Management Plan for a Patient with Suspected Sexually Transmitted Infections
Treatment Plan
According to the differential diagnoses, the most probable diagnosis for the patient with vaginal discharge, mild pelvic discomfort, and pruritis is trichomoniasis, especially knowing her sexual history and clinical presentation. Trichomoniasis is a sexually transmitted infection caused by the protozoan Trichomonas vaginalis, which requires targeted treatment to eradicate the infection and prevent transmission, as stated by Schumann and Plasner (2023).
The conventional mode of managing this illness entails the use of metronidazole, which is an antiprotozoal drug. The recommended doses are 2 g of metronidazole once or 500 mg twice daily for seven days (Weir & Le, 2023). This treatment effectively eradicates the infection in most patients and prevents subsequent complications like pelvic inflammatory disease or further spread of the infection to partners.
Diagnostic Tests
To make a definitive diagnosis of trichomoniasis, a nucleic acid amplification test (NAAT) should be used because of its high sensitivity and specificity in identifying Trichomonas vaginalis, as revealed by Kissinger et al. (2022). Conversely, a wet mount microscopy test may be carried out, and motile trichomonads can be seen in the vaginal discharge sample. However, wet mount microscopy has low sensitivity compared to NAAT and, therefore, is not preferred over NAAT. The expected result from a positive NAAT would indicate the presence of Trichomonas vaginalis, directing the right treatment strategy.
Medications and Nonpharmacologic Treatments
As mentioned earlier, metronidazole is the cornerstone of pharmacologic treatment for this infection. The patient needs to be informed to finish the course of the prescribed medication even if symptoms begin to subside midway since this clears the infection entirely. The patient should also be advised to avoid the use of alcohol during metronidazole therapy and for at least 24 hours after the last dose of metronidazole due to nausea, vomiting, and flushing reactions (Kissinger et al., 2022).
Nonpharmacologic treatment includes educating the patient on safe sexual practices to avoid future episodes, such as the use of condoms. It is also essential to treat the patient’s sexual partners at the same time, even if they are experiencing no symptoms.
Suggested Consults/Referrals
Referral to a sexual health specialist or an infectious disease specialist is not always required in this situation unless there are such issues as persistent signs of the disease or suspected co-infection with other STIs, which would require exceptional management. However, referral to a gynecologist might be required in cases of recurrent infections or suspicion of PID or other complications.
Client Education
It is as evident that client education is an integral part of the management plan (Bhattad & Pacifico, 2022). The patient should be educated about trichomoniasis, how it is transmitted, the possible consequences if not treated, and the reasons for compliance with treatment. In the same regard, it is crucial to promote awareness of the need for testing and treatment of sexual contacts to avoid re-infection of the disease. The patient should be instructed not to have any sexual activity until the patient and her partners are done with the treatment and all symptoms are gone.
Follow-Up
The first post-treatment visit should occur one week after the completion of treatment to confirm that the symptoms have resolved and to identify any side effects caused by the medication administered. When the symptoms do not disappear, the test has to be repeated to determine the virus’s absence. Subsequent follow-up also presents a chance to review education on safe sexual practices and address any other issues that may be of concern to the patient.
References
Bhattad, P. B., & Pacifico, L. (2022). Empowering patients: Promoting Patient Education and Health Literacy. Cureus, 14(7). https://doi.org/10.7759/cureus.27336
Kissinger, P. J., Gaydos, C. A., Seña, A. C., Scott McClelland, R., Soper, D., Secor, W. E., Legendre, D., Workowski, K. A., & Muzny, C. A. (2022). Diagnosis and Management of Trichomonas vaginalis: Summary of Evidence Reviewed for the 2021 Centers for Disease Control and Prevention Sexually Transmitted Infections Treatment Guidelines. Clinical Infectious Diseases, 74(Supplement_2), S152–S161. https://doi.org/10.1093/cid/ciac030
Schumann, J. A., & Plasner, S. (2023). Trichomoniasis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534826/
Weir, C. B., & Le, J. K. (2023, June 26). Metronidazole. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK539728/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Management Plan for a Patient with Suspected Sexually Transmitted Infections
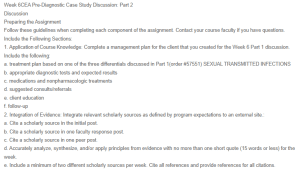
Week 6CEA Pre-Diagnostic Case Study Discussion: Part 2
Discussion
Preparing the Assignment
Follow these guidelines when completing each component of the assignment. Contact your course faculty if you have questions.
Include the Following Sections:
1. Application of Course Knowledge: Complete a management plan for the client that you created for the Week 6 Part 1 discussion. Include the following:
a. treatment plan based on one of the three differentials discussed in Part 1(order #57551) SEXUAL TRANSMITTED INFECTIONS
b. appropriate diagnostic tests and expected results
c. medications and nonpharmacologic treatments
d. suggested consults/referrals
e. client education
f. follow-up
2. Integration of Evidence: Integrate relevant scholarly sources as defined by program expectations to an external site.:
a. Cite a scholarly source in the initial post.
b. Cite a scholarly source in one faculty response post.
c. Cite a scholarly source in one peer post.
d. Accurately analyze, synthesize, and/or apply principles from evidence with no more than one short quote (15 words or less) for the week.
e. Include a minimum of two different scholarly sources per week. Cite all references and provide references for all citations.