Healthcare Ethics Recommendation
Hospitals and other healthcare settings are sometimes presented with challenging patient health situations that create ethical dilemmas. The situation may create conflicts and uncertainty between any actions that may be taken and ethical principles in healthcare. Ethical principles provide a framework that guides decisions in usual and emergency healthcare settings. However, even considering the ethical principles in making the decisions, decision-makers may still find it hard to reach an ethically conclusive decision. This paper addresses a case study in the Neonatal Intensive Care Unit (NICU) involving a Baby Bundle born with anencephaly. It will explore the roles of major stakeholders in the case, the decision-makers, the baby’s rights, ethical considerations, and the role of healthcare managers in making ethical decisions. It will also provide recommendations to assist the baby’s parents in making decisions related to the child’s care.
Identify the major stakeholders in the case.
Stakeholders are all individuals and other groups that are directly or indirectly involved in the care delivery process or have an interest in the healthcare case and how, to some extent, they influence the case outcomes. In the case of Baby Bundle, the main stakeholders are the baby itself, the parents, the Neonatal Intensive Care Unit (NICU) doctor, the nurses involved in the case, the social care services worker, the nurse practitioner (NP) assigned to the NICU, the pediatric ICU nurse, the pediatric ICU doctor, the family health insurer, and the University Hospital Centers and the Child Specialty Clinics management.
Identify the case’s ultimate decision makers (e.g., medical team, parents, etc.).
Decision-making in medical settings is an organizational process involving many stakeholders. There are various individuals and stakeholders who can make legitimate decisions in healthcare settings. Regardless of the need for autonomy at the level of the patient, the overall clinical judgment will always be guided by professional input from the medical team and other stakeholders. The first approach to making the right is determining the ultimate decision-makers in a case. In Baby Bundle’s case, the ultimate decision-maker determination is based on the expected treatment and care outcomes, how well the decision-makers understand the risks and the processes of achieving those outcomes, and the relationship between the patient and the stakeholders. The decision-makers will also be determined based on whether their input will help achieve the set care goals for Baby Bundle. Therefore, based on these factors, the ultimate decision-makers will be Baby Bundle’s parents, the physicians directly involved in the case, the nursing teams directly caring for Baby Bundle, and the facility’s legal advisor.
Explain Baby Bundle’s rights in this case.
Baby Bundle has all the rights as a child and as a patient in the facility. Every child has a right to have their privacy protected and not be exposed (Jenssen et al., 2021). This means they must be handled in a way that preserves her dignity. Although the newborn baby bundle may not be conscious of their surroundings and self, they have a right to be treated with the utmost respect as both a child and a patient in the facility. Baby Bundle has a right to receive the best available care and be handled in a way that comforts the child and the parents. Additionally, Baby Bundle may not be able to ask any questions about her treatment. In this case, the parents of the baby have the right to be provided with all the necessary information about the state of their child’s health, the situation, the possible care the child can be provided with, the risks involved in care, who will be involved in the care team for their child, and any other question they may have related to the case.
Describe the ethical theories or principles that pertain to the case.
The case of Baby Bundle presents a complex patient situation with numerous ethical dilemmas. For instance, the capacity of the patient to make autonomous decisions with regard to their plan. Making ethical decisions in health care involves using various knowledge resources and considering principles of health care ethics (McCradden et al., 2020). The principles of clinical ethics provide a framework for making ethical decisions in complex clinical practice situations. Health care has four main ethical principles: beneficence, nonmaleficence, autonomy, and justice (Varkey, 2021). In the case of Baby Bundle, the question of the autonomy of children in medical situations is an issue of concern as it cannot be guaranteed. However, communication with parents and other facilitators has improved the patient’s autonomy in complicated care cases (Lin et al., 2020). Other stakeholders have to make decisions on behave of Baby Bundle. The principles of beneficence and justice will be considered to guide decisions and ensure that Baby Bundle receives care that is right for their health situation and will help improve their health outcomes and experiences. The stakeholders in the case will inform the parents of the Baby Bundle’s situation and what treatment and procedures will be possible to help their child to make an informed consent. The ethical principles of autonomy, beneficence, and justice will help guide the decisions and actions the care team and the parents make and take toward the care of Baby Bundle.
Analyze your role as a health care manager in this ethics committee decision.
The case of Baby Bundle presents a number of ethical conflicts, uncertainty about the outcome of any care decisions that will be made, and competing values, decision factors, and perspectives between the care providers and the parents. As the health care manager and a member of the ethics committee, I am responsible for presenting approaches to the committee to address best the conflicts and ethical issues related to the case. In my other roles as a member of the ethics committee and an executive of the facility, I will ensure that the ethical committee’s decisions align with the facility’s established ethical culture that guides the facility’s decision-making processes. My roles will also include providing the committee with the right resources, such as information on the case, the facility’s commitments to ethical care, and other resources that guide the committees towards making ethical decisions that best address the case. Additionally, I will provide the committee with the facility’s perspective on the case, the legal risks related to the case, and the facility’s ability to support ethical care regarding resources and available evidence on managing anencephaly.
Based on your review of the case and the fact that the parents are not in agreement, state your recommendation to the committee for the next steps.
Ethical decision-making requires that all decision-makers agree on the decision made and all conflicts have been addressed. Baby Bundle’s parents are not in agreement with the decisions made and the course of action towards the treatment of Baby Bundle. The following recommendations are developed to address the next steps to ensure the child’s right to care and justice are met:
- A social worker and an expert on anencephaly will be required to talk to the parents with a focus on the possibility of success for the procedures for the management of anencephaly and the consequences the parents risk by denying the child their right to receive care if available,
- Consideration should be made to report the case to child services and follow other legal procedures to allow the professionals to proceed with the procedures.
References
Jenssen, B. P., Kelly, M. K., Powell, M., Bouchelle, Z., Mayne, S. L., & Fiks, A. G. (2021). Covid-19 and changes in child obesity. Pediatrics, 147(5). https://doi.org/10.1542/PEDS.2021-050123/180889
Lin, B., Gutman, T., Hanson, C. S., Ju, A., Manera, K., Butow, P., Cohn, R. J., Dalla-Pozza, L., Greenzang, K. A., Mack, J., Wakefield, C. E., Craig, J. C., & Tong, A. (2020). Communication during childhood cancer: Systematic review of patient perspectives. Cancer, 126(4), 701–716. https://doi.org/10.1002/CNCR.32637
McCradden, M. D., Joshi, S., Mazwi, M., & Anderson, J. A. (2020). Ethical limitations of algorithmic fairness solutions in health care machine learning. The Lancet Digital Health, 2(5), e221–e223. https://doi.org/10.1016/S2589-7500(20)30065-0
Varkey, B. (2021). Principles of Clinical Ethics and Their Application to Practice. Medical Principles and Practice, 30(1), 17–28. https://doi.org/10.1159/000509119
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Write an 875- to 1,225-word response to the ethical committee regarding your recommendation as a health care manager presented with this case. In your response, you should:
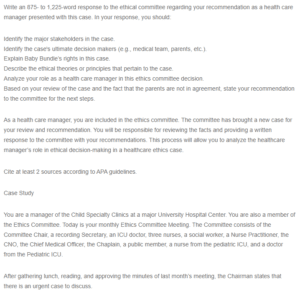
Healthcare Ethics Recommendation
Identify the major stakeholders in the case.
Identify the case’s ultimate decision makers (e.g., medical team, parents, etc.).
Explain Baby Bundle’s rights in this case.
Describe the ethical theories or principles that pertain to the case.
Analyze your role as a health care manager in this ethics committee decision.
Based on your review of the case and the fact that the parents are not in agreement, state your recommendation to the committee for the next steps.
As a health care manager, you are included in the ethics committee. The committee has brought a new case for your review and recommendation. You will be responsible for reviewing the facts and providing a written response to the committee with your recommendations. This process will allow you to analyze the healthcare manager’s role in ethical decision-making in a healthcare ethics case.
Cite at least 2 sources according to APA guidelines.
Case Study
You are a manager of the Child Specialty Clinics at a major University Hospital Center. You are also a member of the Ethics Committee. Today is your monthly Ethics Committee Meeting. The Committee consists of the Committee Chair, a recording Secretary, an ICU doctor, three nurses, a social worker, a Nurse Practitioner, the CNO, the Chief Medical Officer, the Chaplain, a public member, a nurse from the pediatric ICU, and a doctor from the Pediatric ICU.
After gathering lunch, reading, and approving the minutes of last month’s meeting, the Chairman states that there is an urgent case to discuss.
There is a situation in the Neonatal Intensive Care Unit (NICU). A Baby Bundle was born yesterday with anencephaly. Because he had trouble breathing, he was placed on a ventilator and is in the NICU.
For our public member, I will explain: Anencephaly in this child is a congenital neural tube defect where a major portion of his brain, skull, and scalp are missing. The brain stem is the only part of the brain that is present. The brain stem supports the autonomic functions and reflex actions, but he remains permanently unconscious because he lacks his cerebrum. The cerebrum is important because it sets us apart as humans. Not only is the cerebrum the largest part of the brain in humans, but the cerebrum also enables speech, thinking and reasoning, judgment, problem-solving, emotions, and learning. It also serves to initiate and coordinate movements and initiate movement. Anencephaly is always fatal. The children almost always die within a few days, although there have been very few exceptions. The transplant team often approaches parents of children with anencephaly to donate various organs from their child.
Thus, Baby Bundle lacks cognitive abilities or awareness and cannot hear, see, or interact with his environment. Baby Bundle’s brain stem supports his autonomic and reflex actions, but he is permanently unconscious because he lacks a cerebrum. The issue we are looking at today is the father wants to terminate Baby Bundle’s treatment.
The mother wants to continue medical treatment. The doctors have informed the parents of the dismal future for the child and advised termination of treatment. The nurses feel that the child feels pain and is suffering when they suction his ventilator tube and take blood work. Mr. and Mrs. Bundle have been married for 5 years, and this is their first child. Mr. Bundle is an accountant, and Mrs. Bundle works for NASA but has been on maternity leave for 6 months.
QUESTIONS TO CONSIDER
MEDICAL INDICATIONS
What is the patient’s medical problem? History? Diagnosis? Prognosis?
PATIENT PREFERENCE
What has the patient expressed about preferences for treatment (e.g., advanced directives)?
Has the patient been informed of the benefits and risks, understood, and consented?
Is the patient mentally capable and legally competent? What is evidence of incapacity?
If incapacitated, who is the appropriate surrogate? Is the surrogate using appropriate standards?
In sum, is the patient’s right to choose to be respected to every extent possible in ethics and law?
QUALITY OF LIFE
What are the prospects, with or without treatment, for a return to the patient’s normal life?
Are there biases that might prejudice the provider’s evaluation of the patient’s quality of life?
What physical, mental, and social deficits will the patient likely experience if treatment succeeds?
Is the patient’s present or future condition such that continued life might be judged undesirable by them?
Is there any plan and rationale to forgo treatment?
What plans are there for comfort and palliative care?
CONTEXTUAL FEATURES
Are there family issues that might influence treatment decisions?
Are there provider (physicians and nurses) issues that might influence treatment decisions?
Are there financial and economic factors?
Are there religious and cultural factors?
Is there any justification for breaching confidentiality?
Are there any problems with the allocation of resources?
What are the legal implications of treatment decisions?
Is clinical research or teaching involved?
Any provider or institutional conflict of interest?

