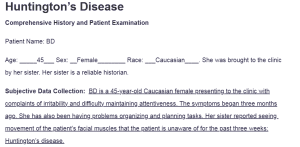
Huntington’s Disease
Comprehensive History and Patient Examination
Patient Name: BD
Age: _____45___ Sex: __Female________ Race: ___Caucasian____. She was brought to the clinic by her sister. Her sister is a reliable historian.
Subjective Data Collection: BD is a 45-year-old Caucasian female presenting to the clinic with complaints of irritability and difficulty maintaining attentiveness. The symptoms began three months ago. She has also been having problems organizing and planning tasks. Her sister reported seeing movement of the patient’s facial muscles that the patient is unaware of for the past three weeks: Huntington’s disease.
Past Medical History:
Allergies: NKFDA.
Medications: None.
Medical: The patient denies having been diagnosed with any physical or mental health illness. She also denies head injuries, hospitalizations, or ever being involved in an accident.
Surgical: Negative.
Health Maintenance: The patient’s last physical examination wason 1/2/2024.
Immunizations and Date if known: The patient is up to date with all her adult vaccines. She recently received her booster shot of COVID-19 Vaccine
Recent travel or Military service: N/A
Family Health History: None of her close family members has ever been diagnosed with a neurodegenerative disease.
Psychiatric Health History: Negative.
Nutritional Health History: The patient drinks two cups of coffee everyday.
Personal Habits: The patient has a regular night sleep routine and sleeps for 8 hours. She denies drinking alcohol or smoking. She also attends her clinical checkups regularly.
Review of systems (Subjective data):
HEENT: The patient denies visual changes and hearing loss.
Cardiovascular: Denies palpitations, irregularities in heart rate, or rhythms. Or edema.
Respiratory: Denies wheezing or shortness of breath.
Gastrointestinal: Denies any inconsistencies in her bowel movements.
Genitourinary: Denies dysuria, urinary frequency, or urinary urgency.
Musculoskeletal: The patient reports occasional muscle weakness, muscle stiffness, and difficulty walking.
Integumentary: Denies any skin changes.
Neurological: The patient suffers from frequent anger episodes. She also reports feeling hopelessness and anhedonia and sustained low mood for most of the day.
Endocrine: Denies heat or cold intolerance.
Hematologic/Lymphatic: Denies splenomegaly or anemia.
Immunological: Denies any allergies.
Female/Male Reproductive Organs: {Breast, Scrotal, Rectal, Vaginal}: Denies any breast lumps.
Physical Assessment (Objective data):
LOC: Alert and responsive. Appearance: Well-groomed. Speech: Goal-directed
Clinical Findings: Describe patient assessment in narrative format.
Skin, Hair, Nails: Consistent in coloration. No signs of scars.
HEENT: The patient exhibited a slow and hypometric gaze on the eye. Involuntary movements of the facial muscles are also evident. The nose is symmetrical. No signs of pain during swallowing.
Respiratory system: The chest is symmetrical. No signs of wheezing or shortness of breath.
Cardiovascular system: The heart rate is rhythmic. No gallop or pericardial friction rub sounds on auscultation.
Gastrointestinal system: The abdomen is symmetrical, smooth, and well-rounded. Abdominal sounds were heard on all four quadrants on auscultation.
Musculoskeletal system: There is a notable involuntary muscle movement on the patient’s arm. There is, however, no sign of joint swelling, rigidity, or restriction in the range of motion.
Neurological system: The patient is alert. She is also responsive and oriented to place. Her memory and judgment are intact.
Functional Assessment: The patient can follow commands.
ASSESSMENT:
- Huntington’s disease.
- Can result from aspiration related to dysphagia and dysarthria, which are common findings in patients with Huntington’s disease.
- Depression is a common manifestation in Huntington’s disease. The presence of anhedonia and depressed mood are highly suggestive of depression.
PLAN:
- The patient is at risk of Huntington’s disease progression. This may result in worsening of cognitive and motor disturbances. The plan is to start the patient on tetrabenazine for symptomatic control.
- The patient is at risk of pneumonia. The plan is to refer her to a language and speech therapist to prevent swallowing abnormalities.
- The patient is at risk of self-harm related to depression. The plan is to refer the patient to a counselor to help alleviate the depressive symptoms.
Completed by: ________________________________________________________________________
References
Andhale, R., & Shrivastava, D. (2022). Huntington’s disease: A clinical review. Cureus. https://doi.org/10.7759/cureus.28484
Stoker, T. B., Mason, S. L., Greenland, J. C., Holden, S. T., Santini, H., & Barker, R. A. (2021). Huntington’s disease: Diagnosis and management. Practical Neurology, 22(1), 32–41. https://doi.org/10.1136/practneurol-2021-003074
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
The SOAP note is a commonly used narrative transcription of a client’s health data. It can be used to identify and explain the client’s problem-oriented complaint and comprehensive history. For this assignment, utilize the attached Word document to record a comprehensive history and client examination in a narrative format.
Huntington’s Disease
- Subjective Data: What the client or family members tell you about the client’s signs and symptoms and the reason for seeking healthcare. Typically, this is documented by quoting the actual words said.
- Past Medical History is subjective data the nurse collects about any past medical history.
- A review of systems is subjective data collected as a list of the body systems obtained through a series of questions to identify signs and/or symptoms the client may be experiencing.
- Objective Data: Factual, measurable clinical findings such as LOC, vital signs, and clinical findings on assessment.
- Assessment: Evaluating clinical findings through Inspection, Palpation, Percussion, and Auscultation. All information obtained is documented in the client’s history and pathophysiology.
- Plan: Short-term and long-term goals and strategies that will be used to relieve the client’s problems.