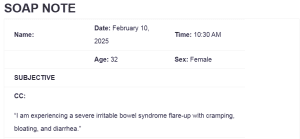
SOAP NOTE
| Name: | Date: February 10, 2025 | Time: 10:30 AM |
| Age: 32 | Sex: Female | |
| SUBJECTIVE | ||
| CC:
“I am experiencing a severe irritable bowel syndrome flare-up with cramping, bloating, and diarrhea.” |
||
| HPI:
The patient reports worsening irritable bowel syndrome (IBS) symptoms over the past three days, characterized by frequent abdominal cramping, bloating, and loose stools occurring approximately five to six times per day. Symptoms are exacerbated by stress and the consumption of dairy and high-fat foods. The patient states that the pain is diffuse but mainly localized in the lower abdomen: SOAP NOTE. The patient denies fever, vomiting, or hematochezia. Over-the-counter antispasmodics have provided minimal relief. The patient has a history of IBS, diagnosed five years ago, with periodic flare-ups triggered by diet and stress. |
||
| Medications:
· Dicyclomine 10 mg PRN for cramping · Loperamide 2 mg PRN for diarrhea · Omeprazole 20 mg daily for acid reflux |
||
| PMH
Allergies: No known drug allergies Medication Intolerances: None reported Chronic Illnesses/Major traumas: Diagnosed IBS, acid reflux Hospitalizations/Surgeries: None reported No history of diabetes, hypertension, peptic ulcer disease, asthma, lung disease, heart disease, cancer, tuberculosis, thyroid disease, or psychiatric disorders. |
||
| Family History
· Mother: Diagnosed with type 2 diabetes and IBS · Father: Hypertension, heart disease · Siblings: No known medical conditions |
||
| Social History
· College graduate, employed as an office worker · Lives alone, single, no children · No history of smoking or illicit drug use · Social alcohol consumption (1-2 drinks per week) · No recent travel or exposure to sick individuals |
||
| ROS | |
| General
No weight changes, fever, chills, or night sweats. |
Cardiovascular
No chest pain, palpitations, or edema. |
| Skin
No rashes, bruising, or lesions. |
Respiratory
No cough, wheezing, or shortness of breath. |
| Eyes
No vision changes or eye pain. |
Gastrointestinal
Abdominal cramping, bloating, diarrhea, no nausea or vomiting, no blood in stool. |
| Ears
No ear pain, ringing, or discharge noted. |
Genitourinary/Gynecological
No dysuria, urgency, or frequency.
No use of contraception, sexual activity, no STDS. |
| Nose/Mouth/Throat
No sore throat, sinus issues, or dental cavities noted. |
Musculoskeletal
No joint pain or swelling. |
| Breast
No self-reported lumps, bumps, or changes noted. |
Neurological
No headaches, weakness, or paresthesias. |
| Heme/Lymph/Endo
No known HIV status, no history of easy bruising or blood transfusions, no night sweats, no swollen glands, no excessive thirst or hunger, no cold or heat intolerance.
|
Psychiatric
Reports stress and anxiety related to symptoms. |
| OBJECTIVE | |
| Weight 72 kg BMI 25.8 | Temp 98.6°F | BP 118/72 mmHg |
| Height 167 cm | Pulse 76 bpm | Resp 16/min |
| General Appearance
The patient appears slightly fatigued but is in no acute distress. She is alert and oriented, responding appropriately to questions. She demonstrates mild discomfort when discussing her symptoms but remains cooperative throughout the exam. Her affect was slightly somber initially, improving as the encounter progressed. |
||
| Skin
Skin is warm, dry, and intact with normal turgor, indicating no signs of dehydration despite frequent diarrhea. No rashes, lesions, or bruising observed. |
||
| HEENT
· Head: Normocephalic, atraumatic. · Eyes: Pupils equal, round, and reactive to light and accommodation (PERRLA). Extraocular movements intact. No conjunctival pallor or scleral icterus, ruling out anemia or liver involvement. · Ears: External canals clear, tympanic membranes pearly gray with normal landmarks. · Nose: Nasal mucosa pink and moist; no congestion or sinus tenderness. · Throat: Oropharynx clear, no erythema or exudate. Mucous membranes are moist, with no signs of dehydration. · Neck : Supple, with full range of motion. No cervical lymphadenopathy or thyroid enlargement. |
||
| Cardiovascular
Regular rate and rhythm with S1 and S2 audible. No murmurs, rubs, or gallops. Peripheral pulses are 3+ bilaterally. Capillary refill within normal limits (less than 2 seconds). No signs of volume depletion or orthostatic hypotension despite diarrhea. |
||
| Respiratory
Breath sounds clear to auscultation bilaterally. No wheezes, rales, or rhonchi. Chest expansion is symmetrical, and there are no signs of respiratory distress. |
||
| Gastrointestinal
The abdomen is slightly distended, consistent with bloating. Bowel sounds are hyperactive in all four quadrants, consistent with diarrhea and increased motility. The abdomen is soft with mild diffuse tenderness, especially in the lower quadrants, but no rebound tenderness or guarding. No hepatosplenomegaly or palpable masses. No signs of peritoneal irritation. No costovertebral angle tenderness. |
||
| Breast
No self-reported lumps, bumps, or changes noted. |
||
| Genitourinary
Bladder non-distended; no suprapubic or flank tenderness. Pelvic examination not indicated at this time due to the absence of genitourinary complaints. |
||
| Musculoskeletal
Full range of motion in all extremities without joint pain or swelling. No signs of musculoskeletal involvement contributing to abdominal pain. |
||
| Neurological
Alert and oriented to person, place, and time. Normal speech and coordination. No focal neurological deficits noted. Reflexes are intact and symmetrical. |
||
| Psychiatric
Patient appears mildly anxious, which she attributes to the stress of managing her IBS symptoms. Maintains good eye contact, with coherent speech and logical thought processes. No signs of severe mood disorder or psychosis. |
||
| Lab Tests
· Urinalysis – Pending (to rule out urinary tract infection or dehydration) · Urine culture – Pending (if infection is suspected) · Wet prep – Pending (if gynecological causes are considered) · Stool studies (if symptoms worsen): To rule out infectious causes such as bacterial or parasitic infections. · Celiac panel (if no improvement): To assess for gluten intolerance. · Electrolytes and CBC: To evaluate for signs of dehydration, anemia, or electrolyte imbalances due to diarrhea. |
| Special Tests
No special tests ordered at this time. If symptoms persist or worsen, consider: · Lactose intolerance test · Small intestinal bacterial overgrowth (SIBO) breath test · Colonoscopy if alarm symptoms develop (e.g., unintentional weight loss, blood in stool) |
| Diagnosis |
| Differential Diagnoses
o 1- Gastroenteritis – Excluded due to the absence of fever, nausea, or vomiting, which are typical of infectious causes (Stuempfig & Seroy, 2021). Additionally, the chronic nature of the patient’s symptoms and prior IBS diagnosis suggest a functional gastrointestinal disorder rather than an acute infection. o 2- Inflammatory Bowel Disease (IBD) – Less likely due to the lack of weight loss, rectal bleeding, or persistent diarrhea with urgency. However, if symptoms persist or worsen despite treatment, further evaluation with fecal calprotectin or colonoscopy may be warranted to rule out Crohn’s disease or ulcerative colitis, as indicated by McDowell et al. (2021). o 3- Celiac Disease – Considered due to the potential for gluten intolerance mimicking IBS symptoms, including bloating and diarrhea (Posner & Haseeb, 2021). Dietary modifications may not cure symptoms; in that case, a tissue transglutaminase (tTG) IgA test and small bowel biopsy may be necessary to confirm or exclude celiac disease. Diagnosis § Irritable Bowel Syndrome (IBS) Flare-Up (ICD-10: K58.9) – The patient’s symptoms, including abdominal cramping, bloating, and frequent loose stools, are consistent with IBS (Ford et al., 2020). The absence of red flag symptoms such as weight loss, bloody stools, or nocturnal diarrhea further supports this diagnosis. |
| Plan/Therapeutics |
| Plan:
§ Further testing: If symptoms deteriorate, stool studies will be done to exclude potential infections that may mimic an IBS flare. If symptoms do not improve with dietary changes, a celiac panel will be ordered to evaluate for gluten intolerance. Also, an abdominal ultrasound can be done if abdominal pain persists or deteriorates to assess for any structural abnormalities like gallbladder disease or other gastrointestinal disorders. § Medication: The patient will also continue Dicyclomine 20 mg PRN to provide relief from abdominal cramping with flare-ups. Loperamide 2 mg PRN will be taken to control diarrhea and avoid excessive fluid loss. Omeprazole 20 mg daily will also be continued for control of acid reflux, as symptoms of GERD can, at times, be present with IBS (Ford et al., 2020). Suppose symptoms continue despite these measures. In that case, a low-dose amitriptyline (10 mg at bedtime) can be tried for pain modulation since tricyclic antidepressants decrease visceral hypersensitivity in patients with IBS. § Education: The patient was counseled on diet changes, such as taking a low-FODMAP diet and avoiding familiar culprits like dairy products, caffeine, and fatty foods that tend to worsen IBS symptoms. Hydration was stressed, and a gradual increase in fiber intake was advised to prevent exacerbating bloating and gas. Stress reduction techniques like yoga, meditation, and mindfulness were suggested since stress is an essential trigger for IBS exacerbations. § Non-medication treatments: Together with dietary and drug therapy, probiotics were also recommended to promote balance in the gut microbiota and potentially reduce symptom severity. The patient was also encouraged to engage in regular physical exercise, as exercise can enhance gut motility and reduce stress, both of which play a role in influencing the symptoms of IBS. Since stress also seems to be an exacerbating factor in the patient’s exacerbations, referral for cognitive behavioral therapy (CBT) was also broached since it is effective in treating IBS symptoms related to anxiety and stress (Chand et al., 2020). |
| Evaluation of patient encounter
The patient had a good comprehension of her illness, treatment, and the need for diet and lifestyle changes. She was willing to adhere to the prescribed diet, medication, and lifestyle changes to treat her IBS symptoms. A two-week follow-up appointment was made to evaluate her response to the treatment plan, with advice to come back earlier if her symptoms get worse or she has new issues. |
References
Chand, S. P., Kuckel, D. P., & Huecker, M. R. (2023, May 23). Cognitive behavior therapy. PubMed. https://pubmed.ncbi.nlm.nih.gov/29261869/
Ford, A. C., Sperber, A. D., Corsetti, M., & Camilleri, M. (2020). Irritable bowel syndrome. The Lancet, 396(10263). https://doi.org/10.1016/s0140-6736(20)31548-8
McDowell, C., Farooq, U., & Haseeb, M. (2021). Inflammatory bowel disease. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/29262182/
Posner, E. B., & Haseeb, M. (2021). Celiac disease. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/28722929/
Stuempfig, N. D., & Seroy, J. (2021). Viral gastroenteritis. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/30085537/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Instructions
SOAP Note
Each week you are required to enter your patient encounters into CORE. Your faculty will be checking to ensure you are seeing the right number and
mix of patients for a good learning experience. Beginning in Week 5, you will need to include one complete SOAP note each week through Week 9 for
a total of 5 complete SOAP notes for this course using this SOAP Notes template.
SOAP NOTE
The SOAP note should be related to the content covered in this week, and the completed SOAP note should be submitted to the Submissions Area. When submitting your note, be sure to include the reference number from CORE where you entered this specific patient‘s case entry.
A SOAP Note guide is available here.
- SOAP note for irritable bowel syndrome flair up