Discussion Responses – Conduct Disorder
Response to Peer 1
Hello Danielle,
This is a great post. You captured the biopsychosocial risk and resilience factors well before and during the onset of the conduct disorder. Your brief points make it easier to understand the case study and factors contributing to the development of conduct disorder and what exacerbates it. The diagnosis of conduct disorder was made after considering the client’s history and any concerning behaviors that were noticed. The diagnosis of conduct disorder in children follows the etiology of the condition. However, CD has a complex etiology as it is a result of interacting biological and psychosocial factors regardless of whether they are risk or resilience factors. However, as noted in the case study, diagnosis of the disorder is complicated by the presence of comorbid conditions such as ADHD and PTSD in children with CD (Wu et al., 2023). Some notable behaviors associated with CD, such as how the client stays interactive and polite when not angry but also throws a tantrum and becomes violent, can be confused for mood disorders.
References
Wu, T., Howells, N., Burger, J., Lopez, P., Lundeen, R., & Sikkenga, A. V. (2023). Conduct Disorder. Treating Disruptive Disorders: A Guide to Psychological, Pharmacological, and Combined Therapies, 120–143. https://doi.org/10.4324/9781315867298-9
Response to Peer 2
Hello Whitney,
Thank you for your post. I agree with your diagnosis of conduct disorder and the rationale provided for the diagnosis. Children with CD usually display behaviors that align with common mood and neurodevelopmental and behavioral disorders such as attention deficit hyperactivity disorder (ADHD), posttraumatic stress disorder (PTSD), and other mood disorders such as aggressive and dangerous behaviors, as well as more antisocial behaviors. In this case, the client is also noted to lack empathy. Current evidence shows that elevations in callous-unemotional (CU) traits in some children as they develop lead to a lack of empathy (Frick & Kemp, 2021). This lack of empathy or emotions towards others is linked to the patterns of aggressive behaviors children with CD exhibit. Both the risk factors and the protective influence are closely interrelated, and both, in a way, contribute to the development of CD or support the management of CD as well as other neurodevelopmental and mood disorders in children. In this case, a complete psychiatric evaluation is necessary before concluding the diagnosis.
References
Frick, P. J., & Kemp, E. C. (2021). Conduct Disorders and Empathy Development. Annual Review of Clinical Psychology, 17, 391–416. https://doi.org/10.1146/ANNUREV-CLINPSY-081219-105809
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Discussion Responses – Conduct Disorder
Your client this week is Sam from page 153. Use the course diagnosis template to complete a diagnostic assessment of Sam. When providing feedback to classmates, ensure you can identify commonalities in the assessment you share, as well as offer constructive criticism.
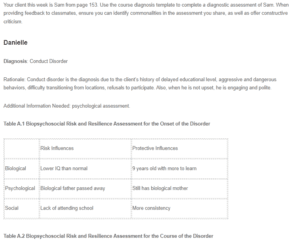
Danielle
Diagnosis: Conduct Disorder
Rationale: Conduct disorder is the diagnosis due to the client’s history of delayed educational level, aggressive and dangerous behaviors, difficulty transitioning from locations, refusals to participate. Also, when he is not upset, he is engaging and polite.
Additional Information Needed: psychological assessment.
Table A.1 Biopsychosocial Risk and Resilience Assessment for the Onset of the Disorder
| Risk Influences | Protective Influences | |
| Biological | Lower IQ than normal | 9 years old with more to learn |
| Psychological | Biological father passed away | Still has biological mother |
| Social | Lack of attending school | More consistency |
Table A.2 Biopsychosocial Risk and Resilience Assessment for the Course of the Disorder
| Risk Influences | Protective Influences | |
| Biological | Male 9 years old | Hormone levels may be changing |
| Psychological | Mother not around much | Lives with great grandmother |
| Social | Stays interactive and polite when not angry | Able to learn more |
Goals:
- Have the child attend anger management and counseling.
- Try to attend school at least 3 days a week with no disruptions.
- Promote Basketball to use as a distraction for his anger.
Critical Perspective of the Diagnosis:
The client is a 9-year-old male with signs of conduct disorder. He has a history of extreme anger to everyone around him. He recently lost his father by gunshot and his uncle. His mother is inconsistent with care. However, he lives with his great grandmother that seems to feed and clothe him decently. Client states he is not generally sad but is angry all the time. He can be polite and engaging when calm. The goals for the client would be to attend anger management and counseling services. He should try to attend school starting out 3 times a week with no disruptions and work up from there. Promoting basketball to use as a distraction for his anger would be beneficial for the client as well.
Whitney
Case Study: Sam
Diagnosis: Conduct Disorder (CD)
Rationale: Exhibits aggressive and dangerous behaviors; threatens to bring a weapon to school to kill staff; spits at, lunges at, bites, and attacks staff, becomes verbally disrespectful towards teacher; destroys property (ripping papers, breaking pencils, turning over chairs and desks)
Additional Information Needed: Specifics of behavior that warranted a complaint with the court and outcome; complete psychiatric evaluation; clearer information on Sam’s mother’s mental health status and why she receives SSI; interview with Sam’s mother and Sam separately to gain more perspective
Table A.1 Biopsychosocial Risk and Resilience Assessment for the Onset of the Disorder
| Risk Influences | Protective Influences | |
| Biological | Male, possible lack of discipline, low SES, low IQ, low emotional intelligence | Has a relationship with paternal great-grandmother |
| Psychological | Lack of guilt or empathy, low verbal IQ, high rates of family problems | Access to home-based services |
| Social | Poverty, unemployment, racial prejudice, mother’s possible depression, mother’s rejection and lack of involvement, | Access to alternative school, no reported abuse |
Table A.2 Biopsychosocial Risk and Resilience Assessment for the Course of the Disorder
| Risk Influences | Protective Influences | |
| Biological | Significantly delayed reading, writing, and math skills | In good health with a good appetite |
| Psychological | Father shot to death, mother tried to relinquish parental rights, mothers’ disengagement in child’s interventions | Does not report being generally sad, reports no abuse |
| Social | Poor parent-child relationship, 3 moves and 4 schools in 3 years, recent death of grandmother | When not upset, polite and engaging, shows interest in sports |
Goals:
- Complete psychiatric evaluation.
- Explore treatment options for Sam such as social skills training, feeling management, stress management, learning alternatives to aggressions and how to plan ahead, anger control, and moral education, as well as family interventions such as parent training.
- Develop expectations with school staff, family, and Sam to develop a sense of consistency and known benchmarks for success.
Critical Perspective of the Diagnosis: While Sam presents with many behavioral symptoms, he also has experienced many life stressors. It is unclear whether these behavioral symptoms are a dysfunction of Sam or if they would not have presented without the stressors.

