Primary Care adult – Herpes Zoster (Shingles)
Primary Diagnosis
Herpes Zoster (Shingles)
ICD-10 Code: B02.9 (Zoster without complications)
Clinical Practice Guideline
The guidelines provided by the Centres for Disease Control and Prevention (2024) for diagnosing and treating Herpes Zoster indicate that the reactivation of the varicella-zoster virus causes shingles. The patient has a burning, slightly itchy rash that is hypersensitive and follows a dermatomal pattern, which often occurs in patients with Herpes Zoster. The patient also had a history of varicella as a child and was not vaccinated for Herpes Zoster, which increases the likelihood of developing shingles.
Different Diagnoses
- Herpes Zoster (Shingles)
The key clinical presentations that led to choosing this differential are linear vesicular rash along a dermatome, a history of varicella, and the burning, hypersensitive sensation. This diagnosis was ruled in by considering the rash’s appearance and dermatomal distribution with burning and hypersensitivity because these symptoms suggest that the patient has Herpes Zoster. This diagnosis was ruled out because there were no systemic symptoms such as headache and fever, and the patient has a history of varicella.
- Contact Dermatitis
The key clinical presentation that led to choosing this differential is exposure to an insect or plant that could trigger a localized rash. This diagnosis was ruled out because contact dermatitis mainly presents with a rash not limited to one dermatome. The disease also lacks the vesicular, scabbed lesions.
- Cutaneous Reaction to Insect Bite
The key clinical presentations that led to choosing this diagnosis are the patient’s history of recent exposure to plants and insects and the localized hypersensitivity and rash. However, this diagnosis was ruled out because a reaction to an insect bite would not present with vesicular, scabbed lesions and would not follow a dermatome.
Management Plan
The patient’s condition can be managed using antiviral therapy, Acyclovir 800 mg PO, five times daily for 7–10 days. Antiviral treatment is most effective when initiated within 72 hours after the rash appears to reduce the severity and duration of symptoms. The patient should also be advised to take the medicine with plenty of water and finish the full dose even if the symptoms improve. The patient also needs ibuprofen 400 mg PO every 6 hours PRN to manage the pain. The patient should be advised to take the pain management medication with food to prevent stomach upset. The patient also needs lidocaine patches to control pain because the patches offer relief for neuropathic pain. Non-pharmacological treatment will include a cool compress to reduce the itching and enough hydration and rest to promote recovery. The patient may also require ancillary testing if systemic symptoms such as fever and headache occur and a referral to dermatology if there are complications or if the rash persists.
Social Determinants of Health
Socioeconomic status, access to healthcare facilities, living conditions, age, and community support networks all play important roles in influencing the risk of getting herpes zoster and the progression of the disease. Understanding how social variables affect the development, severity, and treatment outcomes of herpes zoster is critical for developing effective public health initiatives and interventions. Addressing these underlying socioeconomic issues allows healthcare practitioners to better customize preventative efforts and treatment programs to the specific requirements of high-risk individuals. Furthermore, including a social determinants perspective in herpes zoster management could greatly assist in eliminating discrepancies in healthcare outcomes and enhance overall health equality among those affected by the disorder. Notably, according to Meyers et al. (2018), individuals aged 50 years and above with Herpes Zoster spend $4000 more in all-cause healthcare expenses. Therefore, it is important to ensure that the patient has the financial capacity to meet all healthcare costs to manage his condition effectively.
Health Promotion
Health promotion plays a vital role in improving health outcomes. According to Rehman & Kanwal (2023), health promotion includes enabling people to have more control over their health and improve it. Health promotion in the current case will involve discussing the importance of getting vaccinated against herpes zoster to prevent future outbreaks. The patient should also be advised to receive the Shingrix vaccine after the current health issue is resolved to avoid future complications.
Risk Factors
The patient’s age is a key risk factor because, at 60 years, people develop a high likelihood of shingles because of reduced immunity. The patient’s history of varicella is also a significant risk factor because the virus could be reactivated, leading to future health complications.
Patient Education
Patient education plays a vital role in promoting positive health outcomes. According to Kirimlioğlu (2018), patient education helps patients learn and understand their diagnosis and treatment, leading to positive self-care attitudes. The first step in patient education is explaining that shingles are caused by the chicken pox virus reactivation, which remains dormant in the body. The second step is informing the patient that even though he cannot transmit shingles, he can transmit the varicella-zoster virus to others who have not been vaccinated and those who have not had chickenpox. The third step is advising the patient to avoid scratching the rash to prevent infection and emphasizing the need to use the prescribed medication as directed. The patient should also be advised to keep the rash dry and clean. The final step is recommending the Shingrix vaccine after recovery.
Follow-Up Instructions
It is recommended that the patient returns to the clinic after one week for a follow-up or within the shortest time possible if the rash worsens, if there are signs of infection such as increased pain, chills, or fever, and if there are new symptoms.
References
Centers for Disease Control and Prevention. (2024, July 9). Clinical overview of shingles (Herpes zoster). Shingles (Herpes Zoster). https://www.cdc.gov/shingles/hcp/clinical-overview/index.html
Kirimlioğlu, N. (2018). Patient education and its importance in terms of patient safety. International Journal of Research -GRANTHAALAYAH, 6(12), 109-120. https://doi.org/10.29121/granthaalayah.v6.i12.2018.1090
Meyers, J. L., Candrilli, S. D., Rausch, D. A., Yan, S., Patterson, B. J., & Levin, M. J. (2018). Cost of herpes zoster and herpes zoster-related complications among immunocompromised individuals. Vaccine, 36(45), 6810-6818. https://doi.org/10.1016/j.vaccine.2018.08.080
Rehman, F., & Kanwal, H. (2023). The importance of health promotion and disease prevention. COSMIC JOURNAL OF NURSING AND HEALTH STUDIES, 2(1). https://journals.cosmic.edu.pk/CJNHS/article/view/177
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Case studies
Client is 60 years old male, present to urgent care today for painful rash. PHM includes Osteoarthritis, Hypertension and Varicella as a child. Client reports burning, slightly itchy, hypersensitive rash. Physical examination reveals Linear, scabbed vesicular, hypersensitive rash with erythematous base, no right sided truncal or facial rash, no other rash on upper or lower extremities bilaterally, no purulence or streaking, and left T5 dermatomal pattern. Lack of herpes zoster vaccination noted. Client reported recent NSAID and neomycin with polymyxin use. Client reported exposure to plant and insect. Client denies fever, headache, nausea and vomiting.
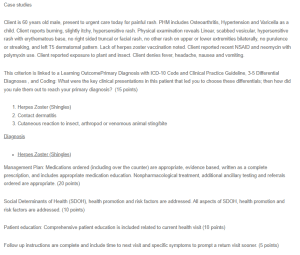
Primary Care adult – Herpes Zoster (Shingles)
This criterion is linked to a Learning OutcomePrimary Diagnosis with ICD-10 Code and Clinical Practice Guideline, 3-5 Differential Diagnoses , and Coding: What were the key clinical presentations in this patient that led you to choose these differentials; then how did you rule them out to reach your primary diagnosis? (15 points)
- Herpes Zoster (Shingles)
- Contact dermatitis
- Cutaneous reaction to insect, arthropod or venomous animal sting/bite
Diagnosis
- Herpes Zoster (Shingles)
Management Plan: Medications ordered (including over the counter) are appropriate, evidence based, written as a complete prescription, and includes appropriate medication education. Nonpharmacological treatment, additional ancillary testing and referrals ordered are appropriate. (20 points)
Social Determinants of Health (SDOH), health promotion and risk factors are addressed. All aspects of SDOH, health promotion and risk factors are addressed. (10 points)
Patient education: Comprehensive patient education is included related to current health visit (10 points)
Follow up instructions are complete and include time to next visit and specific symptoms to prompt a return visit sooner. (5 points)

