SOAP NOTE
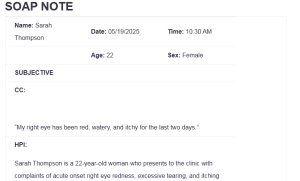
| Name: Sarah Thompson | Date: 05/19/2025 | Time: 10:30 AM |
| Age: 22 | Sex: Female | |
| SUBJECTIVE | ||
| CC:
“My right eye has been red, watery, and itchy for the last two days.” |
||
| HPI:
Sarah Thompson is a 22-year-old woman who presents to the clinic with complaints of acute onset right eye redness, excessive tearing, and itching that started approximately two days ago. She describes the irritation as constant, with a gritty sensation and mild discharge, especially in the morning: SOAP NOTE. There is no associated pain or changes in vision. She denies trauma, foreign body, or contact lens use. No similar symptoms in the left eye. She works as a barista, and reports increased exposure to dust and coffee steam. She has no recent illness, but she noted some co-workers had “colds” recently. No photophobia or systemic symptoms. No history of similar episodes in the past. |
||
| Medications:
Multivitamin, daily – general wellness Ibuprofen 200 mg PRN – occasional headaches |
||
| PMH
Allergies: No known drug allergies (NKDA)
Medication Intolerances: None reported Chronic Illnesses/Major traumas None Hospitalizations/Surgeries Tonsillectomy at age 8 Has never been diagnosed with Diabetes, hypertension, peptic ulcer disease, asthma, lung disease, heart disease, cancer, TB, thyroid or kidney disease, or any psychiatric disorder. |
||
| Family History
Mother – Seasonal allergies Father – Hypertension No family history of eye diseases, diabetes, cancer, TB, or kidney disease. |
||
| Social History
Single, lives alone in a shared apartment. Currently employed as a barista. Non-smoker, drinks alcohol occasionally (1-2 drinks per week), no drug use. No recent travel. Feels safe at home and work. |
||
| ROS | |
| General
No fever, chills, fatigue, or weight changes |
Cardiovascular
No chest pain, palpitations, or edema |
| Skin
No rashes or lesions |
Respiratory
No cough, wheezing, or dyspnea |
| Eyes
Right eye redness, tearing, itching, mild discharge, no vision loss or photophobia |
Gastrointestinal
No nausea, vomiting, or abdominal pain |
| Ears
No pain or discharge |
Genitourinary/Gynecological
No complaints, regular cycles, no STIs |
| Nose/Mouth/Throat
No nasal discharge, sore throat, or congestion |
Musculoskeletal
No joint pain or swelling |
| Breast
No lumps or concerns |
Neurological
No headaches, dizziness, or weakness
|
| Heme/Lymph/Endo
No swollen glands, no heat or cold intolerance |
Psychiatric
No depression, anxiety, or sleep disturbances |
| OBJECTIVE | |
| Weight 140 lbs BMI 22.6 | Temp 98.7°F | BP 112/68 mmHg |
| Height 5’5″ | Pulse 76 bpm | Resp 16 breaths/min |
| General Appearance
Healthy young adult female, alert and oriented, appears mildly uncomfortable due to eye symptoms. |
||
| Skin
Skin is warm, dry, and intact. No lesions or rashes were noted. |
||
| HEENT
The head is normocephalic and atraumatic. The right eye shows conjunctival injection, clear watery discharge, and mild eyelid edema, but pupils are equal, round, and reactive to light and accommodation (PERRLA), with extraocular movements intact (EOMI). There is no photophobia, corneal clouding, or presence of a foreign body. The left eye appears normal. Ears, nose, and throat are unremarkable, with no erythema, drainage, or lymphadenopathy. The neck is supple, without cervical adenopathy or thyromegaly. |
||
| Cardiovascular
S1, S2 regular, no murmurs, rubs, or gallops. |
||
| Respiratory
Clear to auscultation bilaterally. |
||
| Gastrointestinal
Abdomen soft, nontender, normoactive bowel sounds. |
||
| Breast
Free of masses, no other concerns reported. |
||
| Genitourinary
The bladder is non-distended; no CVA tenderness. No other concerns were reported. |
||
| Musculoskeletal
Normal ROM in extremities. |
||
| Neurological
Alert, oriented x3, normal gait and coordination. |
||
| Psychiatric
Appropriate mood and affect, cooperative. |
||
| Lab Tests
None were ordered at this visit |
| Special Tests
Fluorescein Stain Test: Not performed. No signs of corneal abrasion or ulcer based on clinical evaluation.
Visual Acuity Test: Normal in both eyes (20/20), no reported vision changes.
Eversion of Eyelid: Not performed due to absence of foreign body sensation or trauma.
Photophobia Test: Negative. No discomfort upon light exposure.
Lymph Node Palpation: No preauricular or cervical lymphadenopathy was palpated.
|
| Diagnosis |
| Differential Diagnoses
o 1- Acute follicular conjunctivitis, right eye (ICD-10 Code: H10.021) – This condition is typically viral and marked by the formation of follicles—small, round elevations—on the inner conjunctiva. It often causes redness, watery discharge, and a gritty feeling in the eye (Hashmi et al., 2024). The patient’s clinical presentation aligns with this diagnosis, especially in the absence of thick discharge. However, no follicles were specifically noted during the examination, making this a potential but unconfirmed etiology. o 2- Acute atopic conjunctivitis, right eye (ICD-10 Code: H10.121) – Allergic conjunctivitis associated with atopic conditions like eczema or asthma. It usually presents bilaterally with severe itching and tearing (Hashmi et al., 2024). In this case, the unilateral involvement and absence of an allergy history make this diagnosis less likely, though the presence of itching keeps it on the differential list. o 3 – Conjunctivitis due to adenovirus (ICD-10 Code: B30.1) – Adenoviral conjunctivitis is highly contagious and common in close-contact environments. Symptoms include redness, watery discharge, and a gritty sensation in the eye, typically beginning unilaterally (Muto et al., 2023). The patient’s workplace exposure to sick colleagues and the nature of her symptoms make this a strong possible cause, though not confirmed without diagnostic testing. Diagnosis o Unspecified acute conjunctivitis, right eye (ICD-10 Code: H10.30)- This diagnosis is used when a patient presents with symptoms of acute conjunctival inflammation, such as redness, tearing, and irritation, without a confirmed underlying etiology (Hashmi et al., 2024). In this case, the symptoms strongly suggest a viral source due to the watery discharge and lack of purulence, combined with recent exposure to sick co-workers. However, without a lab confirmation, the unspecified code is appropriate for documentation and treatment planning.
|
| Plan/Therapeutics |
| o Plan:
§ Further testing At this time, no laboratory tests or imaging are needed. The clinical presentation is straightforward and consistent with mild, likely viral conjunctivitis. However, the plan includes clear guidance that if the symptoms do not resolve within 5–7 days or begin to worsen (e.g., severe pain, visual changes, or thick purulent discharge), additional testing such as a conjunctival swab, culture, or referral to an ophthalmologist may be considered. This ensures patient safety through appropriate monitoring. § Medication Artificial tears are recommended to soothe eye irritation and flush out any potential viral particles or allergens. These can be used every four hours as needed. Ketotifen eye drops help relieve itchiness, so over-the-counter use of this drug is recommended if the itching becomes more bothersome (Rwizi et al., 2024). There was no use of antibiotics since the symptoms told us it was not due to bacteria. § Education Teaching patients is very important when managing conjunctivitis. The patient was advised to practice eye hygiene by washing their hands, not touching their eyes and taking off their contact lenses as long as they had symptoms. She was told to avoid using towels, washcloths or makeup from others to make sure she does not infect the people around her. Framing the illness to last from 7 to 10 days helps patients understand the usual course of recovery. § Non-medication treatments Using a cool compress on the irritated eye can help reduce both the pain and swelling. Recovery is best supported by getting plenty of rest, and touching or rubbing the eye should be avoided. |
| Evaluation of patient encounter
The patient was assessed with a focused history and physical examination. The signs were indicative of viral conjunctivitis, and bacterial and allergic causes were ruled out. There were no prodromal signs like alteration of vision or photophobia. She was educated on hygiene, symptom management, and transmission prevention. Wet compresses and artificial tears were recommended. The patient acknowledged the plan of care asked questions, and the visit was concordant with best practice for management of acute viral conjunctivitis. |
References
Hashmi, M. F., Gurnani, B., & Benson, S. (2024, January 26). Conjunctivitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK541034/
Muto, T., Imaizumi, S., & Kamoi, K. (2023). Viral Conjunctivitis. Viruses, 15(3), 676. https://doi.org/10.3390/v15030676
Rwizi, S., Mushipe, T., Zulu, W., Annor, A., & Bronkhorst, E. (2024). Beat the itch: allergic conjunctivitis and its management. SA Pharmaceutical Journal., 91(4), 13–18. https://doi.org/10.36303/sapj.0807
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Client’s Notes:
- 22 year old woman with unspecified acute conjunctivitis of the right eye seen in primary care setting.
- Please use the same format from previous soap note assignments
| Name: | Date: | Time: |
| Age: | Sex: | |
| SUBJECTIVE | ||
| CC:
Reason given by the patient for seeking medical care “in quotes” |
||
| HPI:
Describe the course of the patient’s illness, including when it began, character of symptoms, location where the symptoms began, aggravating or alleviating factors; pertinent positives and negatives, other related diseases, past illnesses, surgeries or past diagnostic testing related to present illness. |
||
| Medications: (list with reason for med ) | ||
| PMH
Allergies:
Medication Intolerances:
Chronic Illnesses/Major traumas
Hospitalizations/Surgeries
“Have you every been told that you have: Diabetes, HTN, peptic ulcer disease, asthma, lung disease, heart disease, cancer, TB, thyroid problems or kidney disease or psychiatric diagnosis.” |
||
| Family History
Does your mother, father or siblings have any medical or psychiatric illnesses? Anyone diagnosed with: lung disease, heart disease, htn, cancer, TB, DM, or kidney disease. |
||
| Social History
Education level, occupational history, current living situation/partner/marital status, substance use/abuse, |
||
| ETOH, tobacco, marijuana. Safety status | |
| ROS | |
| General
Weight change, fatigue, fever, chills, night sweats, energy level |
Cardiovascular
Chest pain, palpitations, PND, orthopnea, edema |
| Skin
Delayed healing, rashes, bruising, bleeding or skin discolorations, any changes in lesions or moles |
Respiratory
Cough, wheezing, hemoptysis, dyspnea, pneumonia hx, TB |
| Eyes
Corrective lenses, blurring, visual changes of any kind |
Gastrointestinal
Abdominal pain, N/V/D, constipation, hepatitis, hemorrhoids, eating disorders, ulcers, black tarry stools |
| Ears
Ear pain, hearing loss, ringing in ears, discharge |
Genitourinary/Gynecological
Urgency, frequency burning, change in color of urine.
Contraception, sexual activity, STDS
Fe: last pap, breast, mammo, menstrual complaints, vaginal discharge, pregnancy hx
Male: prostate, PSA, urinary complaints |
| Nose/Mouth/Throat
Sinus problems, dysphagia, nose bleeds or discharge, dental disease, hoarseness, throat pain |
Musculoskeletal
Back pain, joint swelling, stiffness or pain, fracture hx, osteoporosis |
| Breast
SBE, lumps, bumps or changes |
Neurological
Syncope, seizures, transient paralysis, weakness, paresthesias, black out spells |
| Heme/Lymph/Endo
HIV status, bruising, blood transfusion hx, night sweats, swollen glands, increase thirst, increase hunger, cold or heat intolerance |
Psychiatric
Depression, anxiety, sleeping difficulties, suicidal ideation/attempts, previous dx |
| OBJECTIVE | |
SOAP NOTE
| Weight BMI | Temp | BP |
| Height | Pulse | Resp |
| General Appearance
Healthy appearing adult female in no acute distress. Alert and oriented; answers questions appropriately. Slightly somber affect at first, then brighter later. |
||
| Skin
Skin is brown, warm, dry, clean and intact. No rashes or lesions noted. |
||
| HEENT
Head is normocephalic, atraumatic and without lesions; hair evenly distributed. Eyes: PERRLA. EOMs intact. No conjunctival or scleral injection. Ears: Canals patent. Bilateral TMs pearly grey with positive light reflex; landmarks easily visualized. Nose: Nasal mucosa pink; normal turbinates. No septal deviation. Neck: Supple. Full ROM; no cervical lymphadenopathy; no occipital nodes. No thyromegaly or nodules. Oral mucosa pink and moist. Pharynx is nonerythematous and without exudate. Teeth are in good repair. |
||
| Cardiovascular
S1, S2 with regular rate and rhythm. No extra sounds, clicks, rubs or murmurs. Capillary refill 2 seconds. Pulses 3+ throughout. No edema. |
||
| Respiratory
Symmetric chest wall. Respirations regular and easy; lungs clear to auscultation bilaterally. |
||
| Gastrointestinal
Abdomen obese; BS active in all 4 quadrants. Abdomen soft, non-tender. No hepatosplenomegaly. |
||
| Breast
Breast is free from masses or tenderness, no discharge, no dimpling, wrinkling or discoloration of the skin. |
||
| Genitourinary
Bladder is non-distended; no CVA tenderness. External genitalia reveals coarse pubic hair in normal distribution; skin color is consistent with general pigmentation. No vulvar lesions noted. Well estrogenized. A small speculum was inserted; vaginal walls are pink and well rugated; no lesions noted. Cervix is pink and nulliparous. Scant clear to cloudy drainage present. On bimanual exam, cervix is firm. No CMT. Uterus is antevert and positioned behind a slightly distended bladder; no fullness, masses, or tenderness. No adnexal masses or tenderness. Ovaries are non-palpable. (Male: both testes palpable, no masses or lesions, no hernia, no uretheral discharge. ) (Rectal as appropriate: no evidence of hemorrhoids, fissures, bleeding or masses—Males: prostrate is smooth, non-tender and free from nodules, is of normal size, sphincter tone is firm). |
||
| Musculoskeletal
Full ROM seen in all 4 extremities as patient moved about the exam room. |
||
| Neurological
Speech clear. Good tone. Posture erect. Balance stable; gait normal. |
||
| Psychiatric
Alert and oriented. Dressed in clean slacks, shirt and coat. Maintains eye contact. Speech is soft, though clear and of normal rate and cadence; answers questions appropriately. |
||
| Lab Tests
Urinalysis – pending Urine culture – pending Wet prep – pending |
| Special Tests |
| Diagnosis |
| Differential Diagnoses
o 1- o 2- o 3- Diagnosis o |
| Plan/Therapeutics |
| o Plan:
§ Further testing § Medication § Education § Non-medication treatments |
| Evaluation of patient encounter |