Value-Based Purchasing
The US healthcare system has, for a long time, relied on fee-for-service compensation. This system operated in such a way that reimbursements were provided for each service provided and did not rely on patient outcomes or costs. There has been a paradigm shift such that healthcare providers are paid for providing quality or value. The US healthcare system is moving toward rewarding value. Value can be increased by reducing costs and improving outcomes, or both.
Healthcare consumes almost 20% of the US economy’s budget (Chee et al., 2016). Because of this, the burden of healthcare expenditures shifts funds away from other essential areas, such as infrastructure and education. The US ranks lower on healthcare indicators even though it ranks highest on healthcare spending. The US healthcare has, therefore, geared toward quality and value. This has been done by incorporating health care outcomes and the resources allocated to achieve those outcomes. Recent legislation such as Medicare Access and the Affordable Care Act have solidified the role played by value-based payment in Medicare. These are important changes in the healthcare system that have a greater impact on care coordination and delivery (Chee et al., 2016).
Value-Based Purchasing (VBP) is a payment model that offers bonuses and financial incentives to healthcare providers to align with the quality standards set by the healthcare organization and meet certain performance measures (Tanenbaum, 2016). Payment adjustments are made based on value metrics. A portion of the work done by providers and hospitals is paid qualitatively based on their patients’ outcomes instead of purely quantitatively based on the number of patients treated. Some of the VBP programs include the MACRA (Medicare Access and CHIP Reauthorization Act) program, State Medicaid, and private insurance value-based purchasing programs (Chee et al., 2016).
As of 2006, a survey done by the Commonwealth Fund to determine the prevalence of VBP programs found that more than 50% of all state Medicaid programs had at least 1 VBP program in place. More than 70% of state Medicaid programs had plans for new programs (Chee et al., 2016). Managed care organizations were the most common VBP programs. The majority of these organizations provided rewards for achieving an attainment threshold. Most of these programs targeted Medicaid beneficiaries, which mainly include children, adolescents, and women.
The shift toward VBPs has accelerated. In 2015 the US Department of Health announced that they intended to tie traditional Medicare payments to value. The plan was to cover 85% by 2016 and 90% of payments by 2018. In 2016, the Hospital VBP Program increased to representing 1.75% of all Medicare payments to hospitals (Chee et al., 2016).
Four domains are mainly targeted when trying to improve hospital performance. These include efficiency, patient outcomes, patient experiences, and clinical processes. The Medicare Hospital VBP Program was implemented as part of the Affordable Care Act. It aims to improve performance in these domains. Hospital administrators are encouraged to improve performance by using Medicare provider payment penalties and bonuses (Lee et al., 2019).
The Impact of VBPs on the Provision of Healthcare and Cost of Care
Value-based purchasing (VBP) is still an essential component of value payment in Medicare Access. VBP programs focus on improving the effectiveness and outcomes of services through primary and ambulatory care instead of relying on hospitals (Pernisi et al., 2017)
Significant changes have been brought to healthcare delivery in the US through the implementation of value-based purchasing. Multiple VBP programs, both inpatient and outpatient, have been implemented widely. The impact of these programs has been marginal. The effectiveness of VBP programs stems from the specifics of program design, incentive structure, as well as the process of implementation (Chee et., 2016). It is challenging to determine the effectiveness of VBP programs because of the complications caused by external factors and also by how one might define success.
The US Department of Health commissioned Damberg et al. in 2014 to evaluate available literature on VBP models. These models include bundled payments, ACOs, and pay-for-performance. One thousand eight hundred ninety-one articles on pay-for-performance programs were screened and reviewed for the study (Chee et., 2016). Numerous positive results showed that incentives improve prevention measures, screening, and treatment.
Nursing case management has traditionally been used to coordinate hospital health care services (Pernisi et al., 2017). Some of the functions include monitoring patients, discharge planning, and coordination of services to manage diseases. VBP programs such as the MACRA program have generated an interest in the use of nursing case management, which is used to adjust the utilization of services. These services include emergency department visits and hospital admissions. Nursing case management is performed in almost every healthcare setting to provide value to the healthcare systems and patients. (Pernisi et al., 2017). Because of the complexity of cases, using registered nurses for the coordination of care has increased under the Affordable Care Act. This includes an insistence on evidence-based practice (Pernisi et al., 2017).
The MACRA program encourages hospitals to reduce costs for acute care by including incentives. By doing this, it impacts cooperative activities between hospital partners and physicians. The MACRA program also ties physician payments to performance. Positive payment adjustments depend on each physician reaching quality and performance levels. This can be done by reducing visits to the emergency department, hospital admissions, and readmissions. The aim is to significantly increase the focus on keeping the patients out of the hospital (Pernisi et al., 2017).
The strength of the evidence available on the effectiveness of VBP programs in improving patient outcomes and health delivery is mixed and modest. By holding healthcare providers accountable for both quality of care and cost, the VBP system identifies and rewards best-performing providers and attempts to reduce inappropriate care (Chee et al., 2016).
References
Chee, T. T., Ryan, A. M., Wasfy, J. H., & Borden, W. B. (2016). Current State of Value-Based Purchasing Programs. Circulation, 133(22), 2197-2205. doi:10.1161/circulationaha.115.010268
Lee, S. J., Venkataraman, S., Heim, G. R., Roth, A. V., & Chilingerian, J. (2019). Impact of the value‐based purchasing program on hospital operations outcomes: An econometric analysis. Journal of Operations Management, 66(1-2), 151-175. doi:10.1002/joom.1057
Pernisi, L. , Lagoe, R. , Drapola, B. and Littau, S. (2017) Value Based Purchasing and Nursing Case Management. Open Journal of Nursing, 7, 307-317. doi: 10.4236/ojn.2017.72025.
Tanenbaum, S. J. (2016). What Is the Value of Value-Based Purchasing? Journal of Health Politics, Policy and Law, 41(5), 1033-1045. doi:10.1215/03616878-3632254
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
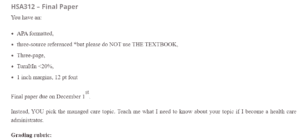
HSA312 – Final Paper
You have an:
Value-Based Purchasing
- APA formatted,
- three-source referenced *but please do NOT use THE TEXTBOOK,
- Three-page,
- TurnItIn <20%,
- 1 inch margins, 12 pt font
Final paper due on December 1st.
Instead, YOU pick the managed care topic. Teach me what I need to know about your topic if I become a health care administrator.
Grading rubric:
- 5 points per peer-reviewed reference used appropriately in the paper – you need in-text citations and full reference at the end of the paper,
- 10 points for overall formatting and attention to detail, and
- the other 75 points for compiling a cogent paper describing your managed care topic. What did you learn researching your topic? What has been the impact your topic had on the provision of care or health care outcomes or cost of care?
Topic: Value-Based Purchasing
Please follow instructions above while writing this paper please.