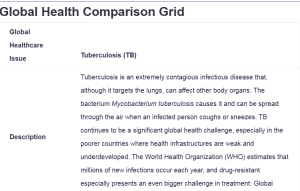
Global Health Comparison Grid
| Global Healthcare Issue |
Tuberculosis (TB) |
|
| Description | Tuberculosis is an extremely contagious infectious disease that, although it targets the lungs, can affect other body organs. The bacterium Mycobacterium tuberculosis causes it and can be spread through the air when an infected person coughs or sneezes. TB continues to be a significant global health challenge, especially in the poorer countries where health infrastructures are weak and underdeveloped. The World Health Organization (WHO) estimates that millions of new infections occur each year, and drug-resistant especially presents an even bigger challenge in treatment: Global Health Comparison Grid. | |
| Country | United States | India |
| Describe the policy in each country related to the identified healthcare issue | Policy: The US implements TB prevention and control policies through the Centers for Disease Control and Prevention (CDC) and local public health departments. The CDC’s Division of Tuberculosis Elimination (DTBE) focuses on surveillance, early detection, and treatment. The US prioritizes screening in high-risk populations, such as immigrants from high-prevalence countries, healthcare workers, and people with HIV.
Strategy: The policy involves systematic screening, case management, directly observed therapy (DOT) to ensure treatment adherence, and research funding for vaccine development. Additionally, the US collaborates with international agencies to address TB globally, especially drug-resistant TB.
|
Policy: India’s National Tuberculosis Elimination Program (NTEP) is the government’s flagship program for TB, aiming to eliminate TB by 2025. The policy involves free, universal access to TB screening, diagnosis, and treatment, including drug-resistant TB. India’s approach emphasizes public awareness campaigns, widespread access to diagnostic tools, and a significant focus on multidrug-resistant TB (MDR-TB) cases.
Strategy: India’s TB policy includes DOTS (Directly Observed Treatment, Short-Course) to promote treatment adherence, extensive community outreach, and partnership with private healthcare providers to improve detection and reporting. The program also includes cash assistance for patients to improve treatment adherence and address the social determinants of health-impacting TB transmission (Husain et al., 2021). |
| What are the strengths of this policy? | Comprehensive Surveillance and Prevention: The CDC’s TB policy ensures a sound surveillance system that provides early detection and thus promptly responds to limit the probability of community transmission of TB. Emphasizing high-priority groups ensures resources are directed where they are most needed.
Directly Observed Therapy (DOT): Standard implementation of DOT implies that patients receive complete treatment courses, which is an important part of preventing the emergence of drug-resistant TB strains (CDC, 2024). Research and Innovation Focus: The US policy focuses on funding and supporting research into TB, comprising vaccine development and innovative treatments; it thus contributes to global progress in TB control and ensures the possibility of better treatment options (Husain et al., 2021). International Collaboration: The US actively collaborates with global health organizations, helping to combat TB in high-burden countries. This cooperation strengthens TB management globally, reducing the incidence of TB importation into the US. |
Universal and Free Access to Diagnosis and Treatment: NTEP policy ensures that India provides free access to all TB services, especially to poor and rural populations, which helps reduce the overall burden of TB in the country.
Community-Based Approach and DOTS: The application of DOTS, coupled with community outreach programs, will, therefore, further reinforce the adherence to treatment in India. Community health worker support for patients leads to better program effectiveness through increased compliance. Focus on Multidrug-Resistant TB (MDR-TB): The policy in India specifically looks into the management of MDR-TB through the use of specific diagnostic tools and treatment protocols. Such specialization is in a sensitive area of TB control since drug resistance is a huge problem. Social Support and Financial Assistance: The policy will ensure cash incentives for TB patients to support them during their treatment. The social determinants of health are, therefore, tamed to reduce non-compliance with treatment due to economic reasons. |
| What are the weaknesses of this policy? | High Costs and Limited Access for the Uninsured: Most uninsured or underinsured people experience financial barriers to care, which stymie their ability to obtain TB treatment. As a result, numerous cases of vulnerable populations go undiagnosed or untreated.
Stigma and Low Detection in Certain Populations: The associated stigma of TB, especially in these high-risk populations, will make people not seek testing and treatment, perhaps leading to undetected cases and further spread of the disease. |
Resource Constraints and Healthcare Infrastructure Limitations: The heavy burden of TB in India burdens healthcare infrastructure, especially in rural areas, leading to a disparity in the quality and accessibility of the treatment accorded.
Challenges in Reaching Remote Populations: While the emphasis is made on community outreach in both remote and rural areas, logistical barriers often prove insurmountable, resulting in actual discontinuities of service and leaving some vulnerable populations less than adequately served.
|
| Explain how the social determinants of health may impact the specified global health issue. (Be specific and provide examples)
|
Economic Stability: The poverty and insecure sources of income among the uninsured may reduce the ability to access health services. For example, poor communities often forgo TB testing or treatment due to fears over costs.
Housing and Living Conditions: Congested and poor housing conditions in urban areas tend to affect the spread of TB since TB bacteria spread more easily when people remain in close proximity. It has also been identified that even homeless shelters may become high-risk environments for the spread of TB because close living arrangements and limited ventilation may be contributing factors (Nidoi et al., 2021). Health Care Access: Poor access to health care in rural and underserved communities reduces TB screening and delays treatment. For example, rural populations might have to travel long distances from their homes just to get to a TB clinic; accessing health care can be postponed or delayed due to great distances. |
Poverty and Employment: High rates of poverty and similarly high rates of informal employment in India nurture the malnutrition factor that, in turn, may weaken the immune system to the risk of acquiring TB. For example, many laborers in India are exposed to work environments filled with dust and other kinds of pollutants, which may raise their chances of suffering from TB or any respiratory infection.
Education and Health Literacy: In addition, limited health literacy, particularly in rural areas, has a negative effect on the understanding of the adherence to treatments concerning TB, making the treatment incomplete and resulting in further drug-resistant TB. An example includes the reliance on traditional medication among some populations, which limits seeking health care services that hasten the spread and worsen the course of TB. Social Stigma and Community Support: Much stigma is associated with TB in many regions, hence leading to a lack of desire or motivation on the part of individuals for testing or treatment due to fear from their communities. More common in rural villages where the disease is not well understood and may be seen as a type of curse or punishment, and people are thus secretive, seeking medical attention very late. |
| How has each country’s government addressed cost, quality, and access to the selected global health issue? | Cost: The US government, through the CDC and public health departments, pays for TB testing and treatment, particularly among high-risk populations. Public programs like Medicaid see to it that indigent cases are provided with low or no-cost treatments for TB. Uninsured individuals or those relying on public health services may have to pay expensive costs for treatment.
Quality: The CDC practices high standards of TB care by adopting evidence-based protocols for treatment, including directly observed treatment, which ensures adherence. This approach minimizes the emergence of resistance to drugs and ensures the quality of care is always consistent. Access: Generally, there is wide access to TB care in the US, especially through the public health clinics where most of the targeted high-risk populations are located. The government also makes sure that access is particularly ensured in correctional facilities, among the homeless, and within the immigrant population. However, access may be poor in rural areas or among populations that lack health insurance. |
Cost: The cost includes free diagnosis and treatment of TB to all citizens by NTEP, India. The support will be provided for drug-susceptible and drug-resistant TB. It is supported by the government in collaboration with international organizations, including the WHO, to secure funding and resources necessary to make treatment accessible without direct costs to patients.
Quality: India follows the WHO-recommended guidelines for the treatment of TB, including DOTS, to ensure adherence to the TB treatment regimen. However, the quality of standards varies across the country, with health facilities, particularly in rural areas, lacking the resources and sometimes the training to maintain care at similar standards. Access: Access has been widened by the Indian government through the establishment of TB services in both urban and rural settings. It is also provided with treatment by community health workers in remote areas. However, this is often restricted due to logistic barriers and, at times, health workforce shortages, particularly in the most inaccessible areas. |
| How has the identified health policy impacted the health of the global population? (Be specific and provide examples) | Advancing TB Research and Treatment: CDC and NIH have the lead in conducting research for TB by providing new diagnostic techniques, treatments, and ways of prevention. US-funded research has led to major developments in rapid molecular tests like the GeneXpert MTB/RIF assay, a test that can detect TB and drug resistance in hours rather than weeks. Currently, this is a globally used tool, especially in high-burden countries, to accelerate diagnosis and reduce the spread of TB.
Global Funding and Partnerships: The United States government has been one of the main donors to the Global Fund to Fight AIDS, tuberculosis, and malaria, providing huge amounts of financial support to TB programs in many countries worldwide. Subsequently, numerous developing and underdeveloped countries have been able to expand their TB treatment programs. As a result, millions of people get timely and effective treatment. For example, US funding for the treatment of TB is accessible both in Africa and Southeast Asia, where TB incidents are still high. |
Focus on High-Burden TB Elimination: India is among the countries bearing the highest burdens of TB. It recorded advances in the elimination of TB through its National Tuberculosis Elimination Program, with an ambitious aim to eliminate TB by 2025. The model for free and universal access to TB treatment is acting as a catalyst for other high-burden countries to take similar programs for mitigating their respective TB crises. For example, India’s strategy has influenced neighbors in the South Asia region to adopt similar strategies in handling TB from a public health perspective.
Development of MDR-TB Treatment Protocols: India’s focal commitment to the treatment of MDR-TB has contributed significantly to the accumulation of global experience in the management of drug-resistant TB. The Government of India, in collaboration with WHO and research institutions, has contributed to the development of better protocols for the treatment of MDR-TB. The protocols developed, including scaled use of bedaquiline for the treatment of MDR-TB in India, have been integrated into WHO guidelines and have since benefited MDR-TB treatment programs across the world. |
| Describe the potential impact of the identified health policy on the role of nurses in each country. | Screening and Preventive Measures: TB screening among the high-risk population is carried out by nurses; this further extends the role of nursing in prevention and assessment.
DOT Stands for Treatment Adherence: Nurses ensure treatment adherence through DOT, observing patients when they take medication and educating them on prevention against drug resistance. Public Health Education: Nurses educate communities in an effort to increase awareness, reduce stigma, and improve rates of TB testing among vulnerable populations. |
Primary Healthcare in Rural Areas: Nurses, being placed in rural communities, are entrusted with the primary responsibilities of TB caregivers through medication and monitoring.
DOTS and Patient Compliance: Nurses implement DOTS and facilitate compliance for patients through home visits and education regarding TB, an integral part of the management of MDR-TB. Community Outreach: They reach out to communities to educate them about TB prevention and the reduction of stigma, which is essential among the underprivileged. |
| Explain how global health issues impact local healthcare organizations and policies in both countries. (Be specific and provide examples) | Policy Adaptations to Prevent Importation of TB: Global TB prevalence has led US healthcare organizations to put in place strict policies of screening among high-risk populations, including immigrants and travelers from countries of high burden. For example, hospitals and clinics should make proper screening among newly arrived persons or those exposed to TB for a long time in the TB-prevalent areas.
Resource Allocation for TB Programs: As a result of the global burden of TB, US public health departments support local TB programs with resources, providing a broad approach that focuses on surveillance, testing, and treatment. This focus affects the distribution of funding and the training of healthcare staff, especially in regions with higher immigrant populations. Collaborative Research Programs: There is a response to Global TB through research collaborations between US-based institutions and global health institutions in the search for better diagnostic tools and treatment protocols that benefit local healthcare. Such collaboration with WHO and CDC has kept the US healthcare system in a state of preparedness for the response to drug-resistant cases of TB. |
Policy Emphasis on Universal TB Care: The high burden of TB in India ensures that local policies regarding free and accessible TB care for all drive healthcare organizations at every level. Public and private clinics alike have to follow the protocols of the NTEP, offering free diagnosis and treatment right down to the remotest rural areas.
Strengthening of Health Infrastructure at Grassroot Levels: The need to tackle TB has ensured the strengthening of basic health infrastructure in impoverished areas. For example, community health centers are provided with resources on diagnosis and treatment of TB, while the health workforce is specifically trained to handle cases related to TB, benefiting other spheres of community health in the process. More Community Outreach Programs: Global TB efforts have local organizations throughout India engage in wide community outreach programs focused on education and stigma reduction. Local health organizations collaborate with community leaders to engage in the promotion of TB awareness and adherence to treatment, ultimately enhancing community health. |
| General Notes/Comments | In the United States, addressing TB is multifaceted, wherein federal, state, and local health agencies take part. The CDC takes the lead in most initiatives on surveillance, prevention, and treatment in collaboration with all public health departments and hospitals in the country. Programs such as DOT and targeted screening for high-risk populations serve as a benchmark of early detection and adherence to treatment policies of the United States in order to prevent drug-resistant TB. These measures show the commitment of the federal government toward ensuring a high level of TB control while making it as cost-effective and accessible as possible. | The TB policy in India is well linked to the public healthcare system through the National Tuberculosis Elimination Program. A program comprising free diagnosis and treatment with DOTS has been established to address one of the biggest burdens of TB in the country. NTEP works in collaboration with local health centers and community health workers to reach underserved populations, especially in rural areas. The latter represents a commitment to health equity and underlines India’s approach of universal access and community-based outreach, which aligns with the national goal of eliminating TB by 2025. |
Plan for Social Change
Advocating for a Global Perspective in Local Practice and Nurse Leadership
I would promote a global health perspective in the nursing practice by informing nurses more about the global burden of TB and how it applies locally. I would facilitate workshops and training sessions on global TB statistics, treatment protocols, and the nurse’s role in managing infectious diseases. In cooperation with the public health departments, I would tailor the policies of our organization to best international practices, as recommended by the WHO. This would enhance preparedness within our organization and foster proactive measures that would facilitate the support of TB screening, treatment adherence, and patient education.
Impact of Incorporating a Global Perspective on Local Practice
The integration of an international perspective into the local practice of nursing assures cultural competence, allowing nurses to realize and respond more appropriately to social determinants in the care of TB patients. For example, applying the knowledge of social determinants like poverty and stigma compels nurses to strive for compassionate, personalized care, which improves patient outcomes. It would help a nurse leader understand the global TB crisis and support policy for early screening, culturally sensitive patient interaction, and adherence to treatment protocols by the patients. This integration enhances nurses’ roles as both caregivers and health advocates, promoting comprehensive, preventive care.
Contribution to Social Change
A nurse leader can achieve much social change within a community by adopting a global health perspective. Examples of this include the facilitation of no-cost, easily accessible TB screening in at-risk populations, coupled with proper culturally sensitive education to help alleviate some of the stigmas associated with TB and improve compliance with treatment regimens. These programs also help to reduce health disparity and increase health equity through equitable access to care and the pursuit of community well-being. Therefore, such a global view widens the approach toward health, inculcating an inclusive culture of responsibility and advocacy in tune with the goals of public health and helping society progress further as more resilient and health-oriented.
References
CDC. (2024, April 20). Tuberculosis infection control. TB Prevention in Health Care Settings. https://www.cdc.gov/tb-healthcare-settings/hcp/infection-control/index.html
Husain, A. A., Kupz, A., & Kashyap, R. S. (2021). Controlling the drug resistant tb epidemic in India: Challenges & implications. Epidemiology and Health, 43(78), e2021022. https://doi.org/10.4178/epih.e2021022
Nidoi, J., Muttamba, W., Walusimbi, S., Imoko, J. F., Lochoro, P., Ictho, J., Mugenyi, L., Sekibira, R., Turyahabwe, S., Byaruhanga, R., Putoto, G., Villa, S., Raviglione, M. C., & Kirenga, B. (2021). Impact of socio-economic factors on tuberculosis treatment outcomes in north-eastern Uganda: A mixed methods study. BMC Public Health, 21(1). https://doi.org/10.1186/s12889-021-12056-1
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Global Healthcare Comparison Matrix And Narrative Statement
If you talk about a possible poor health outcome, do you believe that outcome will occur? Do you believe eye contact and personal contact should be avoided? You would have a difficult time practicing as a nurse if you believed these to be true. But they are very real beliefs in some cultures.
Differences in cultural beliefs, subcultures, religion, ethnic customs, dietary customs, language, and a host of other factors contribute to the complex environment that surrounds global healthcare issues. Failure to understand and account for these differences can create a gulf between practitioners and the public they serve.
In this Assignment, you will examine a global health issue and consider the approach to this issue by the United States and by one other country.
To Prepare:
- Review the World Health Organization’s (WHO) global health agenda and select one global health issue to focus on for this Assignment.
- Select at least one additional country to compare to the U.S. for this Assignment.
- Reflect on how the global health issue you selected is approached in the U.S. and in the additional country you selected.
- Review and download the Global Health Comparison Matrix provided in the Resources.
The Assignment: (1- to 2-page Global Health Comparison Matrix; 1-page Plan for Social Change)
Part 1: Global Health Comparison Matrix
Focusing on the country you selected and the U.S., complete the Global Health Comparison Matrix. Be sure to address the following:
- Consider the U.S. national/federal health policies that have been adapted for the global health issue you selected from the WHO global health agenda. Compare these policies to the additional country you selected for study.
- Explain the strengths and weaknesses of each policy.
- Explain how the social determinants of health may impact the global health issue you selected. Be specific and provide examples.
- Using the WHO’s Organization’s global health agenda as well as the results of your own research, analyze how each country’s government addresses cost, quality, and access to the global health issue selected.
- Explain how the health policy you selected might impact the health of the global population. Be specific and provide examples.
- Explain how the health policy you selected might impact the role of the nurse in each country.
- Explain how global health issues impact local healthcare organizations and policies in both countries. Be specific and provide examples.
Part 2: A Plan for Social Change
Reflect on the global health policy comparison and analysis you conducted in Part 1 of the Assignment and the impact that global health issues may have on the world, the U.S., your community, as well as your practice as a nurse leader.
In a 1-page response, create a plan for social change that incorporates a global perspective or lens into your local practice and role as a nurse leader.
- Explain how you would advocate for the incorporation of a global perspective or lens into your local practice and role as a nurse leader.
- Explain how the incorporation of a global perspective or lens might impact your local practice and role as a nurse leader.
- Explain how the incorporation of a global perspective or lens into your local practice as a nurse leader represents and contributes to social change. Be specific and provide examples.
Global Health Comparison Grid
Assignment document should include:
- Title page
- Introductory paragraph
- Global health comparison matrix
- Plan for social change
- Conclusion
- References
Resources:
- Milstead, J. A., & Short, N. M. (2019). Health policy and politics: A nurse’s guide (6th ed.). Burlington, MA: Jones & Bartlett Learning.
- Corless, I. B., Nardi, D., Milstead, J. A., Larson, E., Nokes, K. M., Orsega, S., Kurth, A. E., … Woith, W. (2018). Expanding nursing’s role in responding to global pandemicsLinks to an external site.. Nursing Outlook, 66(4), 412–415.
- Donkin, A., Goldblatt, P., Allen, J., Nathanson, V., & Marmot, M. (2017). Global action on the social determinants of healthLinks to an external site.. BMJ Global Health, 3(1).
- Sandoval-Almazana, R., & Gil-Garcia, J. R. (2011). Are government internet portals evolving towards more interaction, participation, and collaboration? Revisiting the rhetoric of e-government among municipalitiesLinks to an external site.. Government Information Quarterly, 29(Suppl. 1), S72–S81.
- World Health OrganizationLinks to an external site. (WHO). (2021). World Health Organization (WHO). http://www.who.int