Operative Report Template
Name:
Part One: Operative Report
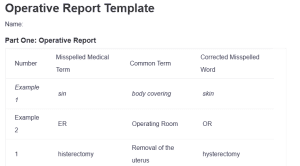
| Number | Misspelled Medical Term | Common Term | Corrected Misspelled Word |
| Example 1 | sin | body covering | skin |
| Example 2 | ER | Operating Room | OR |
| 1 | histerectomy | Removal of the uterus | hysterectomy |
| 2 | ophorectomy | Removal of ovaries | oophorectomy: Operative Report Template |
| 3 | urinarie | Urinary | urinary |
| 4 | incontinental | Loss of bladder control | incontinence |
| 5 | hemorhage | Bleeding | hemorrhage |
| 6 | pielonephritis | Kidney infection | pyelonephritis |
| 7 | cystcele | Bladder hernia | cystocele |
| 8 | vaginl | Vaginal | vaginal |
| 9 | muosa | Tissue | mucosa |
| 10 | blader | Bladder | bladder |
| 11 | enterocele | Bowel hernia | enterocele |
| 12 | interocele | Small bowel hernia | enterocele |
| 13 | suprapublically | Above pubic bone | suprapubically |
| 14 | SPARC needs | Surgical needles | SPARC needles |
| 15 | urethre | Urethra | urethra |
Part Two: HIM Terminology
Progress Note
- Purpose
Progress notes record the daily update of a patient’s care. They give an elaborative record of the progress, new observations, and modification of care treatment. These notes enable the provider to evaluate the effectiveness of interventions put in place and ensure continuity of care (Gao et al., 2023).
- Contents
Progress notes must contain a statement on the patient’s current condition, fluctuations of symptoms, treatment response, newly obtained diagnostic results, and provider instructions for continued care. Often, specific formats are adapted to maintain a standard, such as SOAP-Subjective, Objective, Assessment, and Plan.
- Settings
These notes are primarily used in hospitals, outpatient clinics, and long-term care facilities to monitor patients’ evolving conditions.
History and Physical (H&P)
- Purpose
The H&P serves as the foundational document during a patient’s initial evaluation. It provides a complete picture of the patient’s medical and physical status, guiding diagnostic and treatment decisions.
- Contents
Key elements include the chief complaint, medical history (personal and family), review of systems, physical examination findings, and initial diagnostic impressions. The document also identifies any pre-existing conditions relevant to the patient’s care (Nichol et al., 2024).
- Settings
H&P documentation is standard in hospitals for new admissions, surgical centers for preoperative assessments, and clinics during initial patient consultations.
Operative Report
- Purpose
The operative report provides a comprehensive account of surgical procedures, ensuring accurate documentation for medical, legal, and billing purposes. It also supports continuity of care for post-surgical follow-ups.
- Contents
The operative report outlines pre- and post-operative diagnoses, a step-by-step description of the procedure, anesthesia details, findings, complications, and estimated blood loss.
- Settings
Operative reports are critical in hospitals, ambulatory surgical centers, and specialized surgical clinics.
Discharge Summary
- Purpose
This document summarizes a patient’s hospitalization or care episode, providing essential details for follow-up care and transitions between healthcare providers.
- Contents
It includes the reason for admission, significant findings, procedures performed, treatments administered, the patient’s condition at discharge, and follow-up care instructions.
- Settings
Discharge summaries are commonly used in hospitals, rehabilitation facilities, and skilled nursing settings to guide post-discharge care.
In summary, all these documents play a vital role in health information management, ensuring quality patient care, legal compliance, and seamless communication among healthcare providers.
References
Gao, Y., Dmitriy Dligach, Miller, T., Churpek, M. M., Ozlem Uzuner, & Afshar, M. (2023). Progress note understanding — Assessment and plan reasoning: Overview of the 2022 N2C2 Track 3 shared task. Journal of Biomedical Informatics, 142(78), 104346–104346. https://doi.org/10.1016/j.jbi.2023.104346
Nichol, J. R., Nelson, G., & Sundjaja, J. H. (2024, April 30). Medical history. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534249/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
The Genitourinary System
Identify misspelled medical terms found in a patient’s operative report. Use the template to correct the terms’ spelling and change them into common terms. Write a 1–2 page paper that describes the purpose and contents of some of the types of documentation used in the HIM field. Specify the settings in which these documents would be used.
Introduction
In this assessment we will look at terms from the genitourinary system. This includes the urinary system and the male and female reproductive systems.
This assessment consists of two parts. In Part One you will review an operative report. During this course you have already looked at a progress note and an H&P. In the operative report you review as part of this assessment, you will change the medical terms you find into common terms.
You will also correct spelling errors that appear in the report. This will show your knowledge of diseases, treatments, and diagnostic tests associated with these important body systems.
In Part Two, you will write a 1–2-page paper that explains the different types of documentation in the health record. Knowing what is in, and the use of, each type of report is an important aspect of your role as a HIM professional.
Instructions
There are two parts to this assessment. Please complete both parts on the Operative Report Template and submit the one document..
Part One: Operative Report
Carefully review the operative report for a patient who is having a sling replacement to treat urinary frequency and incontinence. Next, download the Operative Report Template [DOCX] and complete all of the following on the template:
- Select 15 misspelled medical terms in the operative report and place them in Column 1.
- List one misspelled term per line.
- Place the correctly spelled medical term in Column 3.
- Change the 15 medical terms into commonly used terms in Column 2.
Preoperative Diagnosis: Urinary stress incontinence, cystocele.
Postoperative Diagnosis: Same.
Anesthesia: General.
History: This is a 49-year-old female with a history of a histerectomy and bilateral ophorectomy. She complains of urinarie frequency and incontinental. Options were discussed with patient, and she decided to proceed with a sling placement. Risks of the procedure were discussed and include hemorhage, UTI, pielonephritis, cystitis, vaginitis, MI, DVT, PE, death, and were deemed acceptable.
Operative Details: The patient was brought to the ER positioned, prepped and draped in the usual fashion. Time-out was called and patient identity and procedure being performed were validated. A Folley catheter was placed and the bladder drained. Allis clamps were placed on the posterior vaginal muosa.
A small incision was made, and the blader was lifted off of the vaginl mucosa. The cystcele was reduced. At this time, a minor enterocele was noted. Due to the small size, the interocele was not repaired.
Bilateral stab incisions were made suprapublically and SPARC needs placed into the superpubic incisions and pulled through the vaginal incisions. The SPARC mesh was attached to the needles and pulled up through the insicions. The mesh was positioned against the mid-urethre, sutured into place, and cut below the surface of the sin.
The skin was closed with 4-place suture; the vaginal incision was closed with 0-vicryl. The patient was transferred to the recovery room in stable condition.
Blood Loss: Minimal.
Part Two: HIM Terminology
Write a short, 1–2-page paper on some of the types of documentation used in the HIM field. Be sure your paper includes all of the following headings:
- Progress Note.
- History and Physical (H&P).
- Operative Report.
- Discharge Summary.
Under each heading, address each of the following:
- Describe the purpose of the document.
- Detail the contents included.
- Identify settings where the document would be used.
Consult the Capella Writing Center as needed for additional writing resources to help your write the paper portion of your assessment.
Additional Requirements
- Part One: Operative Report
- Format: Complete all columns on the Operative Report Template.
- Scoring Guide: Be sure to read the scoring guide to understand how your faculty member will evaluate your work.
- Part Two: HIM Terminology
- Written communication: Your paper does not need to be in APA format. It does need to be clear and well organized, with correct spelling, grammar, and syntax.
- Title Page: You do not need to include a title page with your paper. You do need to label it HIM Terminology.
- Name: Include your name in the upper right-hand corner on your paper.
- Length: Approximately 1–2 typed and double-spaced content pages in Times New Roman, 12-point font, not including the reference page.
Operative Report Template
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 2: Use medical terminology and abbreviations related to general structures and functions of the human body.
- Correctly spell medical terms related to general structures and functions of the human body.
- Change medical terms related to general structures and functions of the human body into common terms correctly.
- Competency 3: Use medical terminology and abbreviations related to body systems.
- Correctly spell medical terms related to body systems correctly.
- Change medical terms related to body systems into common terms correctly.
- Competency 5: Define medical terminology as used in health information management.
- Describe the purpose and contents of some of the types of documentation that are part of the health record.
- Identify settings where the documentation is used.
- Competency 6: Spell and pronounce basic medical terms.
- Identify misspelled medical and common terms.
- Competency 7: Communicate in a professional manner.
- Write clearly, with correct spelling, grammar, syntax, and good organization.