Off-Label Drug Use for Children
The pharmacodynamics and pharmacokinetics characteristics in children change as they develop. These characteristics include metabolism, distribution, and absorption of drugs. The clearance of drugs from the body also changes and is influenced by liver maturity, enzyme deficiency, gastrointestinal motility, and pH fluctuations. Most drugs that are prescribed to children have not undergone any testing for their efficacy and safety in children. These, too, are supported by often low-quality evidence. Hence, most drugs that are prescribed to children are on an unlicensed or off-label basis (Gore et al., 2017)
Circumstances Under Which Children Should Be Prescribed Drugs for Off-Label Use
Gore et al. (2017) point out that one of the reasons that medicines are prescribed off-label for children is the absence or non-availability of safe, effective, licensed, and standard therapeutic options for specific conditions and also the inconsistent or absent information available to pediatricians on the same. Other reasons include standard therapy failure; a lack of other drug forms for specific age groups’ therapy; and a lack of available clinical trials involving special groups such as pregnant women, infants, or neonates. Another reason is the availability of evidence that is convincing enough for safe and effective application for specific health conditions.
Strategies to Make the Off-Label Use and Dosage of Drugs Safer For Children from Infancy to Adolescence
The decision to use off-label medication should be based on scientific evidence, controlled trials, or medical opinions from experts (Ito, 2015). Also, a physician should be aware of all the package insert contents and consider warnings, contraindications, and precautions (Balan, Hassali, & Mak, 2017). Additionally, a target-effective strategy should be adopted where the dosage is given to a patient until the desired effect is realized or the risk of toxicity occurs. Lee et al., (2018) add that one way of doing so is to give the pediatric patient an adult dose that is divided by 60 and then multiplied by the weight of the patient to the 0.7th power; and dependent on the child’s weight and age for specific drug classes. For example, antibiotics should be prescribed based on the disease-causing organism; tetracycline should be given to children aged 7 and above. Combination therapy can also be used for the treatment of specific diseases such as S. viridians endocarditis that require an aminoglycoside and penicillin.
In conclusion, off-label drugs need to be prescribed with much caution. Physicians should use evidence-based information to back their use of such drugs. All measures need to be taken to avoid adverse drug effects.
References
Balan, S., Hassali, M. A., & Mak, V. S. L. (2017). Challenges in pediatric drug use: A pharmacist point of view. Research in Social and Administrative Pharmacy, 13(3), 653-655.
Gore, R., K Chugh, P., D Tripathi, C., Lhamo, Y., & Gautam, S. (2017). Pediatric off-label and unlicensed drug use and its implications. Current clinical pharmacology, 12(1), 18-25.
Ito, S. (2015). Children: are we doing enough? Clinical Pharmacology & Therapeutics, 98(3), 222-224.
Lee, J. H., Byon, H. J., Choi, S., Jang, Y. E., Kim, E. H., Kim, J. T., & Kim, H. S. (2018). Safety and Efficacy of Off-label and Unlicensed Medicines in Children. Journal of Korean Medical Science, 33(37).
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
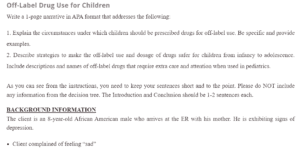
Off-Label Drug Use for Children
Write a 1-page narrative in APA format that addresses the following:
- Explain the circumstances under which children should be prescribed drugs for off-label use. Be specific and provide examples.
- Describe strategies to make the off-label use and dosage of drugs safer for children from infancy to adolescence. Include descriptions and names of off-label drugs that require extra care and attention when used in pediatrics.
As you can see from the instructions, you need to keep your sentences short and to the point. Please do NOT include any information from the decision tree. The Introduction and Conclusion should be 1-2 sentences each.
Off-Label Drug Use for Children
BACKGROUND INFORMATION
The client is an 8-year-old African American male who arrives at the ER with his mother. He is exhibiting signs of depression.
- Client complained of feeling “sad”
- The mother reports that teacher said child is withdrawn from peers in class
- The mother notes decreased appetite and occasional periods of irritation
- The client reached all developmental landmarks at appropriate ages
- Physical exam unremarkable
- Laboratory studies WNL
- Child referred to psychiatry for evaluation
MENTAL STATUS EXAM
Alert & oriented X 3, speech clear, coherent, goal-directed, spontaneous. The self-reported mood is “sad”. Affect somewhat blunted, but child smiled appropriately at various points throughout the clinical interview. He denies visual or auditory hallucinations. No delusional or paranoid thought processes noted. Judgment and insight appear to be age-appropriate. He is not endorsing active suicidal ideation, but does admit that he often thinks about himself being dead and what it would be like to be dead.
You administer the Children’s Depression Rating Scale, obtaining a score of 30 (indicating significant depression)
RESOURCES
§ Poznanski, E., & Mokros, H. (1996). Child Depression Rating Scale–Revised. Los Angeles, CA: Western Psychological Services.
DECISION TREE
- Decision Point One
-
- Begin Zoloft 25 mg orally daily
- RESULTS OF DECISION POINT ONE
- The client returns to the clinic in four weeks
- No change in depressive symptoms at all
- RESULTS OF DECISION POINT ONE
- Begin Zoloft 25 mg orally daily
- Decision Point Two
-
- Increase the dose to 50 mg orally daily
- RESULTS OF DECISION POINT TWO
- The client returns to the clinic in four weeks
- Depressive symptoms decrease by 50%. Client tolerating well
- RESULTS OF DECISION POINT TWO
- Increase the dose to 50 mg orally daily
- Decision Point Three
- Increase to 75 mg orally daily
Guidance to Student
At this point, sufficient symptom reduction has been achieved. This is considered a “response” to therapy. Can continue with current dose for additional 4 week to see if any further reductions in depressive symptoms are noted. An increase in dose may be warranted since this is not “full” remission- Discuss pros/cons of increasing drug dose with client at this time and empower the client to be part of the decision. There is no indication that the drug therapy should be changed to an SNRI at this point as the client is clearly responding to this therapy.

