Peer Responses – Therapeutic Communication and Psychiatric Assessment
Responding to Peer 1
Thank you for your post. I agree with you that the practitioner demonstrated therapeutic communication skills when interviewing the client and that there is a missing link in rapport establishment within the conversation. Good rapport fosters closer and harmonious relationships between caregivers and their clients (Butt, 2021). It was thus crucial that the client establish a good rapport with the client. Psychiatric assessment lets caregivers gather insight into apparent emotional, behavioral, and developmental factors compromising health and wellness. As captured in your post, the Child Behavior Checklist (CBCL) and the Strengths and Difficulties Questionnaire (SDQ) are symptom-rating scales commonly used in psychiatric evaluation for children and adolescents. Children’s Depression Rating Scale (CDRS) and the Children’s Depression Inventory (CDI) are other commonly used symptom rating scales in psychiatric evaluation. As suggested by Srinath et al. (2019), these tools can be used effectively to assess the severity of depression. They can also monitor clients’ responses to therapy.
References
Butt, M. F. (2021). Approaches to building rapport with patients. Clinical Medicine, 21(6). https://doi.org/10.7861/clinmed.2021-0264
Sharma, E., Srinath, S., Jacob, P., & Gautam, A. (2019). Clinical practice guidelines for assessment of children and adolescents. Indian Journal of Psychiatry, 61(8), 158. https://doi.org/10.4103/psychiatry.indianjpsychiatry_580_18
Responding to Peer 2
This is a great post. I agree that the practitioner navigated the interview excellently by carefully probing the client and allowing him to answer the questions. Your post is, however, unclear on why the irritability should be explored further. I agree with your take on suicidality. It is often suggestive of severe disease and should thus be addressed. I also agree with your post on psychiatric screening tools and the available child/adolescent-specific therapies. Youth Anxiety Measure and CDRS-R are some of the widely used symptom screening tools. The Children’s Depression Inventory (CDI) and Child Behavior Checklist (CBCL) are other tools that can be used in psychiatric assessment (Mangione et al., 2022). As captured in your post, play therapy and Parent-Child Interaction Therapy (PCIT) are some of the child-specific psychotherapies that are utilizable in managing the child in the case. As supported by Saito et al. (2020), dialectical behavioral therapy is another effective psychotherapy for the child case presented.
References
Mangione, C. M., Barry, M. J., Nicholson, W. K., Cabana, M., Chelmow, D., Coker, T. R., Davidson, K. W., Davis, E. M., Donahue, K. E., Jaén, C. R., Kubik, M., Li, L., Ogedegbe, G., Pbert, L., Ruiz, J. M., Silverstein, M., Stevermer, J., & Wong, J. B. (2022). Screening for depression and suicide risk in children and adolescents. JAMA, 328(15), 1534. https://doi.org/10.1001/jama.2022.16946
Saito, E., Tebbett-Mock, A. A., & McGee, M. (2020). Dialectical behavior therapy decreases depressive symptoms among adolescents in an acute-care inpatient unit. Journal of Child and Adolescent Psychopharmacology, 30(4), 244–249. https://doi.org/10.1089/cap.2019.0149
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Based on the YMH Boston Vignette 5 video, post answers to the following questions:
- What did the practitioner do well? In what areas can the practitioner improve?
- At this point in the clinical interview, do you have any compelling concerns? If so, what are they?
- What would be your next question, and why?
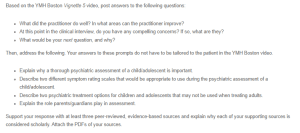
Therapeutic Communication and Psychiatric Assessment
Then, address the following. Your answers to these prompts do not have to be tailored to the patient in the YMH Boston video.
- Explain why a thorough psychiatric assessment of a child/adolescent is important.
- Describe two different symptom rating scales that would be appropriate to use during the psychiatric assessment of a child/adolescent.
- Describe two psychiatric treatment options for children and adolescents that may not be used when treating adults.
- Explain the role parents/guardians play in assessment.
Support your response with at least three peer-reviewed, evidence-based sources and explain why each of your supporting sources is considered scholarly. Attach the PDFs of your sources.
Video
- YMH Boston. (2013, May 22). Vignette 5 – Assessing for depression in a mental health appointmentLinks to an external site. [Video]. YouTube. https://www.youtube.com/watch?v=Gm3FLGxb2ZU.