Patient Logs
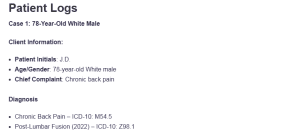
Case 1: 78-Year-Old White Male
Client Information:
- Patient Initials: J.D.
- Age/Gender: 78-year-old White male
- Chief Complaint: Chronic back pain
Diagnosis
- Chronic Back Pain – ICD-10: M54.5
- Post-Lumbar Fusion (2022) – ICD-10: Z98.1
Procedure:
- Review of medical history, including lumbar fusion in 2022
- Physical exam to assess back mobility and pain levels
- No additional procedures during this visit: Patient Logs
Treatment Plan and Notes:
J.D. is a 78-year-old male presenting for follow-up care of chronic back pain, which has been ongoing since 1965 and has worsened post-lumbar fusion in 2022. He complains of continuous and daily limping pain (3/10), and it is worsened by standing and walking. No additional treatments were started during this visit, and pain management consists of gabapentin, Tylenol, and ibuprofen. J.D. walks with a walker and a cane, suggesting that he has a severe functional impairment.
The plan of treatment will be continuing with the present pain management, and the concentration will be on mobility help in the treatment, along with regular follow-ups. Since he is of advanced age, the treatment objective is to ensure he has a quality life and there is no further deterioration in his mobility.
Case 2: 52-Year-Old Black Female
Client Information:
- Patient Initials: K.M.
- Age/Gender: 52-year-old Black female
- Chief Complaint: Sciatica flare-ups and a lump behind the knee
Diagnosis:
- Sciatica – ICD-10: M54.3
- Emphysema – ICD-10: J43.9
- Prediabetes – ICD-10: R73.03
- Asthma – ICD-10: J45.909
- Lipomas – ICD-10: D17.9
Procedure:
- An MRI was ordered to investigate the lump behind the right knee
- Routine physical examination
Treatment Plan and Notes:
K.M. presents with daily sciatica flare-ups and a history of emphysema, asthma, and prediabetes. She also reports a new lump behind her knee, which has prompted an MRI for further evaluation. The patient is treating her sciatica by resting and taking ibuprofen. The management schedule entails controlling the pain using anti-inflammatories and observing the lump based on the MRI report.
An appointment will be made following the checkup results of the MRI to determine the next course of action. Also, her chronic diseases, such as emphysema and asthma, should be monitored closely, and pulmonary testing should be done regularly to improve the situation.
Case 3: 84-Year-Old White Male
Client Information:
- Patient Initials: G.T.
- Age/Gender: 84-year-old White male
- Chief Complaint: Shortness of breath and chest pain
Diagnosis:
- COPD – ICD-10: J44.9
- Lumbar Strain – ICD-10: M54.5
- Chest Pain (Unspecified) – ICD-10: R07.9
Procedure:
- Review of COPD management and current medications
- Monitoring of chest pain episodes with nitroglycerin
- Routine physical examination
- Follow-up with the pulmonologist
Treatment Plan and Notes:
G.T. is a long-term patient with COPD who is placed on continuous oxygen now and complains of back pain daily. His chest pain, which is relieved with nitroglycerin, raises concerns as to the possible cardiac involvement. Treatment plans entail additional oxygen supplementation and medicine against back pain, including referral to a cardiology unit, where chest pain will be investigated.
It is also suggested that the patient limit the physical exercises and stressors that may contribute to the development of symptoms of respiratory and cardiac conditions. Any suggestion of COPD exacerbation (especially worsened or more dyspnea and wheezing) is to be checked regularly, and the patient is to be educated on being warned about increased difficulties with the heart or lungs.
Case 4: 78-Year-Old White Male
Client Information:
- Patient Initials: H.W.
- Age/Gender: 78-year-old White male
- Chief Complaint: Shortness of breath, productive cough, and nasal congestion
Diagnosis:
- Pleural Effusion – ICD-10: J90
- Chronic Sinusitis – ICD-10: J32.9
Procedure:
- Physical examination
- Review of past sinus surgeries (2023)
- Monitoring of respiratory status
Treatment Plan and Notes:
H.W. presents with ongoing shortness of breath, productive cough, and nasal congestion, which are likely linked to pleural effusion and chronic sinusitis. The patient is on Flonase and a saline nasal spray. The management course involves the maintenance of respiration, including Nasal saline irrigation and Flonase.
Pulmonology follow-up is also performed to monitor pleural fluid levels, and a smoking cessation regimen should also be advised to minimize further respiratory complications (Krishna & Rudrappa, 2024). The patient should be educated regarding potential alarming signs of worsening respiratory condition, that is, dyspnea and change in the production of sputum, and instructed to contact the issues as soon as they occur.
Case 5: 27-Year-Old Black Male
Client Information:
- Patient Initials: D.P.
- Age/Gender: 27-year-old Black male
- Chief Complaint: Carpal tunnel syndrome and wrist pain
Diagnosis:
- Carpal Tunnel Syndrome (Right Wrist) – ICD-10: G56.00
- Carpal Tunnel Syndrome (Left Wrist) – ICD-10: G56.01
Procedure:
- Physical exam of both wrists
- Prescription for wrist splints
- Plan for follow-up in 2-3 weeks
Treatment Plan and Notes:
D.P. has carpal tunnel syndrome in both hands, which is worsened by excessive use of computers. The patient has been recommended to take some ibuprofen to ease pain and wear a wrist splint at night and during rest. In 2-3 weeks, a progress review will be conducted. The patient will also be encouraged to take a break when working to avoid any additional strain on his wrists and the use of heavy loads.
Physical therapy can be an option when symptoms do not resolve or become worse. As part of the treatment plan, ergonomic changes to his workstation will be implemented so as to minimize the wrist strain and any additional injury.
Case 6: 58-Year-Old White Male
Client Information:
- Patient Initials: M.F.
- Age/Gender: 58-year-old White male
- Chief Complaint: Follow-up after left kidney removal due to cancer
Diagnosis:
- Post-Kidney Cancer (Left Kidney Removal) – ICD-10: C64.9
Procedure:
- Physical examination
- Routine follow-up to monitor for recurrence
Treatment Plan and Notes:
M.F. is in remission following the removal of his left kidney due to cancer. He denies any pain or urinary symptoms, and he is under follow-up regarding the possibility of recurrence. The treatment plan entails follow-up care, which involves lab work and imaging. The patient is advised to maintain periodic screening to identify any future likelihood of cancer and uphold healthy living to promote overall health. The patient is also advised to take preventive health measures like a balanced diet and regular exercise so as to sustain the functioning of the kidney and healthy living.
Case 7: 20-Year-Old White Male
Client Information:
- Patient Initials: S.B.
- Age/Gender: 20-year-old White male
- Chief Complaint: Radiculopathy from a bulging disc
Diagnosis:
- Lumbar Radiculopathy – ICD-10: M54.16
Procedure:
- Epidural steroid injection in August 2024
- Follow-up physical therapy
Treatment Plan and Notes:
S.B. reports radiculopathy symptoms following a bulging disc in his lumbar region. He already had an epidural steroid injection and is now going through physical therapy. Sitting inflicts more pain on him. The management process will involve the continuation of physical therapy and medications such as nabumetone or Robaxin, which represses pain (Alexander & Varacallo, 2024).
His reaction to treatment will be monitored regularly, and the plan will be adjusted accordingly. Simple tasks such as bending, dashing, and heaving that can tax the back of the patient should also be discouraged, and the patient is encouraged to ensure his body posture in his daily routines is good.
Case 8: 45-Year-Old White Male
Client Information:
- Patient Initials: L.W.
- Age/Gender: 45-year-old White male
- Chief Complaint: Cervical strain and tension headaches
Diagnosis:
- Cervical Strain – ICD-10: M54.2
- Degenerative Disc Disease – ICD-10: M50.30 (Donnally III et al., 2023).
Procedure:
- MRI of cervical spine
- Follow-up physical therapy
Treatment Plan and Notes:
L.W. is managing cervical strain due to tension headaches, with MRI results showing degenerative disc changes. The patient has episodic neck pain that occurs periodically, particularly when he looks up. Treatment involves physical therapy and application of stretching activities to ensure that muscle tension is reduced.
A second follow-up visit will then be scheduled to follow up on his progress and to discuss any new developing symptoms. The patient should also learn to shun neck-straining activities and learn to work using better ergonomics.
Case 9: 78-Year-Old White Male
Client Information:
- Patient Initials: R.F.
- Age/Gender: 78-year-old White male
- Chief Complaint: Prostate cancer follow-up
Diagnosis:
- Prostate Cancer – ICD-10: C61 (Rosario & Rosario, 2020)
- Erectile Dysfunction – ICD-10: N52.9
Procedure:
- Radiation therapy completed (5 weeks)
- Hormone therapy injections
Treatment Plan and Notes:
R.F. has undergone radiation therapy for prostate cancer and is currently receiving hormone therapy injections. He continues to experience erectile dysfunction and frequent nighttime urination. The management involves follow-up treatment with drugs such as Tamsulosin and Proscar.
Follow-up care with oncology is planned to track the possibility of the recurrence of the cancer, and additional treatment can be further changed depending on how he reacts to the ongoing medicines. The patient must also be advised on how to deal with the side effects of his treatment and how to deal with urinary and sexual dysfunction.
References
Alexander, C. E., & Varacallo, M. (2024, February 27). Lumbosacral radiculopathy. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430837/
Donnally III, C. J., Hanna, A., & Varacallo, M. (2023). Lumbar degenerative disk disease. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448134/
Krishna, R., & Rudrappa, M. (2024). Pleural effusion. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448189/
Rosario, E., & Rosario, D. J. (2020). Localized prostate cancer. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK563248/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Patient Log
Throughout this course, you will also keep a log of patient encounters using Meditrek. AGPCNP students must record at least 100 encounters with GYN patients; FNP students must record at least 125 encounters with patients (100 GYN and 25 OB patients) by the end of this practicum.
The patient log must include the following:
- Client Information
- Diagnosis
- Procedure (Note: Make sure that, as you perform procedures at your practicum site, you also note those on your printed-out Clinical Skills List.)
- Treatment Plan and Notes
Please see attached.
78 white male
- Back pain since 1965
- Lumbar fusion in 2022
- 3/10 daily achy pain
- Takes gabapentin, Tylenol, ibuprofen
- Increased with standing and walking
- Use walker cane and wheelchair
- Can’t do sports or golf
52 black female
- Sciatica flare daily
- Hx of emphysema
- Prediabetic
- Asthma
- Multiple lipomas
- Lump behind right knee
- Ordered MRI
- Manages pain with rest and Ibuprofen
84 years old white male
- COPD 1990, lumbar strain
- Continuous oxygen therapy, 2-3 liters
- Follow by Pulmonolgist
- Former smoker 1980
- Denies surgery, procedure
- physical therapy
- Daily back pain, average 3-4/10, flare up 6-7/10 lasting 1-2 hrs after oxygen.
- Pain aggravate by prolong sitting, standing, walking
- Chest pain at the time of the visit, took 2 nitroglycerin with relief, refused to go to ER.
78 years old white male
- Pleural effusion 2023, Sinusitis 2000
- Had chest tube placed x3 in the past
- SOB with rest and activity, Smoker 4-6 cigarettes per day, also wear nicotine patch
- Productive cough, slightly congested, nasal crust
- Service 1980-1993
- Follow by Pulmonologist
- Frequent sinus infection, had 2 sinus surgery june 2023 and May 2025; nasal turbinates reduction
- Currently using flonase, normal saline
27 years old black male
- Carpal tunnel right wrist, wear splint
- Pain developed on left wrist 1-2 weeks
- Denies surgery or procedure
- On computer most of the day related to work
- Painful when twisting wrist, rated pain 6/10
- Voiced mild tingling, denies numbness
- Unable to lift heavy thing related to pain
- Daily weight lifting at gym
- Denies fever, SOB, chest pain, chills, palpitation
- Clear lung sound or heart sound
- Last physical visit 2022, due for physical
- Take OTC Tylenol
- Today plan: ibuprofen 600mg po TID, wear wrist splint at night and off morning, stress ball, follow up 2-3 weeks, restriction of heavy weight lift
Patient Logs
58 white male
- Had left kidney removed due to cancer
- 5 abdominal scars measuring 2 cm, 2.5 cm, 2 cm, 8 cm, 1 cm
- Denies UTI
- No pain at this time.
20 years old white male
- Radiculopathy 2023 from buddying disc of the lumbar
- Denies numbness/tingling
- Constant Shooting pain 6-7/10 on average
- Denies using assistance device
- Epidermal done on lumbar August 2024, denies surgery
- Pain aggravates by prolong sitting
- PT and chiropractor
- nabumetone 500mg po BID
- Robaxin PRN
- No longer able to skiing and fishing
45 years old white male
- Cervical strain november 2024
- Started from tension headache, MRI shows degenerative disc on the neck
- Daily neck pain 1/10 on averages, when flare up go up to 3/10 lasting 2-4 hours, manages with rest and stretching
- Aggravate by looking upward
- Denies numbness/tingling
- Denies any surgery or procedure
- Denies loss of bladder/bowel control
- occupation : IT tech
- Denies taking any prescriptions or OTC, do not like to take meds
78 years old white male
- Prostate cancer 2022, erectile dysfunction, kidney stone
- 5 weeks of 5 days per week of radiation
- 57 seeds into the prostate – 3 injections of hormone x 7-8 weeks
- Last oncology visit June 2025
- Denies surgery or procedure
- Tamsolosin 0.4mg po daily
- Proscar
- Wear brief at night, changes 2-4 times per night
- Voided >5 times per night, weak stream.
- CBC, urinalysis, PSA ordered today
39 years old white male
- TBI from MVA
- Homeless, alert and oriented
- PHM, PTSD, Anxiety, Depression, Chronic adjustment disorder, ADHD
- Impacted short and long term memory
- Projective, intrusive thought, curse alot, insomnia, irritability, lack of motivation, frequent tinnitus, Headache, blurry vision, hypersensitivity to light and sound
- Follow by psychologist
- Occupation: used to be Paramedic, unemployment
47 years old white male
- Prostate cancer summer 2024
- Last urology visit 1/2025
- Had 5 radiation sessions
- Denies surgery or procedure
- Denies leakage, urgency or frequency, erectile dysfunction, UTI
- Occupation, still working, own business
- Tamsulosin 0.4mg po daily
46 black male
- Follow up on 6.2 A1c last year, imaging by urology -hydrocele left greater than right, right shoulder pain x-ray negative
- Smoker, recently incarcerated
- Requested refill on vitamin D, increase on cialis
- C/0 periodic “wet spot” on back with mild pain on “skin bump”
- C/o sore throat (right side) x 2 weeks, increased cough, SOB on exertion
- LCTA, non-labored
- HRR, S1S2 no murmur, click, rub
- Bowel sounds normo-active in all quadrants
- TMs pearly gray with landmarks
- Bilateral nasal mucosa erythemetous/edemetous no discharge
- Oral mucosa pink moist
- Right tonsil +2
- left tonsil +1
- Right tonsillar lymph node tender to palpation no enlargement
- Left superior anterior cervical node firm/nontender
- B/P 140/90
- RECHECK 138/88
- Refer to derm for back
- Refer to ENT for throat
- Refer to urology for hydrocele TX
- Order MRI and PT right shoulder
- Refill vitamin D
- No increase on cialis r/t hypertension
- Recommend smoking cessation
- Prescribe nicotine patch
51 black female
- Follow up after workplace accidental needle stick that drew blood
- HIV non-reactive
- Hepatic B immune
- Housekeeper in Healthcare facility was wiping a bed and felt a needle penetrate her gloved finger. She pulled the butterfly needle out of her finger and it began to bleed. She went to the ED and had blood tests done.
- Her anxiety is peaked, causing neck pain, headaches, heart racing.
- Return in 6 months for repeat blood labs. Seek mental help as necessary.
32 white male
- Bilateral knee pain. Right knee hyperextended in 2024
- MRI shows partial tears that healed
- Left knee pain due to compensation for right
- Daily 5/10 sharp, shooting, pain with tightness and instability worsens with increased walking and sitting. Flares 3/7 days to 7/10. Relieved with ibuprofen and rest
- Right- handed
- Right wrist pain post carpal tunnel surgery 2025
- Daily constant 4/10 pain on waking for 10 minutes or when pushing a button hard
- EMG 2024 prior to surgery
77 years old white male
- Prostate cancer 9/2009
- Follow by urology once yearly
- Denies issues with urination, leakage, kidney infection
- Denies radiation treatment
- Currently doing watchful waiting at this time
- Denies SI & Homeless
- Refused PSA lab and urine sample
75 years old white male
- Cervical strain 1980, from day to day activity
- Denies injuries, surgery, procedure
- Denies PT, Chiropractor
- No MRI or X-ray done
- Daily neck pain average 7/10, flare up to 10/10 as someone climbing on his neck and squishing it. Fare up 2-3 days/wk last 24 hours a day, pain aggravate by looking upward
- Numbness/tingling moderate intermittently on both upper extremities
- Use cane occasionally
- Low back pain 1969, from degenerated disc disorder
- 4 spinal ablation done in the past, last one done 12/2024, help with pain
- Denies surgery of the back
- Daily back pain, average 7/10, flare up daily 10/10 last 24 hours
- Pain aggravate by prolong standing, walking, bending over
- Denies issue bowel/bladder control
- Moderate intermittent numbness/tingling lower extremities
- Take Tylenol for pain
- Impacted day to day activity, limited mobility, no longer hunting, fishing, or camping.