’s vital for John to complete his antibiotics and learn ways to prevent future infections to ensure proper recovery (Kaur & Kaur, 2021) |
| Plan/Therapeutics |
| o Plan:
§ Further testing: a urinalysis and urine culture will be done to confirm the presence of a UTI and identify the causative organism. § Medication: once a diagnosis is made, an antibiotic therapy with trimethoprim-sulfamethoxazole (Bactrim) 160 mg/800 mg BID for 7 days will be initiated. § Education: it will be important to educate the patient about the importance of completing the dose of antibiotics even if symptoms improve and also educate him on the preventive measures to reduce the risk the UTIs recurring. § Non-medication treatments: it is recommended that the patient take warm sitz baths to provide relief.
|
| Evaluation of patient encounter |
References
Kaur, R., & Kaur, R. (2021). Symptoms, risk factors, diagnosis and treatment of urinary tract infections. Postgraduate medical journal, 97(1154), 803–812. https://doi.org/10.1136/postgradmedj-2020-139090
Ghoreifi, A., & Djaladat, H. (2024). A Comprehensive Review on Upper Tract Urothelial Carcinoma: An Update in 2023. Cancers, 16(9), 1613. https://doi.org/10.3390/cancers16091613
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
SOAP NOTE
| Name: | Date: | Time: |
| Age: | Sex: | |
| SUBJECTIVE | ||
| CC:
Reason given by the patient for seeking medical care “in quotes” |
||
| HPI:
Describe the course of the patient’s illness, including when it began, character of symptoms, location where the symptoms began, aggravating or alleviating factors; pertinent positives and negatives, other related diseases, past illnesses, surgeries or past diagnostic testing related to present illness. |
||
| Medications: (list with reason for med ) | ||
| PMH
Allergies:
Medication Intolerances:
Chronic Illnesses/Major traumas
Hospitalizations/Surgeries
“Have you every been told that you have: Diabetes, HTN, peptic ulcer disease, asthma, lung disease, heart disease, cancer, TB, thyroid problems or kidney disease or psychiatric diagnosis.” |
||
| Family History
Does your mother, father or siblings have any medical or psychiatric illnesses? Anyone diagnosed with: lung disease, heart disease, htn, cancer, TB, DM, or kidney disease. |
||
| Social History
Education level, occupational history, current living situation/partner/marital status, substance use/abuse, |
||
SOAP NOTE
| ETOH, tobacco, marijuana. Safety status | |
| ROS | |
| General
Weight change, fatigue, fever, chills, night sweats, energy level |
Cardiovascular
Chest pain, palpitations, PND, orthopnea, edema |
| Skin
Delayed healing, rashes, bruising, bleeding or skin discolorations, any changes in lesions or moles |
Respiratory
Cough, wheezing, hemoptysis, dyspnea, pneumonia hx, TB |
| Eyes
Corrective lenses, blurring, visual changes of any kind |
Gastrointestinal
Abdominal pain, N/V/D, constipation, hepatitis, hemorrhoids, eating disorders, ulcers, black tarry stools |
| Ears
Ear pain, hearing loss, ringing in ears, discharge |
Genitourinary/Gynecological
Urgency, frequency burning, change in color of urine.
Contraception, sexual activity, STDS
Fe: last pap, breast, mammo, menstrual complaints, vaginal discharge, pregnancy hx
Male: prostate, PSA, urinary complaints |
| Nose/Mouth/Throat
Sinus problems, dysphagia, nose bleeds or discharge, dental disease, hoarseness, throat pain |
Musculoskeletal
Back pain, joint swelling, stiffness or pain, fracture hx, osteoporosis |
| Breast
SBE, lumps, bumps or changes |
Neurological
Syncope, seizures, transient paralysis, weakness, paresthesias, black out spells |
| Heme/Lymph/Endo
HIV status, bruising, blood transfusion hx, night sweats, swollen glands, increase thirst, increase hunger, cold or heat intolerance |
Psychiatric
Depression, anxiety, sleeping difficulties, suicidal ideation/attempts, previous dx |
| OBJECTIVE | |
| Weight BMI | Temp | BP |
| Height | Pulse | Resp |
| General Appearance
Healthy appearing adult female in no acute distress. Alert and oriented; answers questions appropriately. Slightly somber affect at first, then brighter later. |
||
| Skin
Skin is brown, warm, dry, clean and intact. No rashes or lesions noted. |
||
| HEENT
Head is normocephalic, atraumatic and without lesions; hair evenly distributed. Eyes: PERRLA. EOMs intact. No conjunctival or scleral injection. Ears: Canals patent. Bilateral TMs pearly grey with positive light reflex; landmarks easily visualized. Nose: Nasal mucosa pink; normal turbinates. No septal deviation. Neck: Supple. Full ROM; no cervical lymphadenopathy; no occipital nodes. No thyromegaly or nodules. Oral mucosa pink and moist. Pharynx is nonerythematous and without exudate. Teeth are in good repair. |
||
| Cardiovascular
S1, S2 with regular rate and rhythm. No extra sounds, clicks, rubs or murmurs. Capillary refill 2 seconds. Pulses 3+ throughout. No edema. |
||
| Respiratory
Symmetric chest wall. Respirations regular and easy; lungs clear to auscultation bilaterally. |
||
| Gastrointestinal
Abdomen obese; BS active in all 4 quadrants. Abdomen soft, non-tender. No hepatosplenomegaly. |
||
| Breast
Breast is free from masses or tenderness, no discharge, no dimpling, wrinkling or discoloration of the skin. |
||
| Genitourinary
Bladder is non-distended; no CVA tenderness. External genitalia reveals coarse pubic hair in normal distribution; skin color is consistent with general pigmentation. No vulvar lesions noted. Well estrogenized. A small speculum was inserted; vaginal walls are pink and well rugated; no lesions noted. Cervix is pink and nulliparous. Scant clear to cloudy drainage present. On bimanual exam, cervix is firm. No CMT. Uterus is antevert and positioned behind a slightly distended bladder; no fullness, masses, or tenderness. No adnexal masses or tenderness. Ovaries are non-palpable. (Male: both testes palpable, no masses or lesions, no hernia, no uretheral discharge. ) (Rectal as appropriate: no evidence of hemorrhoids, fissures, bleeding or masses—Males: prostrate is smooth, non-tender and free from nodules, is of normal size, sphincter tone is firm). |
||
| Musculoskeletal
Full ROM seen in all 4 extremities as patient moved about the exam room. |
||
| Neurological
Speech clear. Good tone. Posture erect. Balance stable; gait normal. |
||
| Psychiatric
Alert and oriented. Dressed in clean slacks, shirt and coat. Maintains eye contact. Speech is soft, though clear and of normal rate and cadence; answers questions appropriately. |
||
| Lab Tests
Urinalysis – pending Urine culture – pending Wet prep – pending |
| Special Tests |
| Diagnosis |
| Differential Diagnoses
o 1- o 2- o 3- Diagnosis o |
| Plan/Therapeutics |
| o Plan:
§ Further testing § Medication § Education § Non-medication treatments |
| Evaluation of patient encounter |
- SOAP NOTE
- basic UTI for a Male patient
- Similar to the recent soap note done on a female, just on a middle-aged male patient.

