Initial Psychiatric SOAP Note – Patient with Generalized Anxiety Disorder
| Criteria | Clinical Notes |
| Informed Consent | Informed consent was given to the patient about the psychiatric interview process and psychiatric/psychotherapy treatment. Verbal and Written consent were obtained. The patient has the ability/capacity to respond and appears to understand the risks, benefits, and (Will review additional consent during treatment plan discussion) |
| Subjective | Verify Patient
Name: Allen DOB: 11/10/2022 Demographic: The client is a 21-year-old male. He is a university graduate. Gender Identifier Note: Male CC: The client presented to the clinic with complaints of worry about the palpitations he has been feeling. HPI: The client is a 21-year-old male who worries about palpitations. These palpitations start whenever he is anxious. These presentations occur most days of the week and often make him feel on edge. Pertinent history in the record and from the patient: The client noted that his anxiety is affecting how he sleeps. He also reports not wanting to socialize with others. Additionally, he reported experiencing chest pain occasionally. During assessment: The client noted that his symptoms are affecting his social wellness and making him feel on edge. The patient’s self-esteem appears fair. There were no reports of lowered self-esteem, loss of interest in otherwise pleasurable activities, or feelings of hopelessness and worthlessness. There were also no reports of appetite changes, memory loss, or difficulty in concentration. The client, however, reported sleep disturbances. Allergies: The client has no known drug or food allergies. Past Medical Hx: There were no reports of past hospitalizations or history of head injuries, accidents, or surgeries. There were also no reports of any cardiac, respiratory, or endocrine disorders. The client also denied having a history of chronic infections. Social history revealed that the client is a graduate. There were no reports of tobacco or alcohol use. There were also no reports of exposure to violence, the client’s background and socioeconomic status. His family history is negative for any genetic illnesses and diseases running along the family line. The client is socially isolated and reported that he does not want to talk to anyone. There were no reports of the client’s nutritional health, including his observation of a balanced diet, daily nutritional intake, and what he ate before presenting to the clinic. Past Psychiatric Hx: There were no reports of any psychiatric illnesses. Previous medication trials: There were no reports of previous medication use. Safety concerns: There were no reports of violence, suicidal ideation and tendencies, or any behavior that may predispose the client to self-harm. There were also no reports of any auditory or visual hallucinations. Mental health treatment history: The client has a negative history of outpatient treatment or hospitalization for any mental health illness. There were also no reports of substance use. Trauma history: There were no reports of any form of trauma currently and in the past. Current Medications: There are no reports of current medications. Past Psych Med Trials: There are no reports of past use of psychotropic medications. Family Medical Hx: There were no reports of past and current use of medications among the client’s family members. Family Psychiatric Hx: There were no reports of substance use, suicidal ideation or tendencies, hospitalizations attributed to mental health disorders, hospitalization attributed to somatic illnesses, and developmental disorders among the client’s family members. Social History: Occupational History: The client is a graduate. Military Service History: The client denied having served in the military. Education history: The client is a graduate. He also has a vocational certificate. Developmental History: No reports of any developmental disorders or health issues. Legal History: There were no reported legal issues. Spiritual/Cultural Considerations: There were no reported spiritual and cultural concerns. ROS: Constitutional: No report of fever or weight loss. Eyes: No report of visual changes or eye pain. ENT: No report of hearing changes or difficulty swallowing. Cardiac: The client reported palpitations and chest pain. Respiratory: Denies dyspnea, cough, or wheezing. GI: No report of abdominal pain. GU: No report of dysuria or hematuria. Musculoskeletal: No report of joint pain or swelling. Skin: The client reported sweating. Neurologic: No report of seizures, blackout, numbness, or focal weakness. Endocrine: No report of polyuria or polydipsia. Hematologic: No report of blood clots or easy bleeding. Allergy: No report of hives or allergic reaction. Reproductive: No report of significant issues. |
| Verify the patient’s name, assigned identification number (e.g., medical record number), date of birth, phone number, social security number, address, and photo.
Include demographics, chief complaint, subjective information from the patient, names, and relations of others present in the interview. HPI: Past Medical and Psychiatric History, Current Medications, Previous Psych Med trials, Allergies. Social History, Family History. Review of Systems (ROS) – if ROS is negative, “ROS noncontributory,” or “ROS negative with the exception of…” |
|
| Objective | Vital Signs: Stable. He is visibly sweating.
Temp: BP:138/80 HR: 78 bpm R:20 bpm O2: 99% Pain: Occasional chest pain-not quantified. Ht: 5’10” Wt: 188 lbs. BMI:27kg/m2 BMI Range: Overweight LABS: Lab findings N/A Tox screen: Negative Alcohol: Negative HCG: N/A Physical Exam: MSE: The client is cooperative and oriented to place time, and event. He is dressed appropriately, maintains eye contact, and demonstrates normative and goal-directed speech and affect. His judgment is also fair and insightful. The patient can articulate his needs and is motivated to comply and adhere to the medication regimen. The patient is willing and able to participate in treatment, disposition, and discharge planning. Diagnostic testing: Generalized anxiety disorder (GAD-7) tool. GAD-7 is a valuable tool in the screening for anxiety disorders. It helps in assessing symptom severity and the presence of an anxiety disorder. The client scored 10, indicating moderate anxiety. |
| This is where the “facts” are located.
Vitals, **Physical Exam (if performed, will not be performed every visit in every setting) Include relevant labs, test results, and Include MSE, risk assessment here, and psychiatric screening measure results. |
|
| Assessment | DSM5 Diagnosis: with ICD-10 codes
Dx: Generalized anxiety disorder F41.9, denoting unspecified anxiety disorders. The client presented with symptoms of anxiety. The assessment findings revealed that his anxiety resulted in functional impairments and was associated with sleep disturbances. Additionally, he was unable to control his anxiety, as evidenced by his health-seeking behavior. As per the fifth version of the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-V), a positive diagnosis of GAD is made in the presence of intense and uncontrollable worry. In addition, this presentation must have resulted in functional impairment (Mishra & Varma, 2023). The client’s manifestations were consistent with those detailed in the DSM-V warranting the GAD diagnosis. Dx: Panic disorder-F41.0. This differential was warranted because of the manifestations of intense worry and palpitation. It was, however, ruled out because of a lack of spontaneity and that the anxiety manifestations seen in the case were presented for many days of the week. Dx: Bipolar disorder-F31.4. This differential was also warranted because of the presence of anxiety symptoms and palpitations. Palpitations and anxiety are common presentations in the manic and hypomanic phases of bipolar disorders. However, this differential was ruled out because of the absence of supportive evidence of depressed mood, suggestive of the depressive phase of bipolar, from the subject findings. The diagnostic impression is a moderate generalized anxiety disorder. The patient has the ability/capacity to respond to psychiatric medications/psychotherapy. He appears to understand the need for medications/psychotherapy and is willing to maintain adherence. Reviewed potential risks and benefits, Black Box warnings, and alternatives including declining treatment. |
| Include your findings, diagnosis and differentials (DSM-5 and any other medical diagnosis) along with ICD-10 codes, treatment options, and patient input regarding treatment options (if possible), including obstacles to treatment.
Informed Consent Ability |
|
| Plan | Pharmacotherapy
Pharmacotherapy using anti-anxiety medications maintains significance in the management of moderate to severe anxiety disorders. These agents help in lessening the severity of anxiety symptoms. Selective serotonin reuptake inhibitors (SSRIs), buspirone, and benzodiazepines are available therapeutic options for patients with anxiety disorders. These medications are equally effective in managing anxiety disorders. In this case, the client can benefit from fluoxetine, an SSRI. He will be initiated on fluoxetine 5mg, administered orally every 24 hours. Psychotherapy The client will be scheduled for psychotherapy sessions. He will be initiated on individualized cognitive behavioral therapy (CBT) to help him identify his thought processes that may be contributing to his presentation. The therapists will then work with the client to help him correct these thought processes. CBT is a psychotherapeutic technique that maintains effectiveness in the management of anxiety disorders (Krzikalla et al., 2023). This modality can be used alongside pharmacotherapy in the comprehensive management of clients with severe manifestations of anxiety disorder. Referral The client will be referred to a cardiologist for the assessment of potential cardiovascular illnesses. As evident in the case presented, the client reported chest pain and palpitations. While these manifestations are typical of the physical manifestations of anxiety, they may also be suggestive of other cardiovascular diseases. Cardiovascular assessment by a cardiologist may help eliminate any underlying cardiovascular disease. Education As part of the holistic management and health promotion of the client, he will be educated on the disease processes and interventions that may help lessen anxiety manifestations. In this respect, the client will be educated on the significance of exercise in managing anxiety. As Kandola and Stubbs (2020) report, exercise helps lower anxiety symptoms. He will also be educated on dietary considerations that may help in alleviating anxiety symptoms. For instance, cutting down on caffeine consumption lowers anxiety manifestations (Klevebrant & Frick, 2022). He will also be advised to avoid or quit tobacco use. As part of the complementary approach to holistic care, the client will be advised to consider medication as a strategy to enhance relaxation. Follow-up: The client will visit the clinic after two weeks for follow-up. Time spent in Psychotherapy: 18 minutes The visit lasted 30 minutes Billing Code for a visit: 99204 90791 ____________________________________________ NAME, TITLE Date: 12/13/23 Time: 1100hrs |
| Include a specific plan, including medications & dosing & titration considerations, lab work ordered, referrals to psychiatric and medical providers, therapy recommendations, holistic options, and complementary therapies, and rationale for your decisions. Include when you will want to see the patient next. This comprehensive plan should relate directly to your Assessment and include patient education.
|
References
Kandola, A., & Stubbs, B. (2020). Exercise and anxiety. Physical Exercise for Human Health, 345–352. https://doi.org/10.1007/978-981-15-1792-1_23
Klevebrant, L., & Frick, A. (2022). Effects of caffeine on anxiety and panic attacks in patients with panic disorder: A systematic review and meta-analysis. General Hospital Psychiatry, 74, 22–31. https://doi.org/10.1016/j.genhosppsych.2021.11.005
Krzikalla, C., Morina, N., Andor, T., Nohr, L., & Buhlmann, U. (2023). Psychological interventions for generalized anxiety disorder: Effects and predictors in a naturalistic outpatient setting. PLOS ONE, 18(3). https://doi.org/10.1371/journal.pone.0282902
Mishra, A. K., & Varma, A. R. (2023). A comprehensive review of the Generalized Anxiety Disorder. Cureus. https://doi.org/10.7759/cureus.46115
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Patient with Generalized Anxiety Disorder
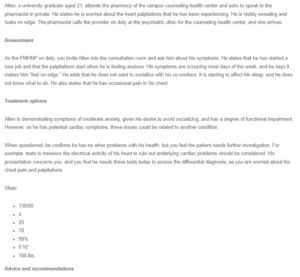
Allen, a university graduate aged 21, attends the pharmacy of the campus counseling health center and asks to speak to the pharmacist in private. He states he is worried about the heart palpitations that he has been experiencing. He is visibly sweating and looks on edge. The pharmacist calls the provider on duty at the psychiatric clinic for the counseling health center, and she arrives.
Assessment
As the PMHNP on duty, you invite Allen into the consultation room and ask him about his symptoms. He states that he has started a new job and that the palpitations start when he is feeling anxious. His symptoms are occurring most days of the week, and he says it makes him “feel on edge.” He adds that he does not want to socialize with his co-workers. It is starting to affect his sleep, and he does not know what to do. He also states that he has occasional pain in his chest.
Treatment options
Allen is demonstrating symptoms of moderate anxiety, given his desire to avoid socializing, and has a degree of functional impairment. However, as he has potential cardiac symptoms, these issues could be related to another condition.
When questioned, he confirms he has no other problems with his health, but you feel the patient needs further investigation. For example, tests to measure the electrical activity of his heart to rule out underlying cardiac problems should be considered. His presentation concerns you, and you feel he needs these tests today to assess the differential diagnosis, as you are worried about his chest pain and palpitations.
Vitals:
- 138/80
- 4
- 20
- 78
- 99%
- 5’10”
- 188 lbs.
Advice and recommendations
You encourage Allen by saying that it is great that he felt he could talk to a pharmacist about this, but explain that he would benefit from continued management with you as the PMHNP and possibly some additional psychotherapy. You explain that his symptoms could be related to anxiety and that you think he may need something to help him manage. He agrees to let you continue the assessment and design a treatment plan.
Use the Initial Psychiatric Assessment SOAP Note template to complete the documentation with the information provided, diagnose the patient, and design a treatment plan.

