SOAP Note – Sleep-Wake Disorder
S: Subjective
- Chief Complaint: “I have trouble falling asleep and staying asleep. Sometimes, I can’t sleep through the night, and there are nights that I only sleep for a few hours at most.”
- History of Present Illness: AB is a Caucasian lady aged 82 years who presented with symptoms of insomnia for a few months duration. She also complains of sleep onset insomnia as well as middle insomnia. She lies awake at night, and sometimes she does not sleep at all, while at other moments, she only gets a few hours of sleep at night. This has been reported to have been going on for some months, and perhaps it starts during daytime functioning. The patient has never mentioned or demonstrated any suicidal thoughts or plans, homicidal thoughts, visual hallucinations, auditory hallucinations, or any intention to harm his body.
- Past Medical History:
- Hypertension
- Tinnitus
- Hearing impairment
- Medications:
- Losartan potassium 100 mg daily
- Atenolol 25 mg daily
- Desvenlafaxine succinate ER 25 mg daily
- Allergies: None known to date (KNDA)
- Social History: She is a retired lady and strongly confirmed that she has never in any way taken any alcohol, cigarettes, or drugs. She is also a happy wife and is blessed with three children. She is married happily to her husband.
- Family History: Grandmother had a history of depression
Review of Systems:
- Constitutional:
- ☐ Fever ☐ Weight loss ☐ Fatigue þ Weakness þ Other: ____ Appears alert and oriented x3_______________
- Head, Eyes, Ears, Nose, Throat (HEENT):
- ☐ Headache þ Vision changes þ Hearing loss ☐ Nasal congestion ☐ Sore throat ☐ Other: ___________________
- Cardiovascular:
- ☐ Chest pain ☐ Palpitations ☐ Shortness of breath ☐ Edema þ Other: ________ No peripheral edema___________
- Respiratory:
- ☐ Cough ☐ Wheezing ☐ Hemoptysis ☐ Shortness of breath þ Other: _________No respiratory problem__________
- Gastrointestinal:
- ☐ Nausea ☐ Vomiting ☐ Diarrhea ☐ Constipation ☐ Abdominal pain þ Other: ____________No GI problem noted_______
- Genitourinary:
- ☐ Dysuria ☐ Frequency ☐ Hematuria ☐ Urgency ☐ Incontinence þ Other: ____________ No abnormalities raised_______
- Musculoskeletal:
- ☐ Joint pain ☐ Muscle pain ☐ Stiffness ☐ Swelling þ Other: __No abnormalities____
- Neurological:
- ☐ Headaches ☐ Dizziness ☐ Numbness ☐ Tremors ☐ Seizures þ Other: ___No signs of motor weakness _______
- Skin:
- ☐ Rash ☐ Itching ☐ Dryness ☐ Lesions þ Other: __No abnormalities_____
- Endocrine:
- ☐ Weight changes ☐ Heat intolerance ☐ Cold intolerance ☐ Excessive thirst þ Other: ____No abnormalities_______
- Hematologic/Lymphatic:
- ☐ Easy bruising ☐ Bleeding ☐ Swollen glands þ Other: __No abnormalities______
O: Objective
- Vital Signs:
- Blood Pressure: 149/90 mmHg
- Heart Rate: 75 bpm
- Respiratory Rate: 19 breaths per minute
- Temperature: 98.1°F
- PHQ-9 Score: 17 (Moderate Depression)
- GAD-7 Score: 12 (Moderate Anxiety)
Physical Examination:
- General: Appears alert and oriented x3
- HEENT: Hearing impaired bilaterally, wears corrective glasses
- Neurological: No motor weakness, normal reflexes, no tremors
- Neck: No abnormalities noted
- Cardiovascular: No peripheral edema
- Pulmonary: Clear to auscultation, no cough noted
Mental Status Exam:
- Appearance:
- ☐ Well-groomed ☐ Disheveled ☐ Poor hygiene þ Other: __Appears stated age, well-groomed_______
- Behavior:
- ☐ Calm ☐ Agitated þ Cooperative ☐ Uncooperative ☐ Other: _____________
- Speech:
- þ Normal rate ☐ Pressured ☐ Slow ☐ Incoherent ☐ Other: _____________
- Mood:
- ☐ Euthymic ☐ Depressed þ Anxious ☐ Euphoric ☐ Other: _____________
- Affect:
- þ Appropriate ☐ Flat ☐ Labile ☐ Inappropriate þ Congruent with stated mood ☐ Other: ___________________
- Thought Process:
- þ Logical ☐ Disorganized ☐ Tangential ☐ Circumstantial ☐ Other: __________
- Thought Content:
- þ No delusions ☐ Delusions ☐ Obsessions ☐ Preoccupations ☐ Other: _______
- Perceptions:
- ☐ No hallucinations þ Hallucinations ☐ Illusions ☐ Other: _________________
- Cognition:
- Orientation:
- þ Oriented to person þ Oriented to place þ Oriented to time þ Oriented to situation
- Attention:
- þ Able to focus ☐ Easily distracted ☐ Difficulty concentrating ☐ Other: ___________________
- Memory:
- þ Intact ☐ Recent memory impaired ☐ Remote memory impaired ☐ Immediate memory impaired
- Abstract Thinking:
- þ Able to interpret proverbs ☐ Difficulty with abstract thinking ☐ Concrete thinking ☐ Other: ___________________
- Orientation:
- Insight:
- þ Good ☐ Fair ☐ Poor ☐ No insight ☐ Other: ___________________
- Judgment:
- þ Good ☐ Fair ☐ Poor ☐ Impaired ☐ Other: ___________________
A: Assessment
- Summary of Findings:
AB is an 82-year-old female who came with a chief complaint of insomnia. These include the inability to fall and stay asleep, resulting in poor-quality sleep. This may be caused by her history of hypertension, tinnitus, and hearing impairment. In light of her age, certain behaviours could also be related to physiological changes that occur during aging as well as medical and psychiatric issues, for instance, depression and anxiety. She also complains of hearing other people’s thoughts, which could be a manifestation of a psychological or neurologic pathology. However, she does not necessarily exhibit signs of psychosis, and there remains no suggestion of suicidal thoughts. The PHQ-9 assessment gives a total of 17 and GAD-7 of 12, which indicates moderate depression and anxiety that may have a role to play in chronic insomnia.
- Diagnosis:
- Primary Diagnosis: The primary diagnosis for AB is Insomnia Disorder (ICD-10: G47.00, DSM-5-TR: 780.52). This is evidenced by the chronic insomnia that has been complained of for several months regarding AB, with difficulty in falling asleep as well as difficulty remaining asleep. Her sleep disturbance implies that her nights may be completely sleepless, or she will only be able to get a few hours of sleep. Furthermore, no medical or psychiatric illness can be listed as the cause of the described sleep disorders and as an exclusion to the diagnosis of insomnia disorder at the same time. Based on the patient’s presentation and being a chronic patient, this case can be diagnosed under the DSM-5-TR and ICD-10 as insomnia (Riemann et al., 2022). As for the existing diseases of the client, hypertension and hearing impairment cannot be regarded as the reason for the sleep disorder.
- Differential Diagnoses
- Generalized Anxiety Disorder (GAD) (ICD-10: F41.1, DSM-5-TR: 300.02)
- The other possible diagnosis is Generalized Anxiety Disorder (GAD). In addition to fatigue, AB has other signs of anxiety, such as difficulty in making her mind relax, which may be causing her sleeplessness. Therefore, GAD can lead to early consumption of food and drinks, which may be taken due to excessive worrying, restlessness and hyperarousal, which can interfere with sleep (Munir & Takov, 2022). It is clear that AB does not have GAD, but anxiety could be the reason for her sleep disturbance. Nonetheless, the lack of excessive rumination and preoccupations implies that although anxiety can be found in insomniacs, it is not the primary concern for her.
- Major Depressive Disorder (MDD) (ICD-10: F33.1, DSM-5-TR: 296.32)
- The other diagnosis to be considered is Major Depressive Disorder (MDD). It is also worth highlighting the fact that sleep disorders are typical for those who have depression. Still, AB, as has been mentioned before, does not show evident signs of depression, although her chronic insomnia may point to the presence of a mood disorder. The absence of other depressive symptoms, such as persistent low mood, anhedonia (loss of interest in activities), or hopelessness, lowers the likelihood of MDD (Marx et al., 2023). However, it remains a possibility that should be monitored, as insomnia is frequently an early sign of depression.
- Sleep Apnea (ICD-10: G47.30, DSM-5-TR: 327.23)
Sleep apnea is an important differential diagnosis, especially in older people. It is defined by recurrent episodes of upper airway obstruction during sleep with consequent fragmented and non-restorative sleep, as noted by Cumpston and Chen (2023). While AB does not have the usual symptoms of loud snoring or witnessed apneas, her chronic insomnia, frequent nighttime awakenings, and daytime somnolence are suggestive. Her background of hypertension also increases the risk, as sleep apnea, if not treated, has cardiovascular implications. This condition is usually undiagnosed in older people, particularly those without a bed partner. A sleep study (polysomnography) would be indicated to establish or eliminate this diagnosis.
P: Plan
- Treatment Plan: The treatment plan for AB’s insomnia disorder is designed to provide both immediate relief and long-term management strategies that address the underlying causes of her sleep difficulties. The plan integrates pharmacological and non-pharmacological approaches and patient education to optimize outcomes.
- Medications:
- Initiate Mirtazapine 7.5–15 mg PO at bedtime to support sleep and mood.
- Review current antidepressant (Desvenlafaxine) – Consider switching to Mirtazapine if anxiety or depression symptoms are present.
- Continue existing medications (Losartan, Atenolol).
- Non-Pharmacological Treatments
- Cognitive Behavioral Therapy for Insomnia (CBT-I) – Focused on addressing sleep-related thoughts and behaviours.
- Sleep Hygiene Education – Consistent sleep-wake schedule and optimized sleep environment.
- Relaxation Techniques – Deep breathing and progressive muscle relaxation exercises.
- Patient Education:
- Educated AB about the use of Mirtazapine for sleep support and the benefits of CBT-I
- Recommended pill organizers and phone reminders for medication adherence.
- Discussed home safety modifications (e.g., labels, night lights).
- Referrals:
- CBT-I-trained therapist for sleep therapy.
- Psychiatric referral if depression or anxiety symptoms worsen.
- Laboratory Testing:
- CBC, Vitamin B12, and TSH to rule out medical causes of insomnia.
- Consider brain MRI if neurological concerns arise.
- Follow-Up: Re-evaluate in 2-4 weeks to assess treatment effectiveness and adjust as needed.
Rationale
- Justification for Treatment Plan: In treating AB’s insomnia disorder, the pharmacological and non-pharmacological approaches, as well as supportive approaches to managing her condition, are employed to provide her with the best solution. The administration of Mirtazapine is due to its dual role in treating sleep disturbances and mood disorders, which are not only the patient’s PHQ-9 score of 17 and GAD-7 score of 12. In elderly patients with both insomnia and mood disorders, Mirtazapine is useful because lower doses have sedative properties, and it has a side effect profile that is favourable for use in elderly patients (Jilani et al., 2022). In addition, AB’s current antidepressant, Desvenlafaxine, used for the treatment of major depressive disorder, may pose a risk of causing sleep disturbances.
CBT-I and other non-pharmacological interventions can be used as maintenance interventions for chronic insomnia. CBT-I is the best evidence-based treatment for insomnia that addresses negative cognitions and behaviours that maintain sleep disturbances, according to Walker et al. (2022). It has been observed to provide significant impacts through a fuller night’s sleep without medication. In addition to CBT-I, sleep hygiene education is essential to enhance AB’s sleep quality as it involves modifying her sleeping conditions and habits. AB will be able to use deep breathing exercises to reduce her anxiety because anxiety can lead to sleep disruption in patients.
Education is part of the management plan for effectively using Mirtazapine and integrating CBT-I as long-term goals. The following interventions will be taken regarding medication regimen compliance: Patient AB will be given pillboxes and phone alarms as tools. To provide comprehensive AB whole-person care, both a referral to a CBT-I trained therapist and psychiatry must be made. Any possible medical cause for its development should be excluded, so the patient needs to take CBC, Vitamin B12, and TSH, though if the patient has any neurological signs, she must have an MRI of the brain. The follow-up is done after 2-4 weeks, after which the effectiveness of the treatment is evaluated, and modification of the treatment can be done if necessary. This is more global and, as a result, an efficient approach toward treating the insomnia disorder that affects AB.
References
Cumpston, E., & Chen, P. (2023). Sleep apnea syndrome. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/33232089/
Jilani, T. N., Gibbons, J. R., Faizy, R. M., & Saadabadi, A. (2024). Mirtazapine. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/30085601/
Marx, W., Penninx, B. W. J. H., Solmi, M., Furukawa, T. A., Firth, J., Carvalho, A. F., & Berk, M. (2023). Major depressive disorder. Nature Reviews Disease Primers, 9(1). https://doi.org/10.1038/s41572-023-00454-1
Munir, S., & Takov, V. (2022, October 17). Generalized anxiety disorder. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/28722900/
Riemann, D., Benz, F., Dressle, R. J., Espie, C. A., Johann, A. F., Blanken, T. F., Leerssen, J., Wassing, R., Henry, A. L., Kyle, S. D., Spiegelhalder, K., & Van Someren, E. J. W. (2022). Insomnia disorder: State of the science and challenges for the future. Journal of Sleep Research, 31(4). https://doi.org/10.1111/jsr.13604
Walker, J., Muench, A., Perlis, M. L., & Vargas, I. (2022). Cognitive behavioural therapy for insomnia (CBT-I): A Primer. Klin Spec Psihol, 11(2), 123–137. https://doi.org/10.17759/cpse.2022110208
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
SOAP Note – Sleep-Wake Disorder
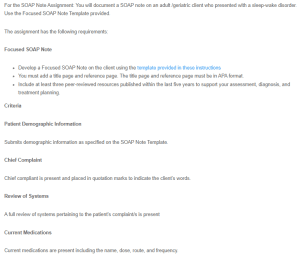
For the SOAP Note Assignment: You will document a SOAP note on an adult /geriatric client who presented with a sleep-wake disorder. Use the Focused SOAP Note Template provided.
SOAP Note – Sleep-Wake Disorder1
The assignment has the following requirements:
Focused SOAP Note
- Develop a Focused SOAP Note on the client using the template provided in these instructions
- You must add a title page and reference page. The title page and reference page must be in APA format.
- Include at least three peer-reviewed resources published within the last five years to support your assessment, diagnosis, and treatment planning.
Criteria
Patient Demographic Information
Submits demographic information as specified on the SOAP Note Template.
Chief Complaint
Chief compliant is present and placed in quotation marks to indicate the client’s words.
Review of Systems
A full review of systems pertaining to the patient’s complaint/s is present
Current Medications
Current medications are present including the name, dose, route, and frequency.
Subjective Information
All subjective information is documented appropriately and thoroughly
Objective Information
A focused exam related to the client’s chief complaint is presented. A full mental status exam is documented.
Assessment
This includes DSM-V-TR diagnosis/diagnoses, and ICD-10 code/s. Assessment data/diagnosis must correspond to the chief complaint and subjective information given by the patient
Plan
Must include full treatment plan (pharmacological, non-pharmacological treatments, patient education, referrals, laboratory testing, and follow-up). A rationale is required to support your treatment plan based on the diagnosis.
APA Format and References
A title page and reference page in APA format must be included. The APA 7th edition should be used. References should be published within the last five years.