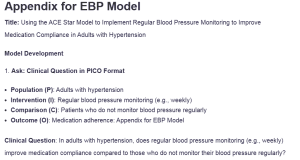
Appendix for EBP Model
Title: Using the ACE Star Model to Implement Regular Blood Pressure Monitoring to Improve Medication Compliance in Adults with Hypertension
Model Development
- Ask: Clinical Question in PICO Format
- Population (P): Adults with hypertension
- Intervention (I): Regular blood pressure monitoring (e.g., weekly)
- Comparison (C): Patients who do not monitor blood pressure regularly
- Outcome (O): Medication adherence: Appendix for EBP Model
Clinical Question: In adults with hypertension, does regular blood pressure monitoring (e.g., weekly) improve medication compliance compared to those who do not monitor their blood pressure regularly?
- Acquire: List Titles of Best Evidence and Levels of Evidence
- Title: Medication adherence and blood pressure control: A scientific statement from the American Heart Association
- Level of Evidence: Systematic review, Meta-analysis
- Summary: This statement supports the correlation between regular blood pressure monitoring and improved medication adherence.
- Title: Patients with hypertension and their compliance with at-home blood pressure monitoring
- Level of Evidence: Randomized controlled trial (RCT)
- Summary: This particular RCT can conclusively show that home blood pressure monitoring serves to enhance the adherence rates among hypertensive patients.
- Title: A mixed-methods study examining the factors that support and hinder blood pressure telemonitoring
- Level of Evidence: Mixed-methods study, Expert opinion
- Summary: This study reveals the barriers to practicing blood pressure telemonitoring, particularly in resource-deprived communities and the possible advantages.
- Appraise: Best Evidence Summary
- Study 1: Blood pressure management and medication compliance (AHA Statement)
- Summary: This statement supports the effectiveness of regular monitoring in improving patient adherence to prescribed medications, thereby controlling blood pressure and reducing cardiovascular complications.
- Study 2: Home blood pressure monitoring (RCT)
- Summary: The RCT reveals that patients are more compliant with medication plans and overall decreased chances of hypertensive crisis if they maintain blood pressure checkups often at home.
- Study 3: Blood pressure telemonitoring (Mixed-methods study)
- Summary: This study identifies some enablers and challenges of telehealth solutions for blood pressure monitoring but adds that digital health interventions are a real boost to medication compliance provided the right support is provided throughout the process.
- Apply: Ethical Considerations
- Ethical Considerations:
- Informed Consent: The patient has to agree and be aware of different aspects of blood pressure monitoring, advantages, and possible drawbacks so they can agree to take the test.
- Privacy (HIPAA): Patient information should be safeguarded at all times, and all patient information should remain compliant with HIPAA rules, especially when technology is used for blood pressure measurement.
- Bioethical Principles:
- Beneficence: The intervention increases patient health literacy on medication regimes, enhances dosing compliance, and controls of blood pressure to reduce potentially fatal conditions such as stroke or heart failure.
- Justice: Help increase the utilization of blood pressure monitoring instruments and information delivery with the aim of bridging the inequality in hypertension control.
- Assess: Measures for Successful Implementation
- Measures:
- Medication Adherence Rate
- Who: APNs and healthcare providers
- What: Medication adherence will be measured using pharmacy refill data and self-reports from patients.
- When: Quarterly evaluations
- How Often: Data will be reviewed every three months
- Benchmark: A 20% increase in medication adherence after six months of intervention.
- Blood Pressure Control
- Who: Patients, APNs, and healthcare providers
- What: Blood pressure control will be measured by the proportion of patients that reach their desired blood pressure readings (less than 140/90 mmHg).
- When: Every three months during follow-up visits
- How Often: Reviewed at each follow-up appointment
- Benchmark: 90% of patients will maintain blood pressure within target levels by the end of the first year.
- Patient Satisfaction
- Who: Patients
- What: Patient satisfaction with the monitoring process will be evaluated using surveys.
- When: At six months and one year
- How Often: Annually
- Benchmark: 85% of comments about perceived benefits and ease of usage should be positive.
- Medication Adherence Rate
Strengths and Barriers
Strengths of the Implementation Plan
- Evidence-based guidelines: Existing research strongly supports the effectiveness of regular blood pressure monitoring in improving medication adherence.
- Accessibility: Home blood pressure monitors are becoming more affordable and widely available, especially in urban settings.
- Technological support: Digital health tools (mobile apps, telehealth) can enhance patient engagement and adherence tracking
Barriers of the Implementation Plan
- Health literacy: Some patients may struggle to understand how to properly monitor their blood pressure or the importance of doing so regularly.
- Financial constraints: Low-income populations may have difficulty affording home monitoring devices or medications.
- Healthcare system challenges: Limited resources in some regions may hinder the widespread implementation of telehealth tools or regular follow-up visits.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Model Development
- Ask: clinical question must be clearly identified in PICO format.
- Acquire: List titles of best evidence outlined to answer clinical question and include the levels of evidence used to support implementation from your literature search. (3 minimum.).
- Appraise: Summarize in 1-2 short bullets the best evidence from each study or guideline/position statement (identified in #2). The bullet items should briefly summarize evidence to support validity and applicability to the problem and situation for each study/guideline.
- Apply: Briefly state at least 2 ethical considerations and why they are important for this population or implementation plan (HIPAA, IRB, i.e. informed consent, etc.) AND 2 bioethical principle considerations and how implementation of your plan impacts the principle (autonomy, beneficence, maleficence, justice).
- Assess: Include 2-3 measures that you will use to determine successful implementation. Measures must include: who, what, when, and how often. Metrics or benchmarks should be used to indicate the standard by which you know the measure has been met, i.e. 20%, 90% pass rate, etc.
Appendix for EBP Model
Strengths and Barriers
Strengths of the Implementation Plan
At least 3 strengths should be identified.
Barriers of the Implementation Plan
At least 3 strengths should be identified.