Patient Logs
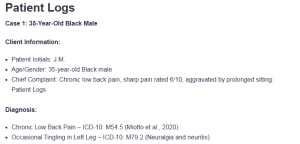
Case 1: 35-Year-Old Black Male
Client Information:
- Patient Initials: J.M.
- Age/Gender: 35-year-old Black male
- Chief Complaint: Chronic low back pain, sharp pain rated 6/10, aggravated by prolonged sitting: Patient Logs
Diagnosis:
- Chronic Low Back Pain – ICD-10: M54.5 (Miotto et al., 2020)
- Occasional Tingling in Left Leg – ICD-10: M79.2 (Neuralgia and neuritis)
Procedure:
- Comprehensive musculoskeletal history and physical exam
- Evaluation of pain severity and functional limitations
- Physical therapy follow-up assessment
- Pain management review and medication history (Ibuprofen)
Treatment Plan and Notes:
J.M. is a 35-year-old Black male with chronic low back pain, rated 6/10, worsened by prolonged sitting. He experiences occasional tingling in his left leg, relieved by standing. He had no prior surgeries or procedures, but he completed physical therapy from 2012-2019. Currently, he uses Ibuprofen for pain relief.
The management plan includes continuing Ibuprofen, re-engaging in physical therapy, and implementing ergonomic adjustments at work. Follow-ups will assess progress, and non-pharmacologic strategies, like posture correction and stretching, will be emphasized.
Case 2: 73-Year-Old White Male
Client Information:
- Patient Initials: R.L.
- Age/Gender: 73-year-old White male
- Chief Complaint: Follow-up visit for non-Hodgkin lymphoma
Diagnosis:
- Non-Hodgkin Lymphoma – ICD-10: C85.9
- Occasional Sweating upon Waking – ICD-10: R61 (Excessive sweating)
Procedure:
- Comprehensive medical history review
- CBC (Complete Blood Count) during the visit
- Physical exam to check for signs of lymphoma progression
- Follow-up with hematologist
Treatment Plan and Notes:
R.L. is a 73-year-old White male presenting for a routine follow-up regarding his non-Hodgkin lymphoma, diagnosed in 2025. He reports occasional sweating upon waking but denies new symptoms like weight loss, pain, or enlarged lymph nodes. His recent CBC was performed during the visit. He follows up with a hematologist annually, with no medication changes.
The management plan includes continuing annual follow-ups, monitoring for lymphoma recurrence, educating on symptom awareness, and providing lifestyle advice for maintaining a healthy immune system (Jamil & Mukkamalla, 2023).
Case 3: 51-Year-Old Black Male
Client Information:
- Patient Initials: M.W.
- Age/Gender: 51-year-old Black male
- Chief Complaint: Follow-up visit for meniscus tear (right knee)
Diagnosis:
- Meniscus Tear (Right Knee) – ICD-10: S83.241A
- Chronic Knee Pain – ICD-10: M25.561
Procedure:
- Comprehensive musculoskeletal exam
- X-ray review (January 2025)
- Orthopedic referral for further evaluation
- Pain severity assessment
Treatment Plan and Notes:
M.W. is a 51-year-old Black male presenting for a follow-up regarding his right knee meniscus tear. He reports ongoing knee pain and difficulty reaching his orthopedic referral. He denies new injuries, but the pain has been persistent since the injury, affecting his daily activities. An X-ray was performed in January 2025, but he has not seen the orthopedic specialist yet.
The treatment plan includes scheduling his orthopedic appointment, continuing pain management with over-the-counter medications, and referring him to physical therapy (El-Tallawy et al., 2021). Regular follow-ups will monitor progress and adjust the treatment plan if needed.
Case 4: 35-Year-Old White Male
Client Information:
- Patient Initials: J.D.
- Age/Gender: 35-year-old White male
- Chief Complaint: Chronic low back pain
Diagnosis:
- Chronic Low Back Pain – ICD-10: M54.5
- Inguinal Hernia (Past Surgery) – ICD-10: K40.90
- Musculoskeletal Pain – ICD-10: M79.1
Procedure:
- Comprehensive musculoskeletal exam
- X-ray of the lower back
- Physical therapy follow-up
- Pain severity rating and movement assessment
Treatment Plan and Notes:
J.D. is a 35-year-old White male complaining of chronic lower back pain that gets exacerbated whenever he bends, sits, or stands. He has a history of surgery for an inguinal hernia and has sharp pain (4-5/10), which increases up to 10/10 during flare-ups. He occasionally experiences numbness and tingling as well.
The treatment plan shall involve the following: continuing with physical therapy, including strengthening and mobility exercises, taking Ibuprofen to manage pain, and taking into account flare-ups with the help of back support braces. Emphasis will be placed on daily stretching exercises and posture improvement with subsequent checkups.
Case 5: 50-Year-Old White Male
Client Information:
- Patient Initials: T.P.
- Age/Gender: 50-year-old White male
- Chief Complaint: Ongoing abdominal pain, diarrhea
Diagnosis:
- Irritable Bowel Syndrome (IBS) – ICD-10: K58.9
- Gastroesophageal Reflux Disease (GERD) – ICD-10: K21.9
- Right Ankle Pain – ICD-10: M25.561
Procedure:
- Comprehensive abdominal exam and GI history review
- Lab work, including CT scan, colonoscopy, and barium swallow study
- Evaluation of current medications and treatment adherence
- Abdominal palpation and bowel habit evaluation
Treatment Plan and Notes:
T.P. is a 50-year-old White male who has a history of IBS and who presents with abdominal pain and diarrhea (up to 15-20 times daily). He controls IBS using Imodium, and he denies the presence of blood in his bowel movement. He has also had CT and colonoscopy scans and barium swallow test studies but without any conclusive results. He also experiences GERD and pain in the right ankle.
The treatment plan consists of looking after the IBS management, changes in the diet, and Imodium use when necessary. Further monitoring by a GI specialist is scheduled, and GERD lifestyle changes will be advised. Ankle pain physical therapy can be considered.
Case 6: 63-Year-Old Male
Client Information:
- Patient Initials: L.K.
- Age/Gender: 63-year-old Male
- Chief Complaint: Follow-up for stroke and memory issues
Diagnosis:
- Stroke (History of) – ICD-10: I63.9
- Cerebrovascular Disease (CVD) – ICD-10: I67.9
- Depression – ICD-10: F32.9
- Right Side Weakness – ICD-10: M62.81
Procedure:
- Neurological history and physical exam
- Medication review for stroke management and depression
- Follow-up with physical therapy, speech therapy, and occupational therapy
- Evaluation of depression symptoms and medication adherence
Treatment Plan and Notes:
L.K. is a 63-year-old male previously diagnosed with a stroke (2018), which weakened his right side and impaired his memory. He follows up with a neurologist and uses aspirin, atorvastatin, baclofen, and Flexeril on an as-needed basis. He complains of low spirits and a sense of inadequacy concerning his recovery.
The treatment plan involves follow-up with a neurologist, keeping him on the same medications, and addressing depression through therapy and changes in medication. Recovery will be enabled by physical, speech, occupational therapy, and social support to cope with the depression.
Case 7: 45-Year-Old Male
Client Information:
- Patient Initials: D.H.
- Age/Gender: 45-year-old Male
- Chief Complaint: Hypertension follow-up and routine physical
Diagnosis:
- Hypertension – ICD-10: I10
- Hyperlipidemia – ICD-10: E78.5
- Alcohol Use – ICD-10: F10.10
- Cigarette Smoking – ICD-10: Z72.0
Procedure:
- Blood pressure (BP) monitoring and evaluation
- Lab orders for CMP, CBC, UA, TSH
- Physical exam and assessment for cardiovascular risk factors
- Discussion of alcohol and tobacco use
Treatment Plan and Notes:
D.H. is a 45-year-old man who presents for a routine physical examination. His blood pressure is high (168/92 mmHg), and he has hypertension (he is taking medications Losartan and Amlodipine) (Purnell, 2023). He consumes 8-10 units of hard liquor per week and smokes cigars at times. He is not on BP medication at this moment because he is not adhering to it, but he agrees to take it up once again.
The treatment plan involves enlarging his dose of Amlodipine to 10 mg, 2 2-week blood pressure checkup, and a change in his lifestyle, including alcohol and smoking. Referral to a cardiologist may be necessary, and tests will be done in the lab to measure cholesterol and thyroid.
Case 8: 60-Year-Old Black Male
Client Information:
- Patient Initials: R.P.
- Age/Gender: 60-year-old Black male
- Chief Complaint: Follow-up for traumatic brain injury (TBI) and memory issues
Diagnosis:
- Traumatic Brain Injury (TBI) – ICD-10: S06.9X0A
- Depression – ICD-10: F32.9
- Anxiety – ICD-10: F41.9
- Memory Impairment – ICD-10: R41.3
Procedure:
- Neurological exam to assess cognitive function
- Psychological assessment to evaluate depression and anxiety symptoms
- Follow-up with neurologist for TBI management
- Cognitive testing to assess memory loss
Treatment Plan and Notes:
R.P. is a 60-year-old Black male with a history of TBI, which occurred as a result of an automobile accident that took place in 2018. He has complained of chronic memory loss, poor memory of names, and some headaches, and his light and sound sensitivity is on the rise. In addition, he has a history of depression and anxiety, and this may be worsened by his TBI.
The treatment plan implies the follow-up of a neurologist, antidepressants and anti-anxiety drugs (such as SSRIs), and cognitive therapy. To acquire emotional well-being and coping, R.P. will be sent to counseling. Regular follow-ups will be scheduled to monitor the patient’s cognitive function and adjust treatment as necessary.
Case 9: 78-Year-Old Black Female
Client Information:
- Patient Initials: A.W.
- Age/Gender: 78-year-old Black female
- Chief Complaint: Follow-up for stage 3 chronic kidney disease (CKD), hypertension, and pre-diabetes
Diagnosis:
- Stage 3 chronic kidney disease (CKD) – ICD-10: N18.3
- Hypertension – ICD-10: I10
- Prediabetes – ICD-10: R73.03
- Anemia – ICD-10: D64.9
Procedure:
- Kidney function assessment (eGFR, creatinine)
- Blood pressure (BP) monitoring
- Comprehensive lab work (CMP, CBC, A1c)
- Nephrology referral for CKD management
Treatment Plan and Notes:
A.W. is a 78-year-old Black woman who has stage 3 CKD, hypertension, and pre-diabetes. Her recent laboratory test findings indicate an eGFR of 47, creatinine of 1.18, and an A1c of 5.8. She is enrolled in Metformin, Metoprolol, Atenolol, and Losartan. Moderate anemia is also present in A.W., as shown by low hemoglobin levels and a certain fatigue.
The course of treatment will consist of further control over hypertension with existing drugs, monitoring of kidney activity, and the referral to a nephrologist regarding its specialized treatment of CKD (Cheung et al., 2021). She will be taught lifestyle changes, such as diet and exercise. A 3-6 month follow-up is planned.
Case 10: 55-Year-Old White Male
Client Information:
- Patient Initials: S.G.
- Age/Gender: 55-year-old White male
- Chief Complaint: Scars on legs due to burn injuries and fatigue
Diagnosis:
- Scar Tissue from Burn Injury – ICD-10: T22.201A
- Chronic Fatigue – ICD-10: R53.82
- Skin Infection (Recurrent) – ICD-10: L08.9
Procedure:
- Comprehensive dermatological exam to assess scars
- Review of medical history and burn injuries
- Evaluation of fatigue and its impact on daily functioning
- Discussion of current treatments for scar management
Treatment Plan and Notes:
S.G. is a 55-year-old White male patient who obtained serious burn wounds in 1993 and got permanent scars on his legs. He keeps on getting skin infections and feeling fatigued owing to internal itching of the scars, which makes him uncomfortable and unable to sleep. These issues cost him 2-3 days of work each year.
The management protocol entails the treatment of scars through topical creams to minimize itching and the occurrence of infections. Referral to a dermatologist to give further care might be necessary. Explanation on wound care, stress management, and sleep hygiene will also be imparted to S.G. There will be follow-ups to determine his condition and fatigue.
Case 11: 67-Year-Old Black Female
Client Information:
- Patient Initials: M.S.
- Age/Gender: 67-year-old Black female
- Chief Complaint: Annual physical checkup and concerns regarding diabetes and hypertension
Diagnosis:
- Diabetes Mellitus Type 2 – ICD-10: E11.9 (Lara-Esqueda et al., 2021)
- Hypertension – ICD-10: I10
- Glaucoma – ICD-10: H40.9
- Insect Bites (Recent) – ICD-10: T77.2
- Vitamin D Deficiency – ICD-10: E55.9
Procedure:
- Comprehensive physical exam
- Eye exam to assess for glaucoma
- Blood pressure monitoring
- Laboratory tests (CBC, CMP, A1c, Vitamin D levels)
- Skin exam for insect bites and other dermatological concerns
Treatment Plan and Notes:
M.S. is a 67-year-old Black female who comes in to have her annual physical examination. She has type 2 diabetes, which is well under control through diets, and hypertension, which is controlled by the use of Nifedipine. Earlier, she developed glaucoma, and she mentioned some insect bites on her back and arm.
She has been taking OTC vitamin supplements for more than two years since the last eye checkup, and she has been taking them since she has a vitamin D deficiency.
The care plan is comprised of her diabetes and hypertension management continuity, referral to an ocular retest, and vitamin D supplements. The insect bites will be treated by prescription of topical hydrocortisone, and the management of diabetes, blood pressure, and glaucoma will be followed up.
Case 12: 60-Year-Old Latino Male
Client Information:
- Patient Initials: C.P.
- Age/Gender: 60-year-old Latino male
- Chief Complaint: Follow-up for multiple myeloma, fatigue, and joint pain
Diagnosis:
- Multiple Myeloma (4-year remission) – ICD-10: C90.00
- Joint Pain – ICD-10: M25.50
- Fatigue – ICD-10: R53.83
- Immunocompromised State – ICD-10: D84.9
Procedure:
- Review of multiple myeloma treatment and current remission status
- Comprehensive physical exam
- Pain assessment and evaluation of joint pain severity
- Blood work to assess for anemia, kidney function, and overall health status
- Follow-up for ongoing chemotherapy and immunosuppressive medications
Treatment Plan and Notes:
C.P. is a 60-year-old Latino Male diagnosed with Multiple Myeloma in 2019 and has been in remission since 2023 after successfully completing chemotherapy. He is on daily chemotherapy pills and has some body aches, joint pain, fatigue, and brain fog. Due to the immunocompromised condition, special attention is paid to the development of infections and other complications.
The treatment plan involves the administration of chemotherapy, alleviation of joint pain using over-the-counter drugs, and referral to physical therapy. C.P. will also be observed in cases of infections, and fatigue management will also be facilitated. He would be scheduled to attend a follow-up appointment to determine his progress.
Case 13: 38-Year-Old Asian Male
Client Information:
- Patient Initials: J.L.
- Age/Gender: 38-year-old Asian male
- Chief Complaint: Chronic back pain, knee pain, and PTSD
Diagnosis:
- Chronic Low Back Pain – ICD-10: M54.5
- Left Knee Meniscus Tear (Partial) – ICD-10: S83.242A
- Right Ankle Sprain – ICD-10: S93.401A
- Post-traumatic stress disorder (PTSD) – ICD-10: F43.10
Procedure:
- Musculoskeletal exam
- Review of imaging
- Pain severity assessment
- PTSD follow-up
Treatment Plan and Notes:
J.L. is a 38-year-old male experiencing chronic back pain, a left knee meniscus tear, and a right ankle sprain. The pain rating is at 4/10 and escalates to 9/10 when the patient spends too much time walking or sitting. He also experiences being numb in the feet.
The pain management is surgically treated using Tylenol and hot/cold therapy in its treatment plan. Back and knee strengthening physical therapy is suggested. Counseling will be used to deal with PTSD. The follow-up will also recheck pain and mental health.
Case 14: 77-Year-Old White Male
Client Information:
- Patient Initials: P.H.
- Age/Gender: 77-year-old White male
- Chief Complaint: Diabetes, hypertension, and diabetic neuropathy
Diagnosis:
- Diabetes Mellitus Type 2 – ICD-10: E11.9
- Hypertension – ICD-10: I10
- Diabetic Neuropathy – ICD-10: E11.40
Procedure:
- Comprehensive physical exam
- Blood pressure monitoring
- Neurological exam for neuropathy
- Lab tests, including A1c and kidney function
Treatment Plan and Notes:
P.H. is a 77-year-old man who has a history of type 2 diabetes, hypertension, and diabetic neuropathy. He controls his diabetes with his diet and hypertension with enalapril. He has severe numbness and tingling sensation in his feet, probably caused by neuropathy. He has A1c 7.2 and blood pressure under control.
The treatment will consist of maintaining him on his existing medications with a possible referral to a pain specialist to treat neuropathy. A follow-up is suggested after 3-6 months to check blood sugar levels, neuropathy, and kidney conditions.
Case 15: 74-Year-Old Black Female
Client Information:
- Patient Initials: L.W.
- Age/Gender: 74-year-old Black female
- Chief Complaint: Follow-up for bone density, mammogram, and urinary issues
Diagnosis:
- Osteopenia – ICD-10: M81.0
- Spinal Stenosis – ICD-10: M48.06
- Hypertension – ICD-10: I10
- Urinary Frequency with Blood (No Findings) – ICD-10: N39.3
Procedure:
- Bone density scan (osteopenia)
- Mammogram (negative)
- Urinary ultrasound
- Review of spinal imaging (degenerative spine)
Treatment Plan and Notes:
L.W. presents herself to the follow-up session after having a bone density scan report, which exhibits osteopenia, a normal mammogram, and recent spinal scans, which have reported degenerative spine and spinal stenosis. She also says that she has urinary frequency with some blood at times, but no results were noticed during urinalysis. She uses metformin and lisinopril to control diabetes and hypertension, respectively, and she has recently discontinued HCTZ.
The treatment plan will involve the continuation of her present medications, calcium/vitamin D supplementation for her osteopenia, and consultation with urology regarding her urinary symptoms. Knee pain will be treated with physical therapy, and this approach will be followed in three months to review her.
Case 16: 70-Year-Old White Male
Client Information:
- Patient Initials: D.T.
- Age/Gender: 70-year-old White male
- Chief Complaint: Sleep disturbances, fatigue, and nightmares
Diagnosis:
- Obstructive Sleep Apnea (OSA) – ICD-10: G47.33
- Chronic Fatigue – ICD-10: R53.83
- Nightmares – ICD-10: G47.51
Procedure:
- CPAP therapy review and adjustment
- Sleep study assessment
- Discussion of sleep hygiene
- Mental health evaluation for nightmares and fatigue
Treatment Plan and Notes:
D.T. is a 70-year-old man who has a history of sleep apnea and has CPAP therapy. He counts continuous fatigue, nightmares, and the inability to sleep at night. He has not been undergoing any notable changes in health in the recent past; however, he experiences falling asleep during the day and has some difficulty staying awake.
The treatment strategy involves the maintenance of the CPAP therapy, with possible changes in the settings, training on how to enhance his sleep hygiene, and mental health assessment to deal with his nightmares and fatigue. The effectiveness of interventions will be measured by a visit 1-2 months later.
Case 17: 70-Year-Old White Male
Client Information:
- Patient Initials: J.M.
- Age/Gender: 70-year-old White male
- Chief Complaint: Prostate cancer follow-up
Diagnosis:
- Prostate Cancer – ICD-10: C61
- Urinary Frequency – ICD-10: R39.15
Procedure:
- PSA (Prostate-Specific Antigen) levels test
- Biopsy results review
- MRI for prostate evaluation
Treatment Plan and Notes:
The patient, J.M., a 70-year-old male, was diagnosed with prostate cancer in 2022. He complains of frequent urination, especially at night. The PSA level has risen up to 10.2 (June 2025) and up to 5.9 (in April 2025). He is under a watchful waiting strategy and has been subjected to prescribed sildenafil, in which he encounters difficulties with urination. The treatment course will involve further monitoring of PSA levels and discussion over possible treatment options based on further PSA changes.
There will be a repeat MRI to check whether it has enlarged the prostate or has metastasized. The patient will proceed with sildenafil use as required to address the urinary frequency, and oncology follow-up will be done to carry out further assessment.
Case 18: 80-Year-Old Black Female
Client Information:
- Patient Initials: T.S.
- Age/Gender: 80-year-old Black female
- Chief Complaint: Hypertension, diabetes, and heart palpitations
Diagnosis:
- Hypertension – ICD-10: I10
- Dyslipidemia – ICD-10: E78.5
- Diabetes Mellitus Type 2 – ICD-10: E11.9
- Heart Palpitations – ICD-10: R00.2
Procedure:
- Comprehensive physical exam
- Blood pressure and heart rate monitoring
- Blood work, including lipid profile and A1c
Treatment Plan and Notes:
T.S. is an 80-year-old patient with hypertension, diabetes, and dyslipidemia. Her heart palpitations are occasional, dyspnea, and 4+ pitting edema in the lower extremities. She takes Lasix, Metoprolol, and Metformin. The treatment plan contains sustained drug therapy, surveillance of heart rate, and referral to soft tissue ultrasound. Fluid management and lifestyle changes will also be stressed.
Case 19: 71-Year-Old African American Female
Client Information:
- Patient Initials: S.P.
- Age/Gender: 71-year-old African American female
- Chief Complaint: Blood pressure follow-up
Diagnosis:
- Hypertension – ICD-10: I10
- Self-Monitoring of Blood Pressure (BP) – ICD-10: Z68.9
Procedure:
- Blood pressure monitoring at the clinic
- Review of home blood pressure readings
- EKG and heart ultrasound
Treatment Plan and Notes:
S.P. is a 71-year-old female with a hypertension history who does not control her blood pressure well after two blood pressure medications. BP at the time of her last visit to the clinic was 168/92 mmHg, but she says that the results are lower at home. This will be followed up by an EKG and heart ultrasound. The management plan will involve a dose increase of Amlodipine to 10 mg and additional training on how to monitor the BP of the patient at home.
A 2-week appointment will be set to recheck her BP. Besides, the patient will be reminded of the importance of taking drugs on schedule, modifying the diet, and stress reduction. She will also be referred to a nutritionist to advise her on the eating plans.
Case 20: White Male
Client Information:
- Patient Initials: M.L.
- Age/Gender: White male
- Chief Complaint: Chronic back pain, which resulted from a back injury in 2020
Diagnosis:
- Chronic Low Back Pain – ICD-10: M54.5
- Neuropathy (Moderate) – ICD-10: G62.9
Procedure:
- MRI and imaging of the back
- 7 months of physical therapy completed
- Pain severity rating and functional mobility assessment
Treatment Plan and Notes:
M.L. is a White male who reports chronic back pains, which occurred as a result of getting an injury when loading a box truck in July 2020. His pain is rated at 5/10 on a daily basis, and he flare-ups every few weeks or a few days. Various characteristics of the pain include dull, sharp, and tight and are exacerbated by sitting, standing, and lying. He is prescribed Tizanidine and Ibuprofen to relieve pain and visits the Back and Spine Center of Froedtert Hospital.
He requires numbness and tingling in both his lower limbs, and he does not indicate that the pain is too agonizing to walk and use assistive devices. A range of motion (ROM) and neuropathy are also included in the course of treatment. The VA will be placed with proposals on further treatment and therapy. A follow-up visit will be done within one year or as needed.
Case 21: 74-Year-Old White Male
Client Information:
- Patient Initials: R.M.
- Age/Gender: 74-year-old White male
- Chief Complaint: Overactive bladder
Diagnosis:
- Overactive Bladder – ICD-10: N32.81
Procedure:
- Urinary evaluation and frequency monitoring
- Review of current urology follow-up
Treatment Plan and Notes:
R.M. is a 74-year-old man with an overactive bladder and urinary frequency. He uses absorbent pads to control his leakage and has a lot of urinary frequency during the day and night.
The treatment plan is to continue the present medications (Myrbetriq, Terazosin, Alfluzosin) and observe the symptoms of urination. He will be relocated to a visit with the urologist every six months. The patient will also be informed about pelvic floor exercises and possible behavioral changes to deal with his symptoms.
Case 22: 82-year-old Black Male
Client Information:
- Patient Initials: B.L.
- Age/Gender: 82-year-old Black male
- Chief Complaint: Knee pain and essential tremor
Diagnosis:
- Bilateral Knee Pain – ICD-10: M17.9
- Essential Tremor – ICD-10: G25.0
Procedure:
- Comprehensive musculoskeletal and neurological exam
- Evaluation of joint pain severity and functional limitations
Treatment Plan and Notes:
B.L. is an 82-year-old man with essential tremor and bilateral knee pain. His knee pain has an average of 8/10, and situations of flare-ups amount to 9/10. To control his essential tremor, he employs weighted utensils. The management plan will comprise managing pain using Ibuprofen and referral to address physical therapy to make the knee muscles firm and free of pain.
In his tremor, he is going to be considered for treatment in the form of beta-blockers (Hunter et al., 2022). A follow-up will be undertaken to check the development of the symptoms.
Case 23: 39-year-old Black Female
Client Information:
- Patient Initials: A.K.
- Age/Gender: 39-year-old Black female
- Chief Complaint: Fainting and low WBC counts
Diagnosis:
- BUP/THC Positive – ICD-10: Z72.9
- Low White Blood Cell Count – ICD-10: D72.819
Procedure:
- Blood work to evaluate WBC count
- Referral to hematology
Treatment Plan and Notes:
A.K. is a 39-year-old woman who had fainting episodes and had low white blood cells. She is referred to hematology, but she has not yet done a follow-up. The treatment plan entails booking an emergency hematology appointment.
The monitoring of WBC and possible testing of the underlying conditions (infection or autoimmune disorders) will be prioritized (Mank & Brown, 2024). The patient will also be examined on aspects of lifestyle that may be affecting her health, such as substance use.
Case 24: 45-Year-Old White Male
Client Information:
- Patient Initials: BP.
- Age/Gender: 45-year-old White male
- Chief Complaint: Neuropathy and back pain
Diagnosis:
- Neuropathy – ICD-10: G63
- Herniated Disc (Previous Surgeries) – ICD-10: M51.9
Procedure:
- Neurological exam and pain assessment
- Review of herniated disc surgeries and history
Treatment Plan and Notes:
B.P. is a 45-year-old male with neuropathy and a history of multiple surgeries for herniated discs. He reports constant numbness and tingling with occasional burning sensations in his extremities. The course of treatment includes analgesia using gabapentin and additional physical activities in terms of muscle strength and movement. A follow-up period will be used to assess the effectiveness of his response to treatment and whether there is a need for other interventions, such as the nerve block or other medications.
Case 25: 40-Year-Old Black Female
Client Information:
- Patient Initials: C.J.
- Age/Gender: 40-year-old Black female
- Chief Complaint: Chronic back pain and seasonal allergies
Diagnosis:
- Seasonal Allergies – ICD-10: J30.9
- Chronic Low Back Pain – ICD-10: M54.5
Procedure:
- Physical exam for back pain
- Allergy testing and assessment
Treatment Plan and Notes:
C.J. is a 40-year-old female with chronic low back pain and seasonal allergies. She reports mild back pain, with flare-ups occurring during weather changes, and uses a back brace occasionally. The treatment involves maintaining back pain through physical therapy and prescribing her antihistamines or intranasal steroids to cure allergies.
She will be advised to get a subsequent consultation with a specialist on further management of allergies and observation of symptoms. It will be followed up on a later visit to assess progress.
Case 26: 37-Year-Old White Male
Client Information:
- Patient Initials: E.M.
- Age/Gender: 37-year-old White male
- Chief Complaint: Bilateral knee pain
Diagnosis:
- Bilateral Knee Pain – ICD-10: M17.9
Procedure:
- Joint examination and pain assessment
- Referral for physical therapy
Treatment Plan and Notes:
E.M. is a 37-year-old male with bilateral knee pain related to daily activity. He reports mild pain (3-4/10) that worsens with prolonged standing and walking. He is currently undergoing physical therapy and uses Ibuprofen for pain relief. The treatment schedule involves maintaining physical therapy in regard to mobility and strength.
Ibuprofen therapy will be used to maximize pain, and knee brace devices can be consulted (Hsu & Siwiec, 2023). Follow-ups will be conducted to assess the progress and the need to use additional imaging.
Case 27: 79-Year-Old White Male
Client Information:
- Patient Initials: W.T.
- Age/Gender: 79-year-old White male
- Chief Complaint: Prostate cancer follow-up
Diagnosis:
- Prostate Cancer – ICD-10: C61 (Rosario & Rosario, 2020)
- Fatigue – ICD-10: R53.82
Procedure:
- PSA level testing
- Urine sample for PSA level
Treatment Plan and Notes:
W.T. is a 79-year-old male with a history of prostate cancer. He underwent radiation therapy 29 times and has been receiving androgen injections every six months for three years. He reports occasional urinary leakage and fatigue. The treatment strategy involves the continued injection of androgen and observing the levels of PSA.
Fatigue control measures will be considered, and W.T. will be observed regarding cancer reoccurrence. We will make a second appointment to check his PSA and explore further treatment.
References
Cheung, A. K., Chang, T. I., Cushman, W. C., Furth, S. L., Hou, F. F., Ix, J. H., Knoll, G. A., Muntner, P., Pecoits-Filho, R., Sarnak, M. J., Tobe, S. W., Tomson, C. R. V., & Mann, J. F. E. (2021). KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney International, 99(3), S1–S87. https://doi.org/10.1016/j.kint.2020.11.003
El-Tallawy, S. N., Nalamasu, R., Salem, G. I., LeQuang, J. A. K., Pergolizzi, J. V., & Christo, P. J. (2021). Management of musculoskeletal pain: An update with emphasis on chronic musculoskeletal pain. Pain and Therapy, 10(1), 181–209. https://doi.org/10.1007/s40122-021-00235-2
Hsu, H., & Siwiec, R. M. (2023, June 26). Knee osteoarthritis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507884/
Hunter, C. W., Deer, T. R., Jones, M. R., Chien, G. C. C., D’Souza, R. S., Davis, T., Eldon, E. R., Esposito, M. F., Goree, J. H., Hewan-Lowe, L., Maloney, J. A., Mazzola, A. J., Michels, J. S., Layno-Moses, A., Patel, S., Tari, J., Weisbein, J. S., Goulding, K. A., Chhabra, A., & Hassebrock, J. (2022). Consensus Guidelines on Interventional Therapies for Knee Pain (STEP Guidelines) from the American Society of Pain and Neuroscience. Journal of Pain Research, 15(67), 2683–2745. https://doi.org/10.2147/JPR.S370469
Jamil, A., & Mukkamalla, S. K. R. (2023, July 17). Lymphoma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560826/
Lara-Esqueda, A., Zaizar-Fregoso, S. A., Madrigal-Perez, V. M., Ramirez-Flores, M., Montes-Galindo, D. A., Martinez-Fierro, M. L., Rodriguez-Sanchez, I. P., Guzman-Esquivel, J., Meza-Robles, C., Ceja-Espiritu, G., Kuri-Morales, P. A., Delgado-Enciso, J., Barriguete-Melendez, A., Galvan-Salazar, H. R., Barajas-Saucedo, C. E., Guillermo-Espinosa, E., Lara-Basulto, A. D., Gonzalez-Roldan, J. F., & Delgado-Enciso, I. (2021). Evaluation of medical care for diabetic and hypertensive patients in primary care in Mexico: Observational retrospective study. Journal of Diabetes Research, 2021, 1–7. https://doi.org/10.1155/2021/7365075
Mank, V., & Brown, K. (2024). Leukocytosis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560882/
Miotto, R., Percha, B. L., Glicksberg, B. S., Lee, H.-C., Cruz, L., Dudley, J. T., & Nabeel, I. (2020). Identifying acute low back pain episodes in primary care practice from clinical notes: Observational study. JMIR Medical Informatics, 8(2), e16878. https://doi.org/10.2196/16878
Purnell, J. Q. (2023, May 4). Definitions, classification, and epidemiology of obesity. Nih.gov; MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK279167/
Rosario, E., & Rosario, D. J. (2020). Localized prostate cancer. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK563248/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Patient Log
Throughout this course, you will also keep a log of patient encounters using Meditrek. AGPCNP students must record at least 100 encounters with GYN patients; FNP students must record at least 125 encounters with patients (100 GYN and 25 OB patients) by the end of this practicum.
The patient log must include the following:
- Client Information
- Diagnosis
- Procedure (Note: Make sure that, as you perform procedures at your practicum site, you also note those on your printed-out Clinical Skills List.)
- Treatment Plan and Notes
Case 1
Client is 35 years old black male
- Present for back pain from daily activities, daily back pain 6/10 sharp pain
- Pain aggravate with prolong sitting
- Medication: Ibuprofen
- Flare up once a up, severity 9/10, lasting 1-2 hrs, last 30 mins if lying down
- No hx of surgery or procedure
- Completed PT
- Service 2012-2019
- Denies loss of B/B control
- Occasional moderate tingling on left leg when bend down, slowly went away when stand up.
- Occupation: Jimmy John’s
- Denies SI or homeless
Case 2
Client is 73 years old retired white male
- FOllow up routine visit for non-hodgkin lymphoma left ear 2025
- SS: occasional sweating when wake up from sleep
- Service: 1970-1974
- Denies tenderness
- Follow by Hematologist once a year
- CBC done at visit
Case 3
Client is 51 years old black male
- Follow up visit for meniscus tear right knee
- X-ray done back in january 2025 and was refer to Orthopedic, but client was having trouble reaching out to them.
- Denies any prescription or OTC
- Denies hx of surgery or procedure
- Denies chest pain, palpitation, headache, fever, chill, numbness/tinging
- Lung and Heart sound normal
- Help schedule visit with Orthopedic on June 13 2025
Case 4
Client is 35 years old white male
- Visit for low back pain
- PHM: Inguinal hernia 2014, had surgery on hernia 2015, chronic low back pain 2014
- Denies injury, surgery or procedure
- Started physical therapy
- X-ray don previously on lower back
- Lower back pain daily, rated 4-5/10 sharp pain
- Flare up 10/10 weekly, lasting 3-4 days
- Take aspirin for pain
- Aggravate: bending over, prolong sitting, standing
- Used to have back brace before, but no longer using them
- Occasional mild numbness and tingling when flare up
Case 5
Client is 50 years old white male
- PHM: Sleep apnea 2015, IBS 1993, Rt ankle pain, Left ear surgery 2015, Grave Disease
- Use Cpap at night.
- s/s ongoing abdominal pain, diarrhea, loose stool 15-20 times per day
- Medication: Imodium
- Denies taking any meds for sleep
- Denies blood in stool or bleeding rectal.
- Followed by GI specialist,
- No surgery or procedure in GI
- Had CT scan, multiple colonoscopy and barium swallow study
Case 6
Client is 63 years old male
- PHM: CVS 2018, embolectomy 2018, right side weakness
- Service 1980-1985
- Followed by Neurologist, f/u appt in August
- Stroke impacted short term and long term memory
- Medications
- Aspirin 81mg po daily
- Atorvastatin 10mg po daily
- Baclofen 10mg po PRN daily
- Flexeril PRN
- Tizanidine PRN
- Seen by ST, PT, OT
- Depress d/t to feel inadequate for taking longer to do simple tasks and afraid will have another CVS
Case 7
Client is 45 years old male
- Routine physical follow up, last physical check was 2021
- No known allergies
- PHM: Hypertension
- Mom disease crohn disease, Dad alive
- Denies drug use
- Alcohol hard liquid 8-10 per weeks, smoke cigar 1-2 times a week
- Report did not his BP meds: Losartan 20mg and Amlodipine 5mg
- Today BP 168/92
- Sleep 5-8 hours per night
- Last eye exam was >2 years ago
- No change in hearing or vision
- Last saw dentist 2/25, f/u 8/25
- Denies rectal bleeding, rash, headache, Dizziness, lightheadedness
- Report easily bruising
- Lab order for CMP, CBC, UA, TSH
Case 8
Client is 60 years old black male
- Traumatic Brain Injury (TBI) 2018,sustained injury from jeep ran over him
- S/S: forgetful, unable to remember name, hard to recall certain things , hypersensitivity to light and sound, clonus, occasional headache, clonus
- PHM: Depression, Anxiety
- Has done CT of the head in the past
- Followed by Neurologist
- Denies surgery or procedure of the brain
Case 9
78 black female
- Stage 3 ckd
- Hypertension
- Low back pain
- Prediabetic
- Triglycerides 127
- Total cholesterol 189
- Hdl 40
- Ldl 97
- eGFR 47
- creatinine 1.18
- LFTs low
- Anemic
- A1c 5.8
- Takes metformin
- Metoprolol
- Atenolol
- Losartan
- Hr 98
- Referral to nephrology
Case 10
55 white male
- Scars on legs from getting stuck in the path of point-blank steam in 1993. Skin fell off legs. Remaining scars itch internally. Miss 2-3 days a year from skin infections. Miss more days from fatigue from itching interfering with sleep.
Case 11
67 black female physical
- Diabetes
- Hypertension
- Insect bites on back and arm
- Takes metformin
- Nifedipine
- Vitamin c
- Multivitamin
- Advil
- Recent glaucoma diagnosis
- CBC, CMP, vitamin D, A1c, urine tests
Case 12
60 Latino male
- Multiple myeloma
- Dx 2019 4 years remission
- Returned 2023- went to ED due to couldn’t walk
- Chemo pill every day for 21 days. Chemo infusions once monthly indefinitely
- 5 radiation treatments
- Took daily steroids but then was insulin dependent so stopped both steroids and insulin
- Body aches, joint pain, fatigue, immunocompromised, brain fog
Case 13
38 Asian male
- Apnea 2020 uses CPAP
- Back 2004
- Left knee (partail meniscus tear) 2009
- Right ankle sprain 2004
- Aircraft Iraq
- Back brace
- Knee brace
- Left knee pain 3/7 days 5/10 sharp pain, Flares to 6/10, can’t walk 2 days a month for 2-3 HOUR
- ankle brace
- Daily:
- Back pain 4/10 stiff increases with prolonged walking/ sitting
- Flares 4/7 days to 9/10 with spasms
- Takes tylenol, hot/cold
- Feet mildly numb and tingly without pain
- Ankle pain 4/10 increases with standing and walking, Flares 5/7 days to 8/10 and can’t walk 2 days a month for a half a day
- Tried physical therapy
Case 14
77 white male
- Diabetes 2
- Hypertension
- Diabetic neuropathy
- Takes enalapril 200/78, 178/82, 178/80
- Manage diabetes with diet A1c 7.2
- Moderate numbness and tingling in feet with severe pain
- Severe numbness, tingling, and pain in right thumb and first and second fingers. Right handed
- EMG 2015
Case 15
74 black female
- Follow up on bone density scan, mammogram, and MRI of head and x-ray of hips
- Bone scan revealed osteopenia- take multivitamin or calcium and d
- Mammogram negative
- Didn’t receive xray/MRI results
- 2023 x-ray shows degenerative spine, spinal stenosis
- Leukocytes low
- Cholesterol good
- eGFR 57 creatinine 1.03
- Takes metformin (A1c 7)
- Takes lisinopril, oxybutinin
- Stopped taking hctz due to dizzy
- C/o diarrhea for 6 months, urinary frequency with blood (None found in urinalysis), nausea and headache every two weeks
- Ordered ultrasound for urinary complaints
- Gi consult for gi complaints
- Physical therapy for bilateral knee pain/ swelling
Case 16
70 white male
- Apnea
- Cpap
- 2024
- Smoker-trying chantix
- Nightmares, fatigue, falls asleep during the day
- Served 76-94 and deployed to desert storm-exposed to burn pits, jet fuel, oil fields, sand storms
Case 17
70 white male
- Prostate cancer 2022
- Psa 5.9 april 2025
- Psa 10.2 June 2025
- Biopsy
- Watchful waiting
- ED-sildenafil
- Urinary frequency q 2 h at daytime
- 2-3 x per night
- MRI scheduled
Case 18
80 black female
- Hx cancer, PE, bilateral cataracts
- Hypertension, dyslipidemia, diabetes,
- Parents deceased
- 1 sister dementia
- 2 brothers
- Hearing impaired daughter
- Last vision exam 2023
- Last dental 2020
- Sleeps 4-5 hours at night, naps in daytime
- Firm/nontender submental nodes
- Right tm redness without c/o pain
- Heart Palpitations
- Sob exertion
- LCTA
- HRR
- 4+ pitting edema BLE
- Takes Lasix
- Metoprolol
- Metformin
- Xerelto
- Olmsartan
- Amlodipine
- Prevastatin
- Triamcinolone topical
- No smoking alcohol or drugs
- No neurological changes
- Ordered soft tissue ultrasound of neck and Ordered tubigrip stockings
Patient Logs
Case 19
71-year-old African American female presents for BP follow-up. Was taking 2 blood pressure medications. BP in clinic still elevated, with systolic in the 160s. Reports using a wrist BP cuff for self-checks at home. Denies headaches, coughing, heart palpitations, or SOB. Reports taking her BP at nighttime. Denies numbness/tingling/dizziness. Does not consume grapefruit products. After rest, BP recheck 140/82.
- Went to EKG appt. Still awaiting results.
- Plan: Increase amlodipine from 5mg to 10mg po qd. F/u in 2weeks or prn for BP recheck. Education on diet and exercise. Reorder echocardiogram and Order heart ultrasound.
Case 20
White male patient presents for routine VA visit. C/o chronic back pain, which resulted from a back injury in 2020.
- Injury occurred in July of 2020 while loading a box truck. Denies back surgeries or procedures.
- Reports imaging and MRI on back. Says that he completed 7 months of physical therapy.
- Back pain still occurs daily. Pain is rated 5/10. He takes tizanidine and Ibuprofen. Follows back and spine center at Froedtert hospital. Flareups occur every few weeks and lasts for days at a time.
- Pain is dull, sharp, and tight. Sitting, standing, and lying down all exacerbate pain. Denies pain being so bad that he cannot walk. Denies use of assistive devices or back brace. Reports numbness and tingling in bilateral lower extremities.
- Plan: ROM, neuropathy (moderate), and pain assessment. Recommendations for tx and therapy submitted to VA. Return in 1 year or prn.
Case 21
74 white male
- Overactive bladder since 2015
- Sees urology every 6 months
- Wears absorbent pads. Experiences leaking, weak flow, hesitency
- No UTIs no stones
- Urination q 2-3 h in daytime, 3-4 times at night
- Takes myrbetriq, terazosin, alfluzosin, amlodipine
Case 22
82 black male
- Bilateral knee pain
- Essential tremor in right hand. Right handed.
- Uses weighted utensils.
- EMG 2025
- No knee imaging. No pt.
- Daily 8/10 pain, left knee pops right knee aches
- Daily spontaneous Flares 9/10
- Takes ibuprofen
Case 23
39 black female
- Positive for BUP/THC
- feels hot/ cold/ faint during bowel movements
- Referred to hematology 3 x for low wbc counts, never went
- C/o “passing out” periodically
Case 24
Client is 45 years old white male
- Neuropathy, from jumped off top off humble during time of service
- Service 1990-1999
- 3 surgery on herniated disc for back surgery
- Use cane occasionally
- Constant moderate numbness/tingling with burning sensation on extremities, can be radom from movement and activity
- Medications: venlafaxine 225mg, OTC ibuprofen
- Last see Neurologist 2016
- Impacted client from doing his favorite hobby such bowling, tennis, running. Father was a professional bowler.
- Pain more severe in when first wake up in the morning, spouse help put on sock and clip nails
Case 25
Client is 40 years old black female
- Annual physical check up
- PHM: seasonal allergies, lower back pain
- Noted Red nasal passage
- Lung/heart, bowel sound clear. No edema on extremities
- Denies headache, chill, fever, sore throat, N/V, Dizziness, no skin rash
- Regular BM
- Chronic shoulder pain and lower back pain. Have a back brace but did not use them for awhile
- Due for PAP smear and mammogram, no menstruation, have IUD no menstruation
- See PT regularly
- Medication, Oxycodone, Vitamin D, Seroquel
- Smoker, Drink alcohol occasionally, use marijuana occasionally
Case 26
Client is 37 years old white male
- Bilateral knees pain 09/2024, started from daily activities
- Services: 1
- Denies injury, procedure, or surgery
- No Imaging done on the knees
- Currently doing PT
- Knees pain daily, on average rated 3-4/10 pressure, soreness pain
- Flare up daily, last 24 hours
- Aggravate prolong sitting, standing, walking
- Medication: Ibuprofen
- Pain occasionally relief with stretching, rest
- Pain impacted running, walking, playing with his kids
Case 27
Client is 79 years old white male
- Prostate cancer 2017
- Radiation done 29 times, No chemotherapy
- androgen injection every 6 months for 3 years
- Denies taking any prescriptions
- Occasional urinary leakage, denies blood in urine
- Ss: fatigue
- Follow by Urologist and Oncologist
- Urine sample done for PSA level