SOAP Note Template
S: Subjective
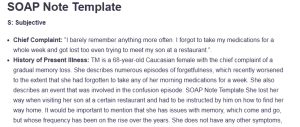
- Chief Complaint: “I barely remember anything more often. I forgot to take my medications for a whole week and got lost too even trying to meet my son at a restaurant.”.
- History of Present Illness: TM is a 68-year-old Caucasian female with the chief complaint of a gradual memory loss. She describes numerous episodes of forgetfulness, which recently worsened to the extent that she had forgotten to take any of her morning medications for a week. She also describes an event that was involved in the confusion episode: SOAP Note Template.She lost her way when visiting her son at a certain restaurant and had to be instructed by him on how to find her way home. It would be important to mention that she has issues with memory, which come and go, but whose frequency has been on the rise over the years. She does not have any other symptoms, including stomach pains, nausea, dizziness, or blurred vision. TM rules out a history of head trauma or recent infection.
- Past Medical History: The patient has hypertension, gastroesophageal reflux disease (GERD) and type 2 diabetes mellitus (DM2).
- Medications: Current medications include Pantoprazole Sodium DR 40 mg taken orally once daily for GERD, Metformin HCL 500 mg taken orally once daily for diabetes management, Seroquel 50 mg taken orally at bedtime, Venlafaxine 75 mg taken orally twice daily, Losartan Potassium 50 mg taken orally once daily for hypertension and Venlafaxine 75 mg taken orally once daily for depressed mood or a disturbed calm.
- Allergies: The patient has no known drug allergies (KNDA).
- Social History: TM refutes any history of smoking or alcohol use and aggressively contributes in community activities. She presently resides in an assisted living facility. Her primary language is Spanish, with English as her secondary language.
- Family History: Her mother and aunt both had dementia, indicating a potential genetic predisposition to neurocognitive disorders.
Review of Systems:
- Constitutional:
- ☐ Fever ☐ Weight loss ☐ Fatigue ☐ Weakness ☐ Other: __ Alert and oriented x3_________________
- Head, Eyes, Ears, Nose, Throat (HEENT):
- ☐ Headache ☐ Vision changes ☐ Hearing loss ☐ Nasal congestion ☐ Sore throat ☐ Other: ______ No abnormalities noted. Hearing intact bilaterally. Vision glasses present.
- Cardiovascular:
- ☐ Chest pain ☐ Palpitations ☐ Shortness of breath ☐ Edema ☐ Other: __________ No peripheral edema_________
- Respiratory:
- ☐ Cough ☐ Wheezing ☐ Hemoptysis ☐ Shortness of breath ☐ Other: __________ No cough_________
- Gastrointestinal:
- ☐ Nausea ☐ Vomiting ☐ Diarrhea ☐ Constipation ☐ Abdominal pain ☐ Other: _________No abnormalities__________
- Genitourinary:
- ☐ Dysuria ☐ Frequency ☐ Hematuria ☐ Urgency ☐ Incontinence ☐ Other: ____________ No abnormalities _______
- Musculoskeletal:
- ☐ Joint pain ☐ Muscle pain ☐ Stiffness ☐ Swelling ☐ Other: _____________ No abnormalities ______
- Neurological:
- ☐ Headaches ☐ Dizziness ☐ Numbness ☐ Tremors ☐ Seizures ☐ Other: _________ No signs of motor weakness __________
- Skin:
- ☐ Rash ☐ Itching ☐ Dryness ☐ Lesions ☐ Other: _____ No abnormalities ______________
- Endocrine:
- ☐ Weight changes ☐ Heat intolerance ☐ Cold intolerance ☐ Excessive thirst ☐ Other: ______________ No abnormalities _____
- Hematologic/Lymphatic:
- ☐ Easy bruising ☐ Bleeding ☐ Swollen glands ☐ Other: _____ No abnormalities ______________
O: Objective
- Vital Signs:
- Blood Pressure: 139/88 mmHg
- Heart Rate: 76 bpm
- Respiratory Rate: 16 breaths per minute
- Temperature: 97.2°F
- Physical Examination:
- General: Alert, oriented x3. Well-groomed. No signs of distress.
- HEENT: No abnormalities. Hearing intact bilaterally. Vision glasses present.
- Neurological: No motor weakness, normal reflexes, no tremors.
- Neck: No abnormalities noted.
- Cardiovascular: No peripheral edema.
- Pulmonary: No cough, clear lung sounds bilaterally.
Mental Status Exam:
- Appearance:
- ☐ Well-groomed ☐ Disheveled ☐ Poor hygiene ☐ Other: ___________________
- Behavior:
- ☐ Calm ☐ Agitated ☐ Cooperative ☐ Uncooperative ☐ Other: ___________________
- Speech:
- ☐ Normal rate ☐ Pressured ☐ Slow ☐ Incoherent ☐ Other: ___________________
- Mood:
- ☐ Euthymic ☐ Depressed ☐ Anxious ☐ Euphoric ☐ Other: ___________________
- Affect:
- ☐ Appropriate ☐ Flat ☐ Labile ☐ Inappropriate ☐ Congruent with stated mood ☐ Other: ___________________
- Thought Process:
- ☐ Logical ☐ Disorganized ☐ Tangential ☐ Circumstantial ☐ Other: ___________________
- Thought Content:
- ☐ No delusions ☐ Delusions ☐ Obsessions ☐ Preoccupations ☐ Other: ___________________
- Perceptions:
- ☐ No hallucinations ☐ Hallucinations ☐ Illusions ☐ Other: ___________________
- Cognition:
- Orientation:
- ☐ Oriented to person ☐ Oriented to place ☐ Oriented to time ☐ Oriented to situation
- Attention:
- ☐ Able to focus ☐ Easily distracted ☐ Difficulty concentrating ☐ Other: ___________________
- Memory:
- ☐ Intact ☐ Recent memory impaired ☐ Remote memory impaired ☐ Immediate memory impaired
- Abstract Thinking:
- ☐ Able to interpret proverbs ☐ Difficulty with abstract thinking ☐ Concrete thinking ☐ Other: ___________________
- Orientation:
- Insight:
- ☐ Good ☐ Fair ☐ Poor ☐ No insight ☐ Other: ___________________
- Judgment:
- ☐ Good ☐ Fair ☐ Poor ☐ Impaired ☐ Other: ___________________
A: Assessment
- Summary of Findings: TM has poor and progressive memory loss, impaired memory recall, and inability to perform serial computation. She scored twenty-three in SLUMS, indicating a mild level of neurocognitive impairment.
- Diagnosis:
Primary Diagnosis:
The patient primary diagnosis is Mild Neurocognitive Disorder due to Alzheimer’s Disease (Alzheimer’s Disease with Mild Neurocognitive Impairment) (ICD-10-G31.84 DSM-5-TR 331.83). This assessment is made on the basis of the patient’s presentation, which shows progressive memory loss, poor recall, confusion, and inability to do serial subtraction. Her SLUMS equals 23, which refers to mild neurocognitive impairment, and her family history of dementia provides an indication that Alzheimer’s disease is present (Carrillo et al., 2022).
The findings are indicative of early Alzheimer’s – the patient’s difficulties in immediate recall and the nature of her thinking that is circumstantial and tangential. Because there is no evidence of mood change, focal neurological signs, or cerebrovascular disease in this case, this is the most likely diagnosis.
Differential Diagnoses:
Another condition that this patient could have is Vascular Dementia (ICD-10: F01.50). The patient has a background of hypertension, which poses a danger of vascular dementia (Uwagbai & Kalish, 2020). However, she has no history of strokes or transient ischemic attacks on which this diagnosis can be based. Additionally, it should be noted that her symptoms are not worsening stepwise, as it usually happens with Alzheimer’s disease.
Besides another diagnosis includes Major Depressive Disorder with Cognitive Impairment (F33.1 ICD-10). Although the patient has a background of anxiety that is being treated by venlafaxine, she did not complain of depressive symptoms such as lack of pleasure in activities, persistent low mood, or social isolation. The deficits of cognitive function seem to be the main problem, thus ruling out depression with cognitive dysfunction as an issue (Rhee et al., 2024).
P: Plan
- Treatment Plan: The treatment plan for TM’s mild neurocognitive disorder due to Alzheimer’s disease is a multimodal plan using pharmacologic and nonpharmacologic strategies, patient education, and appropriate referrals. It aims to slow the rate of disease progression, improve cognitive function, maintain quality of life, and avoid health risks.
- Medications:
- Donepezil 5 mg per oral daily – This is the first-line treatment for cognitive impairment related to Alzheimer’s disease.
- Continue existing medications.
Non-Pharmacologic Treatments:
- Cognitive training exercises (puzzles, memory apps).
- Regular physical activity (walking 30 minutes daily).
- Social engagement through community activities.
- Mediterranean diet rich in omega-3 fatty acids.
Patient Education:
- Educated TM and her son on memory impairment and medication adherence.
- Recommended pill organizers and phone reminders.
- Discussed home safety modifications (labels, night lights).
Referrals:
- Neurology Consultation
- Geriatric Psychiatry Referral
- Social Worker Consultation
Laboratory Testing:
- CBC, CMP, TSH, Vitamin B12
- MRI Brain
- To Come Again (TCA) Re-evaluate the patient in 4 weeks to assess the response of medication on cognitive status.
Rationale
Justification for Treatment Plan:
- In the given case of mild neurocognitive disorder due to Alzheimer’s disease, the following treatment plan is proposed, which corresponds to the advanced and recent guidelines for the management of this condition. According to Kumar et al. (2023), donepezil, a cholinesterase inhibitor, is used as a first-line therapy as recommended by the American Academy of Neurology (AAN) and the Alzheimer’s Association as it has been proven effective in delaying the progression of the disease and enhancing functional activities in patients with moderate Alzheimer’s disease.Therefore, cognitive training exercise, social engagement, and different forms of exercise and workouts are some of the non-pharmacological interventions that have proven to have some level of efficiency in enhancing the reserve and slowing the advancement of the disease. As mentioned by Klimova et al. (2021), adherence to the Mediterranean-style diet characterized by omega-3 fatty acids and antioxidants contributes to more desirable cognitive results in older adults.CBC, CMP, TSH, and Vitamin B12 also should be conducted to exclude other treatable causes or contributing factors to dementia. An MRI brain scan is needed to determine other structural changes in the brain associated with Alzheimer’s or vascular dementia. It is important to follow up with patients on a regular basis to assess the changes in the diseases or success in response to treatment.
References
Carrillo, P., Rey, R., Padovan, C., Herrmann, M., & Dorey, J.-M. (2022). Association between mild neurocognitive disorder due to Alzheimer’s disease and possible attention-deficit/hyperactivity disorder: A case report. Journal of Psychiatric Practice, 28(3), 251–258. https://doi.org/10.1097/pra.0000000000000627
Klimova, B., Novotny, M., Schlegel, P., & Valis, M. (2021). The effect of Mediterranean diet on cognitive functions in the elderly population. Nutrients, 13(6), 2067. https://doi.org/10.3390/nu13062067
Kumar, A., Sharma, S., & Gupta, V. (2023, August 17). Donepezil. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513257/
Rhee, T. G., Shim, S. R., Manning, K. J., Tennen, H. A., Kaster, T. S., D’Andrea, G., Forester, B. P., Nierenberg, A. A., McIntyre, R. S., & Steffens, D. C. (2024). Neuropsychological assessments of cognitive impairment in major depressive disorder: A systematic review and meta-analysis with meta-regression. Psychotherapy and Psychosomatics, 93(1), 8–23. https://doi.org/10.1159/000535665
Uwagbai, O., & Kalish, V. B. (2020). Vascular dementia. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430817/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
SOAP Note Assignment
For the SOAP Note Assignment: You will document a SOAP note on the geriatric client who presented with a neurocognitive disorder. Use the Focused SOAP Note Template provided.
The assignment has the following requirements:
Focused SOAP Note
- Develop a Focused SOAP Note on the client using the template provided in these instructions
- You must add a title page and reference page. The title page and reference page must be in APA format.
- Include at least three peer-reviewed resources published within the last five years to support your assessment, diagnosis, and treatment planning.
SOAP Note Template
Criteria
Patient Demographic Information
Submits demographic information as specified on the SOAP Note Template.
Chief Complaint
Chief compliant is present and placed in quotation marks to indicate the client’s words.
Review of Systems
A full review of systems pertaining to the patient’s complaint/s is present
Current Medications
Current medications are present including the name, dose, route, and frequency.
Subjective Information
All subjective information is documented appropriately and thoroughly
Objective Information
A focused exam related to the client’s chief complaint is presented. A full mental status exam is documented.
Assessment
This includes DSM-V-TR diagnosis/diagnoses, and ICD-10 code/s. Assessment data/diagnosis must correspond to the chief complaint and subjective information given by the patient
Plan
Must include full treatment plan (pharmacological, non-pharmacological treatments, patient education, referrals, laboratory testing, and follow-up). A rationale is required to support your treatment plan based on the diagnosis.
APA Format and References
A title page and reference page in APA format must be included. The APA 7th edition should be used. References should be published within the last five years.