Advocating for Lasting Change
Hello, and welcome to the presentation on advocating for lasting change. The exhibition aims to identify healthcare challenges and opportunities, provide budget estimates, evaluate leaders ‘ leaders positive and negative influences on healthcare processes, and develop proactive strategies to change the organization’s culture by incorporating evidence-based practices.
The main stakeholders include:
- The Chief executive officer
- The Head of health services
- The Insurance executives.
- The Head of departments
- The State and Federal government representatives.
They are involved in policy-making for the healthcare system.
Numerous challenges face the healthcare system. The rural city has only two health centers, St. Francis Health Center and Oak Terrace Senior Living Centre, located in Midtown and suburban Districts. There is no healthcare organization in the downtown district. Further, these health centers are inaccessible from the downtown district (Vila Health, n.d.). Caregivers in rural settings face fewer formal services, fewer health care providers and health education services, difficulties with transportation, weather problems in winter, and isolation. Residents from the downtown district would face increasing health issues, as they do not have access to the health care system of access to midtown health centers. There is limited education and awareness due to inadequate healthcare providers, and easy access to fast food and alcohol only adds to the healthcare complications. As the population ages, there are more robust mortality indicators and chronic diseases such as cancer and cardiovascular diseases. Low awareness of healthy lifestyles and eating habits, lack of transportation, internet, and healthcare services prevent the community from enjoying quality healthcare services. Health literacy is a crucial predictor of health status. As the residents living in the rural community reflect the lower socioeconomic status and education level, it can impact their attitude towards health and their health outcomes.
The goals and potential outcomes of the proposed change are to improve patient health outcomes with more accessible and convenient access to health care and lower healthcare costs. The direct benefits of using Telemedicine are direct interaction between the physicians and the patients, even from remote areas. Telemedicine applications are linked to handling large volumes of complex data and electronic patient records with the help of mobile devices and technology (Flodgren et al., 2015). The changes and improvements will positively impact the overall health of the rural community with limited access to health care. Telemedicine can encourage real‐time remote monitoring with video‐conferencing depending on clinical condition and provide prompt treatment and advice for self‐management. Nurses can offer education and support to the patients while the specialists can provide treatment decisions and consultations for diagnosis remotely (Flodgren et al., 2015). The potential barriers to Telehealth in rural areas include limited access to high-speed internet and broadband availability, limited access to a smartphone and licensing for state requirements, and lack of awareness among the rural populations (RHI Hu, 2021).
Certain environmental and social factors in the rural community can create resistance to changes, such as an aging population, limited education, and low awareness regarding Telehealth, which creates mistrust of technology and healthcare. Acceptability can be influenced by the expectations and discrimination in healthcare systems by the local racial/ethnic minority populations (Zahnd et al., 2021). Policy and financial support are necessary to overcome these barriers and fully implement telemedicine. Implementing telemedicine will help overcome present challenges, such as limited access to healthcare due to inadequate healthcare facilities.
Telemedicine will help to produce the intended outcomes by facilitating various tasks. They include
Follow-up visits
Using telemedicine-associated technology for routine patient follow-up is more efficient for providers and patients and increases the likelihood of follow-up, reducing missed appointments and improving patient outcomes. This will help to increase access to healthcare services and ensure timely delivery of services.
Remote chronic disease management
The increasing rate of chronic diseases in the rural community is a significant challenge to the health system. Telemedicine software will be beneficial because it makes it easier and less expensive for patients to maintain control over their health. Furthermore, it helps to solve the problem of inadequate healthcare providers because they can monitor numerous patients remotely. An example is Remote patient monitoring for diabetic and hypertensive patients, where they can measure their blood sugars or blood pressure remotely and transmit the values to healthcare providers (Flodgren et al., 2015).
Preventative care support
Weight loss and smoking cessation are critical to reducing heart disease and other conditions. Telemedicine can be a valuable tool in connecting providers with patients to ensure they get the support they need to succeed. This can be achieved by RPM, videoconferencing, and mobile applications (Flodgren et al., 2015).
Assisted living center support
Telemedicine software has already proven helpful in keeping assisted living facility residents out of the hospital. Problems often occur at night or on weekends, making hospitalization the only option, even for less urgent issues. With telemedicine, on-call doctors can conduct a remote visit to determine if hospitalization is necessary(Flodgren et al., 2015).
Ongoing patient education
Telemedicine technologies such as videoconferencing enable healthcare providers to provide promotive and preventive education to patients. This helps to avoid lifestyle diseases.
Different resources should be considered when estimating the budget for the proposed change. The first resource is access to broadband internet. A solid and sufficient bandwidth is required to transmit audio and video data. Rural healthcare organizations and community patients can experience difficulties connecting to or obtaining affordable and reliable broadband service (Chen, 2017).
The second resource is Imaging technology or peripherals. These devices are the backbone of telemedicine. They allow rural health organizations to monitor patients even when miles apart. Digital stethoscopes, for instance, can transmit heart and lung sounds to remote providers (Chen, 2017).
The third resource is the technical support staff. Technical support staff members can help answer questions about telehealth programs. To help with efficiency, technical support staff may be shared across collaborating organizations.
The fourth resource is the training of staff. Staff should be trained on how to use telehealth technology, which may take time. Considerations on the workflow changes should be made and training done accordingly (Chen, 2017).
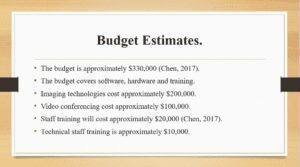
The budget estimate for the proposed change is approximately $330,000. The cost of imaging technologies for essential primary care services ranges from $4,000-$9,000, including devices such as an examination camera, ENT scope, and digital stethoscope (Chen, 207). The total budget for imaging technologies is approximately $200,000. Depending on the video conferencing needs, a Web-based telemedicine portal having software-based or hardware-based video conferencing can be used(Chen, 2017). The software-based route can cost as little as $1,000 per patient site without cost for the remote provider. The price for hardware-based video conferencing can start around $9,000 per patient site and increases with the number of remote provider sites you need. It is estimated that the total cost for videoconferencing for 100 patients using the software-based option is $100,000. Staff training programs for telemedicine range from $150 to $1,500 per site, depending on the complexity of equipment, the number of users, and other factors. The total cost for staff training and support staff training is approximately $20,000 and $10,000 respectively.
The five management practices will lead to transformational, evidence-based change in the organization. According to the behavioral and organizational research model, management practices that are consistently associated with the successful implementation of change initiatives include balancing the tension between efficiency and reliability (safety), creating and sustaining trust throughout the organization, actively managing the process of change, involving workers in decision making about work design and workflow, and using knowledge management practices to establish the organization as a learning organization. A balance between efficiency and reliability will ensure that telemedicine produces the desirable evidence-based results. Establishing trust between healthcare providers and patients will ensure that patients embrace telemedicine actively and facilitate its implementation. Both internal and external stakeholders should be involved in the decision-making process. This will lead to the identification of gaps in the proposed change. This will ensure that an evidence-based approach is chosen. Therefore, essential management practices will help establish a transformational, evidence-based change in the organization.
The proposed change initiative is to make the rural population aware of new technologies in health care and offer them the required education and information to realize the benefits of telemedicine before implementing it. Implementation of this project will have long-term benefits in the future. Currently, members of the remote rural community face challenges such as Inadequate healthcare facilities, inadequate healthcare providers, deficiency of health education, an increase in acute and chronic diseases, and poor housing predisposing members to conditions. Implementation of the project will result in better and improved overall care by Increasing access to healthcare services, ensuring timely delivery of healthcare services, and reducing morbidity and mortality rates from chronic diseases due to timely delivery of healthcare services.
A transformational leadership style is selected because of its desirable traits. The first trait is inspirational motivation. It refers to the degree to which a leader articulates an appealing vision that inspires and motivates others to perform beyond expectations. Leaders with an emotional basis have high standards and expectations for their followers. They are optimistic about followers’ ability to meet goals and always provide meaning to their followers by showing the importance of all duties and responsibilities (Generett & Welch, 2018). This will enable the successful implementation of the change proposal. Idealized influence requires the leader to engage in ethical behavior. Ethical behavior creates respect among followers. This allows followers (staff and patients) to work towards the vision. Intellectual stimulation is a trait that focuses on the extent to which transformational leaders challenge assumptions, take risks, and solicit followers’ ideas. They recognize followers through stimulation, creativity, and innovation. The leader supports and collaborates with the followers as they try new approaches (Generett & Welch, 2018). This is important because it encourages feedback delivery on the success of the change.
Stakeholders must support the project because it addresses the remote rural population’s problems. Caregivers in rural settings face fewer formal services, fewer health care providers and health education services, difficulties with transportation, weather problems in winter, and isolation. This hinders the provision of health education to patients. Furthermore, the facilities are inadequate. The city has only two health centers, St.Francis Health Center and Oak Terrace Senior Living Centre, located in Midtown and suburban Districts. There is no healthcare organization in the downtown district. Further, these health centers are inaccessible from the downtown district (Vila Health, n.d.). The proposed change faces challenges such as limited internet, software, and hardware access.
There is limited access to smartphones, licensing for state requirements, and a lack of awareness among rural populations (RHI Hu, 2021). The importance of the project necessitates funding to avert the challenges facing its successful implementation. Therefore, stakeholders should be actively involved in supporting the change.
Stakeholders’ support is needed to raise the resources required for the proposed change. The budget estimate for the proposed change is approximately $330,000. The cost of imaging technologies for essential primary care services ranges from $4,000-$9,000, including devices such as an examination camera, ENT scope, and digital stethoscope(Chen, 2017). The total budget for imaging technologies is approximately $200,000. Depending on the video conferencing needs, a Web-based telemedicine portal having software-based or hardware-based video conferencing can be used. The software-based route can cost as little as $1,000 per patient site without cost for the remote provider. The price for hardware-based video conferencing can start around $9,000 per patient site and increases with the number of remote provider sites you need. It is estimated that the total cost of videoconferencing for 100 patients using the software-based option is $100,000 (Chen, 2017). Staff training programs for telemedicine range from $150 to $1,500 per site, depending on the complexity of equipment, the number of users, and other factors. The total cost for staff training and support staff training is approximately $20,000 and $10,000 respectively. Therefore, the importance of the change to the remote rural community necessitates support from stakeholders to ensure that it is fully implemented.
The goals and potential outcomes of the proposed change are to improve patient health outcomes with more accessible and convenient access to health care and lower healthcare costs. The direct benefits of using Telemedicine are direct interaction between the physicians and the patients, even from remote areas. Telemedicine applications are linked to handling large volumes of complex data and electronic patient records with the help of mobile devices and technology (Flodgren, Rachas, Farmer, Inzitari, Shepperd, & Shepperd, (2015). The changes and improvements will positively impact the overall health of the rural community with limited access to health care. Telemedicine can encourage real‐time remote monitoring with video‐conferencing depending on clinical condition and provide prompt treatment and advice for self‐management. Nurses can offer education and support to the patients while the specialists can provide treatment decisions and consultations for diagnosis remotely (Flodgren, Rachas, Farmer, Inzitari, Shepperd, & Shepperd, (2015). The potential barriers to Telehealth in rural areas include limited access to high-speed internet and broadband availability, limited access to a smartphone and licensing for state requirements, and lack of awareness among the rural populations (RHI Hu, 2021).
Certain environmental and social factors in the rural community can create resistance to changes, such as an aging population, limited education, and low awareness regarding Telehealth, which creates mistrust of technology and healthcare. Acceptability can be influenced by the expectations and discrimination in healthcare systems by the local racial/ethnic minority populations (Zahnd et al., 2021). Policy and financial support are necessary to overcome these barriers and fully implement telemedicine. Implementing telemedicine will help overcome present challenges, such as limited access to healthcare due to inadequate healthcare facilities.
The budget estimate for the proposed change is approximately $330,000. The cost of imaging technologies for essential primary care services ranges from $4,000-$9,000, including devices such as an examination camera, ENT scope, and digital stethoscope. The total budget for imaging technologies is approximately $200,000. Depending on the video conferencing needs, a Web-based telemedicine portal having software-based or hardware-based video conferencing can be used. The software-based route can cost as little as $1,000 per patient site without cost for the remote provider. The price for hardware-based video conferencing can start around $9,000 per patient site and increases with the number of remote provider sites you need. It is estimated that the total cost for videoconferencing for 100 patients using the software-based option is $100,000. Staff training programs for telemedicine range from $150 to $1,500 per site, depending on the complexity of equipment, the number of users, and other factors. The total cost for staff training and support staff training is approximately $20,000 and $10,000 respectively. A transformational leader will help fulfill the vision.
Traits of a transformational leader: Individualized consideration, inspirational motivation, idealized influence, and intellectual stimulation. Stakeholder support will help raise the budget and implement the change effectively.
References
Chen, E. T. (2017). Considerations of Telemedicine in the Delivery of Modern Healthcare. American Journal of Management, 17(3), 20–28. http://search.proquest.com.ezproxylocal.library.nova.edu/docview/1963800986?accountid=6579%0Ahttp://novacat.nova.edu:4550/resserv?genre=article&issn=21657998&title=American+Journal+of+Management&volume=17&issue=3&date=2017-09-01&atitle=Considerations+of+T
Flodgren, G., Rachas, A., Farmer, A. J., Inzitari, M., Shepperd, S., & Shepperd, S. (2015). Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Library, 2016(12), CD002098-CD002098.
Generett, G. G., & Welch, O. M. (2018). Transformative Leadership: Lessons Learned Through Intergenerational Dialogue. Urban Education, 53(9), 1102–1125. https://doi.org/10.1177/0042085917706598
Levy, F. (2014). Keeping Patients Safe: Transforming the Work Environment of Nurses. In Critical Care Medicine (Vol. 32, Issue 10). https://doi.org/10.1097/01.ccm.0000142897.22352.05
RHI Hub (2021b). Telehealth Use in Rural Healthcare – Funding & Opportunities. Rural health info, retrieved from https://www.ruralhealthinfo.org/topics/telehealth/funding
Vila Health. (n.d.). Environmental Analysis and Windshield Survey. http://media.capella.edu/CourseMedia/MSN6218/vilaHealthEnvironmentalAnalysisWindshieldSurvey/wrapper.asp
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Develop and record a 10-15-slide, asynchronous, audiovisual presentation for policymakers, soliciting resource and policy support for the community health care system change you proposed in the previous assessment.
Note: This assessment builds upon the work you completed in the previous evaluation. Therefore, conduct the reviews in the order in which they are presented.

Advocating for Lasting Change
Nurse leaders must be able to make effective financial and policy decisions. Equally important is the ability to communicate their vision for change to policymakers and provide objective, evidence-based support for their position concerning systemic change’s regulatory, political, social, ethical, legal, and financial aspects.
This assessment provides an opportunity to develop a presentation soliciting resources and policy support for the community health care change you proposed in Assessment 3. By completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
Competency 1: Identify the challenges and opportunities facing health care.
• Explain why proposed changes to a health care system require policy and financial support to ensure positive, systemic change and to overcome present challenges.
Competency 2: Compare the effects of different healthcare finance models and policy frameworks on resources and patient outcomes.
• Provide broad budget estimates to fund specific capital or human resource outlays that are important to the success of a proposed change.
Competency 3: Evaluate leaders’ positive and negative influences on healthcare processes and outcomes.
- Assess the potential future for wellness, health, and improved overall care and the role of visionary leaders in achieving the desired goals.
- Cultivate stakeholder interest in and support for the proposed community health care system changes.
Competency 4: Develop proactive strategies to change the organization’s culture by incorporating evidence-based practices.
- Provide compelling evidence that proposed changes to a health care system will produce the intended outcomes.
- Outline a plan for leading transformational, evidence-based change in an organization.
Competency 5: Communicate effectively with diverse audiences in an appropriate form and style consistent with applicable organizational, professional, and scholarly standards.
- Develop slides that augment a multimedia presentation.
- Argue persuasively to obtain policy and financial support from policymakers for a proposed community health care change.
Support assertions, arguments, propositions, and conclusions with relevant and credible evidence.