Evidence-Based Patient-Centered Concept Map and Narrative
Concept Map Narrative
A concept map is an essential tool that is used in the planning of patient care. It is instrumental in the patient’s complex economic, health, and cultural needs (Pishgooie et al., 2019). This concept paper was developed for Keith Rodgeris, an 18 old-year African American. Keith is a recent high school graduate diagnosed with HIV but has never been treated. Following this scenario, a concept map was developed to address Keith’s issue while considering his economic, health, and cultural needs. Our assignment writing services will allow you to attend to more important tasks as our experts handle your task.
The Patient And Their Family’s Needs And How Those Needs Will Influence A Patient-Centered Concept Map
In the interview, Keith said that he and his friend Nick turned positive during the summer when they got tested. He was given information pamphlets but could not leave them around the house. His parents did not know about their HIV status, so he threw the pamphlets away. All this happened six months ago. His friend, Nick, read on the internet that meth helps in HIV since it slows disease progression. He thinks this illicit drug is working; on the contrary, the drug is giving him tachycardia. Keith believes Nick would be mad if he knew he had revealed that information. However, Keith no longer cares since he thinks they will soon be discovered. To ensure that Keith adheres to the regimen chosen, his ability to afford this must be discussed; his mum threw him out, and he is now living with his friend Nick.
Justification Of The Value And Relevance Of The Evidence Used As The Basis Of The Concept Map
Evidence-based practice (EBP) improves the patient’s health condition since the evidence shows that it enables healthcare professionals to develop a patient care plan while considering the patient’s needs and cultural beliefs. Evidence-based practice (EBP) applies critical thinking, experimental facts, and the caregiver’s experience (Kirby, 2017).
In this case, the main issue is the risk of Keith’s condition progressing to full-blown HIV due to a lack of treatment with Antiretrovirals (ARVs) (Welch et al., 2020). Keith has HIV but cannot access treatment since he feels HIV drugs are expensive. In addition, he is currently homeless after being thrown out of their house by his mother; hence he lacks financial support. Lastly, he threw away the HIV pamphlet, which could be a great source of information, while his friend Nick convinced him that meth helps with the management of HIV. So lack of information and cost implications appear to be critical factors in choosing a treatment plan for Keith.
To ensure Keith’s situation is handled well, it is critical to analyze his lack of social support network, as evidenced by a lack of family support since her mother threw him out of the house. Keith is at a higher risk of falling into depression since he does not feel loved, which could affect the prognosis of HIV and can affect medication adherence. Keith’s family should be convinced to take him back to their home to provide moral and emotional support. He should also be educated that meth does not treat HIV. In addition, the family should be educated that HIV is not spread by sharing utensils and bedding.
Relevant And Measurable Criteria For Evaluating The Degree To Which The Concept Map’s Desired Outcomes Were Achieved
Keith needs to be put on ARVs therapy (Welch et al., 2020). He should also start living a healthy lifestyle, such as adhering to a well-balanced diet and engaging in regular exercise, which helps in the management of HIV. Keith should also consistently take ARV medication without fail since this will lead to a poor prognosis; Keith’s viral load will be assessed in the next clinical visit.
How To Communicate Specific Aspects Of The Concept Map To Patients And Their Family In An Ethical, Culturally Sensitive, And Inclusive Way
Keith should meet his healthcare giver to ensure that his concept map is adequately understood. The primary concerns that should be considered by the healthcare provider are Keith’s family and background. Keith’s mother believes that homosexuality is a sin, and hence he throws him out. The caregiver needs to explain to Keith the importance of strictly following the laid down treatment plan, HIV may not have a cure, but one can live with the virus for an extended period when on medications. The healthcare giver needs to assess his economic needs since the patient feels that he does not have enough money to cover his treatment cost and that insurance cannot cover the treatment costs given that he has a terminal illness (Kühnert et al., 2018).
Conclusion
The concept map will help Keith understand his disease’s prognosis, factors that may negatively affect the disease progression, and his strict conformance to the treatment plan. By knowing Keith’s medical needs, the caregiver will develop a trustworthy relationship with the patient. Lastly, by understanding the patient’s economic and social background, the caregiver will develop a care plan specific to this patient.
Concept Map
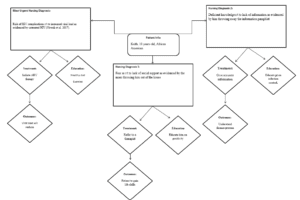
Concept Map
References
Kirby, J. N. (2017). Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychology and Psychotherapy: Theory, Research and Practice, 90(3), 432-455.
Kühnert, D., Kouyos, R., Shirreff, G., Pečerska, J., Scherrer, A. U., Böni, J., … & Swiss HIV Cohort Study. (2018). Quantifying the fitness cost of HIV-1 drug resistance mutations through phylodynamics. PLoS pathogens, 14(2), e1006895.
Pishgooie, A. H., Abdi, A., Mazhari, M. S., & Nazari, M. R. (2019). Comparing two teaching methods based on a concept map and lecture on the level of learning in basic life support. Nurse education in practice, 38, 40-44.
Welch, J. L., Kaddour, H., Winchester, L., Fletcher, C. V., Stapleton, J. T., & Okeoma, C. M. (2020). Semen extracellular vesicles from HIV–1–infected individuals inhibit HIV-1 replication in vitro, and extracellular vesicles carry antiretroviral drugs in vivo. JAIDS Journal of Acquired Immune Deficiency Syndromes, 83(1), 90-98.
Nowak, R. G., Bentzen, S. M., Ravel, J., Crowell, T. A., Dauda, W., Ma, B., … & Charurat, M. E. (2017). Rectal microbiota among HIV-uninfected, untreated HIV, and treated HIV-infected men who have sex with men (MSM) in Nigeria. AIDS (London, England), 31(6), 857.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Evidence-Based Patient-Centered Concept Map and Narrative
Overview:
Create an evidence-based, patient-centered concept map that illustrates an individualized approach to patient care, based on a patient case file of your choice.
Evidence-based practice is a key skill in the toolkit of the master’s-prepared nurse. Its goal is to ensure that healthcare practitioners are using the best available evidence to ensure that patients are receiving the best care possible (Godshall, M., 2015.). In essence, evidence-based practice is all about ensuring quality care.
Evidence-Based Patient-Centered Concept Map and Narrative
In this assessment, you have an opportunity to apply evidence-based practice and personalized care concepts to ensure quality care and improve the health of a single patient.
Competencies:
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
- Competency 1: Apply evidence-based practice to plan patient-centered care.
- Analyze the needs of a patient, and those of their family, with regard to how they will influence a patient-centered concept map.
- Design an individualized, patient-centered concept map, based upon the best available evidence for treating a patient’s specific health, economic, and cultural needs.
- Competency 3: Evaluate outcomes of evidence-based interventions.
- Propose relevant and measurable criteria for evaluating the outcomes of a patient-centered concept map.
- Competency 4: Evaluate the value and relative weight of available evidence upon which to make a clinical decision.
- Justify the value and relevance of evidence used as the basis of a patient-centered concept map.
- Competency 5: Synthesize evidence-based practice and academic research to communicate effective solutions.
- Develop a strategy for communicating with patients and their families in an ethical, culturally sensitive, and inclusive way.
- Integrate relevant and credible sources of evidence to support assertions, correctly formatting citations and references using APA style.
******************************
Questions to Consider:
As you prepare to complete this assessment, you may want to think about other related issues to deepen your understanding or broaden your viewpoint. You are encouraged to consider the questions below and discuss them with a fellow learner, a work associate, an interested friend, or a member of your professional community. Note that these questions are for your own development and exploration and do not need to be completed or submitted as part of your assessment.
Recall an experience you have had—or one that you might have observed in your care setting—in which you individualized care for a patient.
- In your approach to individualized care, did you:
- Address any health concerns other than those for which the patient was seeking care.
- Consider the patient’s economic and daily environmental circumstances.
- Consider any ethical issues inherent in working with the patient.
- What might you have done differently, if you could revisit that patient’s case?
- What evidence supported your original course of action?
- What evidence would you present to support an alternative course of action, if you could revisit that patient’s case?
******************************
Required Resources
The following resources are required to complete the assessment.
Evidence-Based Practice
- Evidence-Based Patient-Centered Care | Transcript. (see transcript attached)
Suggested Resources
The resources provided here are optional. You may use other resources of your choice to prepare for this assessment; however, you will need to ensure that they are appropriate, credible, and valid. The MSN-FP6011 – Evidence-Based Practice for Patient-Centered Care and Population Health Library Guide can help direct your research, and the Supplemental Resources and Research Resources, both linked from the left navigation menu in your course, provide additional resources to help support you.
Evidence-Based Practice
- Godshall, M. (2015). Fast facts for evidence-based practice in nursing: Implementing EBP in a nutshell (2nd ed.). New York, NY: Springer Publishing Company.
- Read Chapter 7.
- Blix, A. (2014). Personalized medicine, genomics, and pharmacogenomics: A primer for nurses. Clinical Journal of Oncology Nursing, 18(4), 437–441.
- Baker, J. D. (2017). Nursing Research, Quality Improvement, And Evidence-Based Practice: The Key To Perioperative Nursing Practice: Editorial. Association of Operating Room Nurses, 105(1), 3.
- Hain D. J., & Kear, T. M. (2015). Using evidence-based practice to move beyond doing things the way we have always done them. Nephrology Nursing Journal, 42(1), 11–20.
- Evidence-Based Practice in Nursing & Health Sciences: Review Levels of Evidence.
- Evidence-Based Practice in Nursing & Health Sciences.
- Evidence-Based Practice: What It Is and What It Is Not | Transcript.
Concept Mapping
- Concept Maps.
- This resource provides a general overview of concept maps. The guide is not specific to nursing but may prove helpful to the initial conceptualization of your assessment.
- Taylor, L. A., Littleton-Kearney, M. (2011). Concept mapping: A distinctive educational approach to foster critical thinking. Nurse Educator, 36(2), 84–88.
- This article will help you decide how you would like to structure and conceptualize your concept map.
- Concept Map Template [DOCX].
- Concept Map Tutorial | Transcript.
- Information on working with the concept map and template to complete your assignment.
Research Guides
- Nursing Masters (MSN) Research Guide.
- Database Guide: Ovid Nursing Full Text PLUS.
- Kaplan, L. (n.d.). Framework for how to read and critique a research study. Retrieved from https://www.nursingworld.org/~
4afdfd/globalassets/ practiceandpolicy/innovation– evidence/framework-for-how-to- read-and-critique-a-research- study.pdf
******************************
Assessment Instructions:
Preparation
You have been presented with a number of patient case files in the Evidence-Based Patient-Centered Care media piece. You reviewed each case, selected one case for further research, and created a draft evidence-based concept map to illustrate an approach to individualized care for the patient. In this assessment, you will build upon and refine your draft concept map and develop a supporting narrative.
Create your concept map and narrative as separate documents. Be sure to note the areas where you need to include your evidence-based support and where you need to make clear your strategies for communicating information to the patient and the patient’s family.
Note: Many organizations use the spider style of concept maps (see the Taylor & Littleton-Kearney article for an example). Also, if a specific style of concept map is used in your current care setting, you may use it in this assessment.
Create your concept map and narrative as separate documents. Be sure to note the areas where you need to include your evidence-based support and where you need to make clear your strategies for communicating information to the patient and the patient’s family.
Note: The requirements outlined below correspond to the grading criteria in the scoring guide, so be sure to address each point. In addition, you may want to review the performance level descriptions for each criterion to see how your work will be assessed.
Integrate relevant evidence from 3–5 current scholarly or professional sources to support your assertions.
- Apply correct APA formatting to all in-text citations and references.
- Attach a reference list to your narrative.
Concept Map
- Develop a concept map for the individual patient, based on the best available evidence for treating your patient’s health, economic, and cultural needs.
Narrative
Develop a narrative (2–4 pages) for your concept map.
- Analyze the needs of your patient and their family, and determine how those needs will influence a patient-centered concept map.
- Consider how your patient’s economic situation and relevant environmental factors may have contributed to your patient’s current condition or affect their future health.
- Consider how your patient’s culture or family should influence your concept map.
- Justify the value and relevance of the evidence you used as the basis of your concept map.
- Explain why your evidence is valuable and relevant to your patient’s case.
- Explain why each piece of evidence is appropriate for both the health issue you are trying to correct and for the unique situation of your patient and their family.
- Propose relevant and measurable criteria for evaluating the degree to which the desired outcomes of your concept map were achieved.
- Explain why your proposed criteria are appropriate and useful measures of success.
- Explain how you will communicate specific aspects of the concept map to your patient and their family in an ethical, culturally sensitive, and inclusive way. Ensure that your strategies:
- Promote honest communications.
- Facilitate sharing only the information you are required and permitted to share.
- Are mindful of your patient’s culture.
- Enable you to make complex medical terms and concepts understandable to your patient and their family, regardless of language, disabilities, or level of education.
Additional Requirements
- Be sure to include both documents when you submit your assessment.

