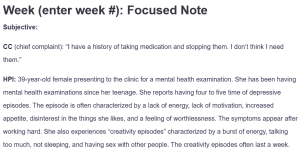
Week (enter week #): Focused Note
Subjective:
CC (chief complaint): “I have a history of taking medication and stopping them. I don’t think I need them.”
HPI: 39-year-old female presenting to the clinic for a mental health examination. She has been having mental health examinations since her teenage. She reports having four to five time of depressive episodes. The episode is often characterized by a lack of energy, lack of motivation, increased appetite, disinterest in the things she likes, and a feeling of worthlessness. The symptoms appear after working hard. She also experiences “creativity episodes” characterized by a burst of energy, talking too much, not sleeping, and having sex with other people. The creativity episodes often last a week.
Psych Hx: The client has a history of depression, anxiety, and bipolar.
Medications trials: Zoloft made her feel “high”. She was also unable to sleep as her heart was racing. Risperidone made her gain weight. Clonipine “slowed her down.”
Substance Current Use: She smokes a pack of nicotine a day. Her last use of alcohol was when she was 19. She has used marijuana once. She denies using any other psychotropic agents.
Family History of Substance Use: The mother had bipolar, her father was imprisoned for drugs, and her brother has schizophrenia.
Medical History: The patient has hyperthyroidism and is on medications. She also has polycystic ovarian syndrome, which forces her to take birth control pills. She has been hospitalized four times for psychiatric illness. One of the hospitalizations was attributed to a suicidal attempt, as the client overdosed on Benadryl in 2017. She has not had any episodes of suicidal thoughts or attempts since.
- Current Medications: None
- Allergies:No known drug allergies
- Reproductive Hx:The client has regular menstruation. Her last menstrual period was last month.
- Legal Hx: Negative
Psychosocial Hx: The client was raised by the mother and older brother. She has a male boyfriend. She reports living with his boyfriend but sometimes lives with her mother, especially when her boyfriend is mad at her for “sleeping around”. The sleeping around seems to be affecting her relationship. The client denies having any children. She works part-time at her aunt’s bookstore. Her aunt fills in for her whenever she does not report because of feeling depressed. The client is currently studying cosmetology. Her hobbies are writing and painting. She was arrested and taken to the hospital for “dancing around”.
ROS:
- GENERAL: Denies fever or chills.
- HEENT: Denies hearing or visual loss, nasal discharge, or difficulty swallowing.
- CARDIOVASCULAR: Denies palpitation or chest pains.
- RESPIRATORY: Denies wheezing or shortness of breath.
- GASTROINTESTINAL: Has excessive appetite on depressed days.
- NEUROLOGICAL: Denies seizures or headaches.
- MUSCULOSKELETAL: Denies muscle or skeletal pain.
- ENDOCRINOLOGIC: The patient has hyperthyroidism.
Objective:
Vitals: Temp 98.2 | Pulse 90 | Respiration 18 | B/P 138/88
The patient seems alert. She had episodes of restlessness and irritability during the interview, as she was irritated by some interview questions.
Diagnostic results: Urine drug and alcohol screens are negative. CBC and CMP are within normal ranges. The lipid panel is also within normal ranges. Prolactin Level 8; TSH 6.3 (H)
Assessment:
Mental Status Examination: The patient is alert and oriented to place and event. She is responsive and answers the interview questions appropriately. Her memory and reasoning are intact. Her judgment is goal-directed and logical. The patient has a history of auditory hallucinations. She had attempted suicide at 17.
Differential Diagnoses:
- Bipolar disorder: A mood disorder characterized by alternating depressive and manic or hypomanic manifestations. During the depressed phase, the person experiences a loss of interest in things and feelings of being overwhelmed, among other depressive episodes. In the manic or hypomanic phase, the patient feels a burst of energy and may have grandiose ideas. They may also be irritable, distractible, and involved in sexual behaviors (Baldessarini et al., 2020). The patient’s manifestation met the criteria for bipolar.
- Major depressive disorder (MDD): The presence of depressive manifestations warranted the inclusion of this differential. As per DSM-V, MDD is characterized by persistent low mood and anhedonia lasting for more than six months (Christensen et al., 2020). It was, however, ruled out due to the presence of the manic manifestations.
- Schizophrenia: The presence of a history of hallucination, delusionary thought patterns, family history of schizophrenia, and a past psychiatric history significant of suicidality, depression, mania, and problems adhering to treatment warranted the inclusion of this differential. Schizophrenia is characterized by hallucinations and delusions. Suicidality may also be apparent in the disorder (Lopez-Castroman et al., 2019).
Diagnostic Impression: Bipolar disorder
- Assessment findings, along with the patient’s manifestations, did not meet the criteria for schizophrenia and MDD.
Reflections:
The interview provided insight into a comprehensive mental health assessment. I would be more interested in a physical examination to corroborate the subjective findings. An ethical consideration in this case is beneficence. Caregivers managing patients must be willing to act in the best interest of the patients. A social determinant of health that interplay in this case is access to health. The patient is at risk of self-harm due to a history of suicidality and should thus be accorded the best care. As a point of health promotion, the patient should be advised to adhere to therapy to stabilize her mood.
Case Formulation and Treatment Plan:
The patient will be started on mood stabilizers and a CBT program. She will be given sodium valproate at a starting dose of 200 mg, administered orally every 12 hours. CBT and pharmacotherapy combination are superior in alleviating bipolar symptoms (Goes, 2023).
References
Baldessarini, R. J., Vázquez, G. H., & Tondo, L. (2020). Bipolar depression: A major unsolved challenge. International Journal of Bipolar Disorders, 8(1). https://doi.org/10.1186/s40345-019-0160-1
Christensen, M. C., Wong, C. M., & Baune, B. T. (2020). Symptoms of major depressive disorder and their impact on psychosocial functioning in the different phases of the disease: Do the perspectives of patients and healthcare providers differ? Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00280
Goes, F. S. (2023). Diagnosis and management of Bipolar Disorders. BMJ. https://doi.org/10.1136/bmj-2022-073591
Lopez-Castroman, J., Leiva-Murillo, J. M., Cegla-Schvartzman, F., Blasco-Fontecilla, H., Garcia-Nieto, R., Artes-Rodriguez, A., Morant-Ginestar, C., Courtet, P., Blanco, C., Aroca, F., & Baca-García, E. (2019). Onset of schizophrenia diagnoses in a large clinical cohort. Scientific Reports, 9(1). https://doi.org/10.1038/s41598-019-46109-8
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
- Review this week’s Learning Resources. Consider the insights they provide about assessing, diagnosing, and treating mood disorders.
- Review the Focused SOAP Note template, which you will use to complete this Assignment. There is also a Focused SOAP Note Exemplar provided as a guide for Assignment expectations.
- Review the video, Case Study: Petunia Park. You will use this case as the basis of this Assignment. In this video, a Walden faculty member is assessing a mock patient. The patient will be represented onscreen as an avatar.
- Consider what history would be necessary to collect from this patient.
- Consider what interview questions you would need to ask this patient.
- Consider patient diagnostics missing from the video:
Provider Review outside of interview:
Temp 98.2 Pulse 90 Respiration 18 B/P 138/88
Laboratory Data Available: Urine drug and alcohol screen negative. CBC within normal ranges, CMP within normal ranges. Lipid panel within normal ranges. Prolactin Level 8; TSH 6.3 (H)
Develop a Focused SOAP Note, including your differential diagnosis and critical-thinking process to formulate a primary diagnosis. Incorporate the following into your responses in the template:
Week (enter week #): Focused Note
- Subjective: What details did the patient provide regarding their chief complaint and symptomatology to derive your differential diagnosis? What is the duration and severity of their symptoms? How are their symptoms impacting their functioning in life?
- Objective: What observations did you make during the psychiatric assessment?
- Assessment: Discuss the patient’s mental status examination results. What were your differential diagnoses? Provide a minimum of three possible diagnoses with supporting evidence, listed in order from highest to lowest priority. Compare the DSM-5-TR diagnostic criteria for each differential diagnosis and explain what DSM-5 criteria rules out the differential diagnosis to find an accurate diagnosis. Explain the critical-thinking process that led you to the primary diagnosis you selected. Include pertinent positives and pertinent negatives for the specific patient case.
- Plan: What is your plan for psychotherapy? What is your plan for treatment and management, including alternative therapies? Include pharmacologic and nonpharmacologic treatments, alternative therapies, and follow-up parameters as well as a rationale for this treatment and management plan. Also incorporate one health promotion activity and one patient education strategy.
- Reflection notes: Reflect on this case. Discuss what you learned and what you might do differently. Also include in your reflection a discussion related to legal/ethical considerations (demonstrate critical thinking beyond confidentiality and consent for treatment!), social determinates of health, health promotion, and disease prevention that takes into consideration patient factors (such as age, ethnic group, etc.), PMH, and other risk factors (e.g., socioeconomic, cultural background, etc.).
Link for case study
- Walden University. (2021). Case study: Petunia Park. Walden University Blackboard. https://waldenu.instructure.com