SOAP Note – Chlamydia
ID:
Client’s Initials: D.B. | Age: 28 | Race: Caucasian | Gender: Female | DOB: January 1, 1996
The patient presented to the clinic alone. She is a reliable historian.
Subjective:
CC: “I have been experiencing a lot of pain when peeing.”
HPI:
D.B. is a 28-year-old Caucasian female presenting with complaints of pain during urination. The pain began one week ago and is localized in the lower abdominal region and the urogenital areas. The pain has been on and off over the past week but has increased significantly over the last three days. The pain is of a burning type and diffuses, mainly appearing during urination and shortly after urination. It is aggravated by urine holding and improved by voiding. The pain is present during the better part of the day and increases in intensity during urination. The patient scores the pain as 7/10. She also reports complaints of nausea and vomiting, frequent urination, and urinary urgency.
Past Medical History:
- Medical Problem List
- No known medical problems
- Negative history of an STI or a UTI
- Preventative Care:
- The patient had a dental checkup and a breast examination in March. Both tests were negative for any anomalies.
- Surgeries: None
- Hospitalizations: No reports of past hospitalizations
- LMP and Pregnancy Status:
- Her LMP date was 2/10/2024
Immunizations: The patient is up to date with all of her immunizations, including a booster shot of the COVID-19 vaccine and the annual flu vaccine.
Allergies: No known food or drug allergies
Medications: The patient is on paracetamol 1g, taken every eight hours for the management of the pain. She started taking the drug three days ago.
Family History: The patient has no family history of any urinary tract or sexually transmitted infections.
Social History:
- Sexual history and contraception/protection: The patient is in a relationship and is sexually active. She engages in unprotected sexual intercourse and had sexual contact with her boyfriend ten days ago. She also notes that she has been suspecting her boyfriend of having other sexual partners. She denies using any other form of contraceptive. She also denies having had any sexually transmitted infections or urinary tract infections.
- Chemical history (tobacco/alcohol/drugs):The patient is a social smoker. She smokes at social events and occasionally over the weekends. She is also a binge alcohol drinker, drinking over the weekends and during parties. She has no recall of taking any hard drugs or narcotics.
Other: The patient is in a relationship with one male partner. She lives alone in a rented apartment and works as a receptionist. She takes a balanced diet regularly, including two cups of coffee on every workday. She rarely exercises. She is a staunch Catholic and sometimes attends church services.
Safety: The patient conforms to various safety practices, such as wearing a seat belt when driving. She does not own a gun.
ROS
- Constitutional:Denies weight loss. The patient reported experiencing fever and chills over the past 24 hours.
- EENT: Denies any visual change, eye discharge, or double visions. The patient also denies hearing loss, ear discharge, or any recent ear infections. Denies nasal congestion, sore throat, or any difficulty in swallowing.
- Cardiovascular: Denies palpitations, any irregularity in heart rate of rhythms, chest pain, or swelling in the extremities.
- Respiratory: Denies shortness of breath, wheezing, unusual coughs, or tachypnea. Respiratory symptoms such as labored breathing and coughs can be suggestive of pneumonia secondary to chlamydia infections.
- Gastrointestinal: The patient reported experiencing diffuse lower abdominal pain that radiates to the back. She also has occasional nausea. She has had multiple episodes of vomiting over the past three days.
- Genitourinary: The patient reported complaints of pain during urination for the past week. She also has a urinary frequency, urgency, and a malodorous discharge. She reported seeing blood spots in her underwear the past day despite not being in her period. She also has flank pain. She, however, denies post-coital bleeding, urinary incontinence, and dyspareunia.
- Musculoskeletal: Denies joint pain, joint stiffness, joint swelling, or reduction in the range of motion in her joints. Joint pain and swelling can be suggestive of reactive arthritis secondary to chlamydia infection.
- Neurological: Denies seizures, memory loss, or any changes in her personality.
Objective
Vital Signs:
HR: 89 beats per minute, 88 bpm on repeat | BP: 134/83mmHg, 129/82mmHg on repeat
Temp: 99.0 degrees F | RR: 16 breaths per minute | SpO2: 97%
Height: 6’0 | Weight 176.0 lbs | BMI: 23.5
Laboratory Findings
- Urinalysis on 9/10/2024: Performed to evaluate apparent UTI and an ST1.
The urine used for evaluation was obtained through spontaneous voiding on the initial contact with the patient.
- Physical Examination of the Urine: The urine is cloudy and malodorous.
- Biochemical Examination:
| Test | Result |
| Blood | Negative |
| Leukocytes | Positive |
| Nitrite | Positive |
| Protein | Negative |
| pH | 6 |
| Specific gravity | 1.030 |
| Glucose | Negative |
| Ketones | Negative |
| Bilirubin | Negative |
| Urobilinogen | 0.6 mg/dL |
- Complete Blood Count on 9/10/2024: A complete blood count (CBC) is warranted to check the presence of an inflammatory process. Inflammation is a predominant manifestation in urogenital conditions such as cervicitis and urethritis. A CBC panel may help point toward the diagnosis.
| Hematology | Result | Normal range |
| Red cell count | 5.5 x 1012/L | 4.5–5.7 |
| White cell count | 12 x 109/L | 4.0–10.0 |
| Hemoglobin | 156 g/L | 133–167 |
| Hematocrit | 0.49 | 0.35–0.53 |
| MCV | 93 fL | 77–98 |
| MCH | 31.9 pg | 26–33 |
| MCHC | 351 g/L | 330–370 |
| RDW | 13.5% | 10.3–15.3 |
- Nucleic acid amplification testing (NAAT): Pending
- Endocervical examination: Ordered
- Pregnancy test: Negative
Physical Exam
- General survey: The patient is alert. She responds to the interview questions asked appropriately. She is feverish and shivers occasionally during the interview.
- Eyes: The eyes are symmetrical. Vision is intact. No sign of eye discharge, puffiness, eyelid swelling, or erythema. The pupils are rounded and reactive to light.
- ENT: The ears are symmetrical. No sign of ear discharge or hearing loss. The nose is well-positioned on the face. No sign of nasal congestion or discharge. The uvula is midline. No signs of tonsilar swelling.
- Cardiovascular: The heart rate is regular and rhythmic. No signs of edema, pallor, or cyanosis. S1 and S2 sounds were heard. No murmur sounds were heard on auscultation.
- Chest/Thorax: The chest is symmetrical. No sign of a barrel chest or any chest deformity. There were also no signs of labored breathing, excessive coughing, or use of respiratory muscles for respiration. No wheezing or crackling sounds were heard on auscultation.
- Abdominal and pelvic: The abdominal wall is symmetrical. No sign of skin color inconsistencies, scars, abdominal masses, engorged veins, striae, or distension on abdominal inspection. Auscultation of the abdomen revealed low-pitched, gurgling sounds. No bruit sounds were heard over the aorta and the iliac and femoral arteries. Tympanic sounds could be heard on percussion. Light and deep palpation of the abdomen and the flanks revealed slight tenderness in the flanks. There was, however, no abdominal pain, crunching feeling or crepitus, abdominal pain, masses, or tenderness.
- Bladder exam: There were no signs of bladder hyper-extension on visual extension. No signs of skin indentation on the area above the bladder. No sign of fullness in the costovertebral angle.
- Musculoskeletal: No signs of joint swelling, pain, or tenderness. There were also no signs of restrictions in the range of motion of the phalangeal joints.
- Neurological: The patient is alert and responsive to the interview questions asked. She is also oriented to the place, time, and event of the day. Her memory is intact. Her judgment is also intact, goal-directed, and logical. Her speech is normal and consistent in tone and volume. Mood is euthymic.
Assessment
Differentials
- Chlamydia ICD-10 Code A74.9: Chlamydia is a sexually transmitted infection caused by a gram-negative bacteria, Chlamydia trachomatis. The disease primarily affects the cervix and may manifest as cervicitis, pelvic inflammatory disease, urethritis, proctitis, and perihepatitis. Chlamydia is transmitted through sexual contact. The symptoms of the disease may manifest within one to three weeks after contact. Patients with the disease often present diverse symptoms that correspond with the urogenital site affected. While many patients with the disease remain asymptomatic, many progress to manifest with the classic symptoms of dysuria, vaginal discharge, abdominal pain, and bleeding (Rodrigues et al., 2022). PID is one of the urogenital infections attributable to chlamydia infections. It occurs when the bacteria ascends to the upper reproductive tract. Patients with PID will report complaints of abdominal pain or flank pain alongside dysuria, dyspareunia, urinary urgency and frequency, and malodorous urine. Extragenital symptoms such as nausea, vomiting, lower back pain, fever, and chills are also common in PID secondary to chlamydia infections (Mitchell et al., 2021). In the case presented, the patient had pain during urination. Assessment findings revealed flank pain, fever, chills, nausea, and vomiting. Likewise, she is a sexually active woman who indulges in unprotected sexual intercourse. These manifestations are aligned with the CDC criteria for diagnosing chlamydia. This warranted the inclusion of this differential.
- Cervicitis ICD-10 Code N72: Cervicitis is a clinical syndrome resulting from an inflammation of the ectocervix. Cervicitis is a common finding in sexually active women. Cervicitis can have an infectious and a non-infectious etiology. Infectious causes include Neisseria gonorrhea, Chlamydia trachomatis, and vaginalis, among others. Non-infectious causes include chemical and mechanical irritants, such as pessaries, tampons, cervical caps, diaphragm, spermicides, soaps, and contraceptive creams, among others. Cervicitis may be acute or chronic. Assessment findings in cervicitis often reveal multiple sexual partners or partners with multiple sexual partners, use of pregnancy protection modalities such as spermicides, and previous STIs. The disease typically manifests with mucopurulent or purulent vaginal discharge, intramenstrual bleeding, dyspareunia, urinary symptoms such as dysuria, and pelvic pain. High fever and adnexal tenderness are also apparent in the disease (La Tabla & Gutiérrez, 2019). The patient in the case presented had urinary manifestations of urinary frequency, urgency, and dysuria. Likewise, she reported complaints of intermenstrual bleeding, high fever, and pelvic pain. Assessment findings confirmed adnexal tenderness. This meets the diagnostic criteria for cervicitis. An endocervical examination is warranted to rule out the diagnosis.
- Complicated urinary tract infections ICD 10 Code N39.0: Urinary tract infections (UTIs) are infections of the urogenital tract but may also affect the rectal and perineal areas. The most implicated organisms in UTI include Escherichia coli, Klebsiella, Enterococcus, and Pseudomonas. According to the CDC, a complicated UTI is any form of UTI that does not fit the criteria for a simple UTI. This includes simple cystitis, occasional recurrent cystitis, and a single episode of ascending pyelonephritis (Marantidis & Sussman, 2023). Patients with either form of UTI may present with manifestations of dysuria, urinary frequency and urgency, suprapubic pain, and hematuria. Complicated UTI differs from uncomplicated UTI in that it may also manifest with extragenital symptoms such as fever, chills, and flank pain. Septicaemia may be apparent in severe cases of complicated UTI. Unprotected sexual intercourse, pregnancy, obesity, urinary incontinence, and a family history of UTI are known risk factors for UTI (Marantidis & Sussman, 2023). The patient in the case presented had pain during urination and urinary frequency and urgency. Assessment findings revealed flank pain, fever, and chills. These manifestations are consistent with those of complicated UTIs, warranting the inclusion of this differential. The differential was ruled out due to the presence of vaginal discharge, as vaginal discharge is not a typical feature of UTI.
Diagnosis: The presumptive diagnosis is chlamydia infection. The urinary symptoms of urinary frequency, urgency, and dysuria and the presence of fever, chills, and flank pain point toward PID secondary to chlamydia infections. Assessment findings also revealed risk factors for chlamydia infections, such as unprotected sexual intercourse. The absence of vaginal discharge helped in ruling out complicated UTIs. The endocervical examination was negative for mucoid discharge and easy bleeding from the cervix, ruling out cervicitis. According to the CDC guidelines on the diagnostic considerations for cervicitis, the presence of a purulent or a mucopurulent endocervical exudate, seen on an endocervical swab specimen, or sustained endocervical bleeding on gentle passage of a cotton swab through the cervix warrants the diagnosis for cervicitis (CDC, 2022). This was, however, not the case in the case presented, ruling out the diagnosis.
Plan
Chlamydia ICD-10 Code A74.9
- Diagnostics and Laboratory workup:Nucleic acid amplification testing (NAAT) will be ordered. NAAT is the most specific and sensitive test for chlamydia and Neisseria. It helps identify the bacteria involved in the pathogenesis of the disease and subsequently directs the therapeutic approach for the patient. NAAT can be performed on urine samples or endocervical swabs (Van Ommen et al., 2023). Urine culture may also be ordered for the case presented. Urine culture is, however, less sensitive in detecting chlamydia. Likewise, chlamydia are obligate microorganisms that cannot be grown by conventional bacteriological medium. This makes bacterial cultures a less preferred option for diagnosing chalmydia. NAAT may also detect Neisseria gonorhea. Culture may help detect other microorganisms causing the identified symptoms (Van Ommen et al., 2023).
- STI screening: The patient will be screened for STIs. STI screening is recommended for all patients presenting with the symptoms of STI. According to the CDC guidelines, patients should be screened for HIV, syphilis, and gonorrhea whenever they are considered high-risk. The patient in the case presented is high risk as she has a sexual partner who may be having other sexual partners (CDC, 2022).
- Treatment: The patient will be started on doxycycline 100mg, administered orally every 12 hours for seven days. Doxycycline is an antibiotic that is effective in managing uncomplicated urogenital chlamydia infection. It is first line in managing chlamydia in adolescents and adults with urogenital chlamydia infections (CDC, 2021). It helps lower the risk of disease transmission and resolves the symptoms of chlamydia infections. Its use has, however, been associated with side effects such as diarrhea, headaches, and loss of appetite.
Azithromycin and levofloxacin are also available for use in chlamydia infections. Azithromycin is available as a single oral dose of 1g. It is preferred where doxycycline is contraindicated. Its once-daily dosing makes it flexible and may increase its acceptability among diverse patient groups. It has, however, been associated with side effects such as GI disturbance and QT prolongation.
Levofloxacin is a fluoroquinolone antibiotic administered orally. The 500mg once daily dosing for seven days remains effective in addressing the symptoms of chlamydia. This medication is preferred where a suboptimal response is seen after therapy with doxycycline and in patients in whom doxycycline is contraindicated.
- Patient Education:
- Disease Process: The patient will be educated on the disease process. She will be informed that chlamydia is a sexually transmitted infection contracted through sexual contact with an infected person. She will also be educated on the available therapeutic options and the significance of medications in managing the disease. In this case, the prescribed antibiotic will help address her symptoms as well as minimize her chances of transmitting the disease. The patient will also be informed that if the disease is left untreated, it may result in several complications, such as ectopic pregnancy, infertility, and chronic pelvic pain, among others. It is thus important that the patient follows administration instructions given to her (CDC, 2021).
- Medication: The patient will be advised to take the prescribed doxycycline for the entire seven-day therapy period. She will also be told of the potential side effects, such as GI disturbances, and advised to report to the clinic whenever she experiences severe side effects, such as skin reactions. Skin reaction may be suggestive of a hypersensitivity reaction.
- Sexual Behaviors: The patient will also be educated on sexual behaviors that predispose her to STIs. In this respect, she will be told that having unprotected sex and sexual partners with other sexual partners makes her vulnerable to sexually transmitted infections such as syphilis, chlamydia, HIV, and gonococcal disease. Additionally, having a partner who has other sexual partners puts her at high risk of contracting sexually transmitted infections. The patient should also be advised to talk to her partner to seek therapy. Chlamydia may be asymptomatic in some individuals. This, however, does not reduce their potential to transmit the disease to others. Therefore, the partner must also be treated to prevent him from reinfecting the patient (CDC, 2021).
- Healthcare-Seeking Behavior: The patient should be educated on the significance of routine STI screening. The United States Preventive Service Task Force recommends that all sexually active women should be screened for chlamydia, pelvic inflammatory disease, and infertility. This can help detect early disease and inform therapeutic measures (CDC, 2021).
- Follow-up: The patient is expected to return for follow-up after one week. This will allow caregivers to determine whether the symptoms have resolved. The patient should, however, be advised to return whenever she feels her symptoms are not going away, as this may allow for medication revision (CDC, 2021).
References
CDC. (2021, July 22). Chlamydial infections – STI treatment guidelines. Centers for Disease Control and Prevention. https://www.cdc.gov/std/treatment-guidelines/chlamydia.htm
CDC. (2022, September 21). Urethritis and cervicitis – STI treatment guidelines. Centers for Disease Control and Prevention. https://www.cdc.gov/std/treatment-guidelines/urethritis-and-cervicitis.htm#:~:text=Two%20major%20diagnostic%20signs%20characterize,of%20a%20cotton%20swab%20through
La Tabla, V. O., & Gutiérrez, F. (2019). Cervicitis: Etiology, diagnosis and treatment. Enfermedades Infecciosas Y Microbiologia Clinica (English Ed), 37(10), 661–667. https://doi.org/10.1016/j.eimce.2018.12.011
Marantidis, J., & Sussman, R. D. (2023). Unmet needs in complicated urinary tract infections: Challenges, recommendations, and emerging treatment pathways. Infection and Drug Resistance, 16, 1391–1405. https://doi.org/10.2147/idr.s382617
Mitchell, C. M., Anyalechi, G. E., Cohen, C. R., Haggerty, C. L., Manhart, L. E., & Hillier, S. L. (2021). Etiology and diagnosis of pelvic inflammatory disease: Looking beyond gonorrhea and chlamydia. The Journal of Infectious Diseases, 224(Supplement_2). https://doi.org/10.1093/infdis/jiab067
Rodrigues, R., Sousa, C., & Vale, N. (2022). Chlamydia trachomatis as a current health problem: Challenges and opportunities. Diagnostics, 12(8), 1795. https://doi.org/10.3390/diagnostics12081795
Van Ommen, C. E., Malleson, S., & Grennan, T. (2023). A practical approach to the diagnosis and management of chlamydia and gonorrhea. Canadian Medical Association Journal, 195(24). https://doi.org/10.1503/cmaj.221849
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
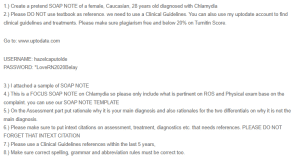
1.) Create a pretend SOAP NOTE of a female, Caucasian, 28 years old diagnosed with Chlamydia
2.) Please DO NOT use textbook as reference. we need to use a Clinical Guidelines. You can also use my uptodate account to find clinical guidelines and treatments. Please make sure plagiarism free and below 20% on Turnitin Score.
SOAP Note – Chlamydia
Go to: www.uptodate.com
USERNAME: hazelcaputolde
PASSWORD: *LoveRN2020Belay
3.) I attached a sample of SOAP NOTE
4.) This is a FOCUS SOAP NOTE on Chlamydia so please only include what is pertinent on ROS and Physical exam base on the complaint. you can use our SOAP NOTE TEMPLATE
5.) On the Assessment part put rationale why it is your main diagnosis and also rationales for the two differentials on why it is not the main diagnosis.
6.) Please make sure to put intext citations on assessment, treatment, diagnostics etc. that needs references. PLEASE DO NOT FORGET THAT INTEXT CITATION
7.) Please use a Clinical Guidelines references within the last 5 years,
8.) Make sure correct spelling, grammar and abbreviation rules must be correct too.