Hispanic American Cultural Beliefs
Several culturally motivated beliefs guide an individual’s perspective on life, disease, and death and, therefore, impact choices related to health care, specifically end-of-life decisions. To a health professional, these beliefs provide a means to offer sympathetic and culturally competent care. Regarding terminal disease and death, certain beliefs and customs are of particular importance to Hispanic Americans, who center life on family, faith, and tradition. This paper discusses these cultural beliefs and compares them with those of African Americans, a culture similarly steeped in solid values about health care delivery. A case is made for incorporating cultural knowledge within nursing practice as an essential component of holistic care.
Hispanic American Beliefs and Practices Surrounding Terminal Illness and Death
Hispanic Americans claim their origins from numerous nations in Latin America. Family, faith, and spirituality are some of the fundamental values that are deemed necessary when considering life processes like terminal illness and death (Barragan-Carrillo et al., 2022). These core values are essential to healthcare decision-making, as most decisions are made in a communal manner where the family, including the extended members, is directly involved in caregiving and decision-making.
The Role of Religion and Spirituality
Religion, particularly Catholicism, is primarily one of the prime elements in Hispanic American notions about terminal illness and death. It forms their perception about diseases and dying through the belief in an afterlife, God’s will, and prayer. Many believe suffering has a divine purpose, and death is not the end but a transit to eternal life. As such, this often makes Hispanic Americans more accepting of terminal illness and, in their reluctance or refusal to seek aggressive treatments aimed at prolonging suffering. Comfort measures, such as hospice care, along with spiritual support in the way of reciting prayers or blessings from family members or religious leaders, are considered more important and are usually favored over medical interventions attempting to extend life.
Spiritual support, though comforting, may be an integral part of the end-of-life experience for many Hispanic American families. Religious rituals, including prayer, sacraments, or blessings, may be essential to the patient’s and family’s coping with the emotional and spiritual challenges of a terminal illness, as stated by Miller et al. (2023). Healthcare providers must acknowledge the importance of these rituals and ensure access to spiritual support through chaplains or community religious leaders.
Family-Centered Decision Making
In Hispanic American culture, the family is central during illness or death, with healthcare decisions made by family consensus rather than individual autonomy, contrasting with Western values. This may involve “benevolent deception,” where the family shields the patient from the full extent of their illness to prevent emotional distress. These practices reflect collectivist values, prioritizing the family’s well-being over individual needs. Accordingly, healthcare providers must recognize these cultural dynamics and involve the family in discussions to ensure care decisions align with cultural values and maintain family harmony.
Death and Dying Rituals
Hispanic Americans continue many culturally significant rituals regarding death as a way to honor the dead and console the bereaved. Funerals are often large family gatherings; friends also provide support. Many families will also hold novenas, praying for nine consecutive days after a death, reflecting deep religiosity and solace. These rituals serve religious and emotional purposes, helping the grieving process by situating them in a comfort zone. Therefore, it is essential that health professionals respect these traditions and that families be given the opportunity and privacy to do so without interruption (Tariq & Hackert, 2023). Recognition of these practices may be imperative, as well as inappropriately offering appropriate support to a family in their grief.
Comparison with African American Beliefs
Although both Hispanic Americans and African Americans base their EOL care on family and religion, the strategies employed by each culture are unique and varied. Many African American families, because of historical injustices and mistrust of the healthcare system, may desire more aggressive treatments, hoping for a cure for their loved ones even when the diagnosis is terminal. Many religious beliefs include a strong emphasis on divine intervention and miracle healing; thus, life-prolonging treatments are focused on. While the majority of other cultures concentrate on providing a peaceful and culturally significant transition rather than aggressive interventions, for example, it is reversed for Hispanic American families, who endorse comfort and spiritual support during dying.
The Role of Healthcare Workers
Healthcare workers, especially nurses, also have a vital role in giving culturally competent care to patients who are Hispanic American. The involvement of family members in decisions about one’s care is essential for delivering effective care; likewise, cultural beliefs, as supported by a patient, must be respected, as stated by Kuipers et al. (2019). Instead, rapport building between the patient and oneself and the family is fundamental for a mutual bond of trust, leading to adequate healthcare delivery.
Addressing Language Barriers
One of the most prevalent possible barriers in the care of Hispanic American patients by healthcare workers includes language barriers. Most Hispanic Americans may prefer to converse in Spanish, especially those of older age or fresh immigrants. Healthcare staff should ensure interpreters are provided, as well as written materials in the patient’s preferred language. Essentially, effective communication ensures that active patients and their families fully understand a diagnosis, treatment options, and a contemplated care plan.
Providing Spiritual Support
Since religion is central to Hispanic American culture, healthcare professionals should be prepared to offer spiritual support or facilitate reaching religious services for patients. This may include arranging for a priest or chaplain to visit the patient, say prayers with the patient and family, or provide space for religious observances. Spiritual care can significantly add to the experience of both the patient and the family, especially during end-of-life care, as asserted by García-Navarro et al. (2021). The nurse and other health professionals should support the patient and their families by participating in cultural rituals and practices that offer comfort.
Incorporating Cultural Knowledge into Nursing Practice
The knowledge obtained in learning about the Hispanic American cultural beliefs and practices in this chapter can then be assimilated into nursing practice by providing culturally competent care. Notably, culturally competent care includes acknowledging and valuing the patient’s cultural beliefs about their lifestyle. For example, cultural competence ensures the healthcare provider examines the family’s involvement in a client’s healthcare decision, the place of religion/spirituality in the process, and the cultural practices of the client’s end-of-life care.
Culturally Competent Care
Culturally relevant treatment is administering medical care that is in harmony with the patient’s culture. Family, spirituality, and cultural aspects are important in enhancing patients’ trust, which are ways to embrace them (Stubbe, 2020). This involves the mobilization of the family in managing care and decision-making for the client, spiritual support, and permitting religious practices in the care planning if the Hispanic-American client is a religious person.
Advocacy for Patients and Families
Nurses are influential in assisting patients and their families through advocacy and making care plans culturally appropriate. This may include collaborating with healthcare teams to decide when comfort care is more important than invasive measures or supporting providing interpretive services and culturally relevant educational materials. This will ensure their care is closer to their culture since nurses engage patients and their loved ones in making the best decisions.
Conclusion
Health professionals must be aware of the Hispanic American cultural beliefs about terminal illness, as family, religion, and spirituality are enormously influential in decision-making. The core of decision-making in the Hispanic culture is the family, with religious and spiritual beliefs. If culturally competent care is to serve the wishes of the patient and his family, recognition and respect for these beliefs are essential. These compare to African American beliefs, which may be geared more toward faith and divine intervention while they struggle to mistrust the health care system. Understanding these, but comparing them to other cultures, such as African Americans, extends one’s view on the cultural concept of death and guides health care providers to culturally competent care for these values, thus building trust, ensuring quality, and providing holistic, non-judgmental care to the patients and their family through end-of-life care.
References
Barragan-Carrillo, R., Pabon, C. M., Chavarri-Guerra, Y., Soto-Perez-de-Celis, E., & Duma, N. (2022). End-of-life care and advanced directives in Hispanic/Latinx patients: Challenges and solutions for the practicing oncologist. The Oncologist, 27(12), 1074–1080. https://doi.org/10.1093/oncolo/oyac211
García-Navarro, E. B., Medina-Ortega, A., & García Navarro, S. (2021). Spirituality in patients at the end of life—is it necessary? A qualitative approach to the protagonists. International Journal of Environmental Research and Public Health, 19(1), 227. https://doi.org/10.3390/ijerph19010227
Kuipers, S. J., Cramm, J. M., & Nieboer, A. P. (2019). The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Services Research, 19(13), 1–9. https://doi.org/10.1186/s12913-018-3818-y
Miller, M., Addicott, K., & Rosa, W. E. (2023). Spiritual care as a core component of palliative nursing. AJN the American Journal of Nursing, 123(2), 54. https://doi.org/10.1097/01.NAJ.0000919748.95749.e5
Stubbe, D. E. (2020). Practicing cultural competence and cultural humility in the care of diverse patients. Focus, 18(1), 49–51. https://doi.org/10.1176/appi.focus.20190041
Tariq, R. A., & Hackert, P. B. (2023). Patient confidentiality. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519540/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
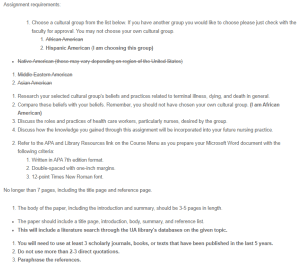
Assignment requirements:
-
- Choose a cultural group from the list below. If you have another group you would like to choose please just check with the faculty for approval. You may not choose your own cultural group.
- African American
- Hispanic American (I am choosing this group)
Hispanic American Cultural Beliefs
- Choose a cultural group from the list below. If you have another group you would like to choose please just check with the faculty for approval. You may not choose your own cultural group.
- Native American (these may vary depending on region of the United States)
- Middle Eastern American
- Asian American
- Research your selected cultural group’s beliefs and practices related to terminal illness, dying, and death in general.
- Compare these beliefs with your beliefs. Remember, you should not have chosen your own cultural group. (I am African American)
- Discuss the roles and practices of health care workers, particularly nurses, desired by the group.
- Discuss how the knowledge you gained through this assignment will be incorporated into your future nursing practice.
- Refer to the APA and Library Resources link on the Course Menu as you prepare your Microsoft Word document with the following criteria:
- Written in APA 7th edition format.
- Double-spaced with one-inch margins.
- 12-point Times New Roman font.
No longer than 7 pages, including the title page and reference page.
- The body of the paper, including the introduction and summary, should be 3-5 pages in length.
- The paper should include a title page, introduction, body, summary, and reference list.
- This will include a literature search through the UA library’s databases on the given topic.
- You will need to use at least 3 scholarly journals, books, or texts that have been published in the last 5 years.
- Do not use more than 2-3 direct quotations.
- Paraphrase the references.