Addressing the Potential Second Surge in COVID-19 Cases
Disciplines For The Team And The Number Of Participants
The COVID-19 outbreak created a public health emergency that created the need for partnered response among healthcare professionals and the public (Tabari et al., 2020). As the number of COVID-19 infections starts to rise, it is important, as the hospital’s CEO, I am tasked with setting up a response team to help manage the new COVID-19 cases. The Centers for Disease Control and Prevention (2020) notes that a rapid response team should be made of all essential components of public health emergency response, including coordination of administrative units and elements of a functional healthcare system. Based on these CDC guidelines, the disciplines I will include in the QI team to assist in preparing for a second surge will include; a team leader, 2 case management officers, two epidemiologists, two infection prevention and control specialists, 2 Laboratory specialists, two risk communication officers, four nurses, two nurse informaticists, and two social mobilization specialists. Therefore, a total of 19 individuals will participate in the team.
Mission Statement and Goals for the Team
The mission statement for the team is to work collaboratively towards optimizing care for all patients during this time of COVID-19. The goals for the team include:
- Ensuring readiness for the second COVID-19 outbreak,
- Rapid detection and control of new cases,
- Rapid contact tracing and setting up quarantine centers,
- Optimize patient care for all patients, including COVID-19 patients,
- Reduce the spread of the new outbreak,
- Ensure the facility and the responders are well equipped with the resources, including educational resources,
- Minimize the impact of COVID-19 on the facility’s operations as well as the community.
The Methodology For The Planned Process
The QI team will utilize the Plan-Do-Study-Act (PDSA) Methodology to prepare for the second surge. The PDSA cycle is a proven methodology that has been effectively applied in evaluating and sustaining quality improvement projects within emergency care settings (Chartier et al., 2019).
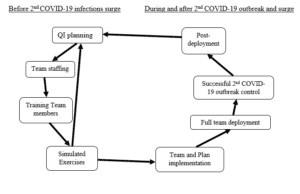
Mapping Out the Plan Utilizing the PDSA Cycle
The PDSA methodology provides a systematic approach to the continuous improvement of quality. The PDSA cycle will guide the preparations and response to the second COVID-19 infection surge. Based on the Plan-Do-Study-Act cycle, below is a map of the plan to address the 2nd potential surge in COVID-19 cases:
Barriers and Challenges
The QI team faced various challenges and barriers during and after the implementation process of the plan. During the development of the QI plan, the team had to deal with communication and role confusion challenges. The team had various misunderstandings regarding the role of each specialist and how information was to be shared with the members, which restricted the plan’s progress at the beginning of the process. However, these challenges were solved through training on communication and role integration, which have been proven to be successful in promoting positive communication and relationships in demanding care settings such as surgical teams (Tørring et al., 2019). The team did not face many challenges and barriers during implementation as a majority of the issues had been identified during the QI planning and systems set in place to solve any emerging challenges.
The Criteria the Team Must Meet for Success
The team will be successful if they can successfully integrate their diverse roles, communicate as a team, and work as one during the QI planning and implementation process. Role integration, role reconfiguration, and effective communication help interdisciplinary teams work together and are integral to team functioning (Schot et al., 2020).
Measuring The Team’s Success
The success of the team will be measured based on various indicators, including the time taken to fully deploy the emergency response team, the percentage of the suspected and lab-confirmed COVID-19 cases identified within the facility, and the effectiveness of contact tracing within 48 hours of reporting. Success will also be measured based on the percentage of quarantined contacts after tracing, the percentage of newly reported hospital-acquired infections (HAI), and the self-reported levels of team member satisfaction.
Disband the Team or Not?
According to the Centers for Disease Control and Prevention (2020), the response to the COVID-19 outbreak in countries that had existing rapid response teams and those that lacked such teams and the overall use of such teams in managing the outbreak showed the importance of having ready multidisciplinary teams in public health management. Therefore, the team will remain intact after fully implementing the intervention. The team will not be disbanded but will remain operational, with normal hospital roles but readily available as an effective rapid response team to health emergencies.
References
Centers for Disease Control and Prevention. (2020). Guidance For U.S. Centers For Disease Control And Prevention Staff For The Establishment And Management Of Public Health Rapid Response Teams For Disease Outbreaks. In CDC. https://www.cdc.gov/globalhealth/healthprotection/errb/pdf/RRTManagementGuidance-508.pdf
Chartier, L. B., Vaillancourt, S., Cheng, A. H. Y., & Stang, A. S. (2019). Quality improvement primer part 3: Evaluating and sustaining a quality improvement project in the emergency department. Canadian Journal of Emergency Medicine, 21(2), 261–268. https://doi.org/10.1017/CEM.2018.380
Schot, E., Tummers, L., & Noordegraaf, M. (2020). Working on working together. A systematic review of how healthcare professionals contribute to interprofessional collaboration. Journal of Interprofessional Care, 34(3), 332–342. https://doi.org/10.1080/13561820.2019.1636007/SUPPL_FILE/IJIC_A_1636007_SM9051.DOCX
Tabari, P., Amini, M., Moghadami, M., & Moosavi, M. (2020). International Public Health Responses to COVID-19 Outbreak: A Rapid Review. Iranian Journal of Medical Sciences, 45(3), 157. https://doi.org/10.30476/IJMS.2020.85810.1537
Tørring, B., Gittell, J. H., Laursen, M., Rasmussen, B. S., & Sørensen, E. E. (2019). Communication and relationship dynamics in surgical teams in the operating room: An ethnographic study. BMC Health Services Research, 19(1), 1–16. https://doi.org/10.1186/S12913-019-4362-0/TABLES/4
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Addressing the Potential Second Surge in COVID-19 Cases
Scenario
It is the beginning of the fall season and the number of COVID-19 cases and infection rate is starting to increase above the rolling average experienced the past month. The CEO of your hospital has assigned you the responsibility of convening a QI team to assist in preparing for a second surge.
What disciplines would you select for the team and how many individuals should participate?
Develop a mission statement and goals for the team.
What methodology will they utilize for their planned process? hint PDSA is one type.
Map out the plan to address the potential 2nd surge in COVID-19 cases utilizing the methodology selected, for example–Plan, Do, Study, Act.
a. What barriers or challenges did the QI team face along the way, as well as during the implementation process?
b. What criteria do you believe the team needs to meet to be successful?
c. How would you measure the team’s success?
d. Once the team has implemented their interventions, would you disband them?