Final Systematic Literature Review – Substance Use Disorder (SUD)
Abstract
This systematic literature review aims at synthesizing available empirical and discussion literature on peer support programs as a key element in enhancing outcomes for clients that have substance use disorder (SUD) in different service delivery contexts. This systematic literature review only focused on peer-reviewed articles published between January 2020 and April 2025 using quantitative, qualitative, and mixed methods. The results affirm that peer support increases medication compliance, self-identified recovery outcomes, abstinence, and retention in the care of high-risk groups. Despite small sample sizes and self-reports in some studies, they remain feasible, culturally sensitive, and comprehensive. Peer support is a viable, person-centered adjunct to clinical treatment for SUD.
Final Systematic Literature Review
Problem
Description of the Problem
SUD is one of the biggest issues in modern society. It is a vital concern for the present-day population since it touches upon the inhabitants of various statuses, ages, and cultural backgrounds. SUD is a condition in which a person constantly uses substances that are toxic to the body, mind, social environment, and other relevant aspects of life.
Problem Significance
According to Castaldelli-Maia and Bhugra (2022), 2.2 percent of the global population experience drug use disorders from across the world. Moreover, more than 100,000 drug overdose deaths were recorded within one year in the United States of America (Kornfield, 2022). These statistics show an increase in the prevalence, and as such, there is a need for increased effort to address the situation. The absence of a supportive environment exposes SUD patients to the risk of relapse, mental health disorders, homelessness, imprisonment, and premature death.
Consequences of the Problem
SUD has economic and social implications since it creates burdens and expenses on the healthcare system, the judicial system, and social services. People recovering from SUD suffer from prejudice, stigma, social withdrawal, and lack of culturally competent treatment that complicates their path to recovery (Earnshaw, 2020). For social workers, the management of SUD aligns not only as a medical necessity but as a social justice issue. It is, therefore, crucial to understand and develop supportive interventions, especially those based on the client’s experiences of addiction.
Intervention
Peer support programs are a unique and person-centered model of substance use disorder intervention. They consist of people who have managed to come out of the numerous struggles affecting society. This mainly involves providing mutual support to people having gone through the same problem (Fortuna et al., 2022). In this way, mutual understanding and a non-emotional approach create a feeling of inclusion and support in a group. This connection makes it easier for people to feel understood in ways that clinical relationships may lack. The personal stories of peer supporters bring hope and strength of evidence to support recovery. Interpersonal aspects can build trust and strengthen the recovery process, and whenever they relate to people, they become more motivated to embrace the recovery process. Peer support is effective for people with substance use disorders.
Peer support programs may be structured in several ways; however, the most common aspects involve individual and group mentoring. It intends to provide the participants with space for discussion, strengthen their self-esteem, and increase personal responsibility. The peer supporters exemplify recovery because they show other clients that it is possible to recover from substance abuse and become productive members of society again (Ibrahim et al., 2022). This keeps participants interested and ensures they continue with treatment, and also discourages them from using unhealthy ways of handling stress. These interpersonal dynamics are of utmost importance in any recovery process. Over time, regular interactions with peers can help in managing mental health, reduce substance dependence, and enhance social relationships.
Besides emotional support, peer programs also offer more functional support when the participant needs to identify and address issues or seek resources such as health care treatment, housing, or legal aid. Some of the tasks carried out by peer workers include attending appointments with clients, helping them with paperwork, and advocating when they need help. As such, peer programs enable clients to overcome barriers that might hamper their recovery process. As a result, trust in the system is established, and there will also be increased engagement in services. It is not only the rehabilitation process that helps people but also encourages them to regain control of their lives.
Peer support is currently provided in diverse services, proving its flexibility and availability in different contexts. Such settings include hospitals, clinics, schools, correctional institutions, and other community structures. The availability of peer support in different settings guarantees that assistance is provided in the different stages of recovery. This makes it easier for clients to access these services since they can be introduced at early stages and maintained throughout. In conclusion, peer support programs increase not only the clinical success of treatment but also the well-being of the community.
Research Question
Therefore, due to the increasing interest in employing peer support programs and the need for personalized recovery-oriented approaches, this review aims to answer the question: How effective are peer support programs in improving outcomes for individuals with substance use disorder across various service settings? This question will help in framing the systematic literature review to determine what changes the programs offer, how the programs work to bring about the required changes, and the context within which the programs achieve efficiency.
Methods
Keywords and Databases Used
This systematic literature review seeks to establish the evidence on the effectiveness of peer support programs for persons with SUD. A structured search was done, and therefore, the databases APA PsycInfo Academic Search Ultimate, Pubmed, and CINAHL were used. Words like ‘peer support,’ ‘substance use disorder,’ ‘recovery,’ and ‘intervention’ were linked with Boolean operators to enhance the search relevance.
To help refine the results, Boolean operators such as AND and OR were included in the search. For example, using the phrase ‘peer support AND substance use disorder’ will only find articles that deal with both concepts; they were effective in improving the precision. The OR operator was also used in an attempt to include any study that might use equivalent terms or phrases of the filter terms to broaden the search to encompass more articles while enhancing its specificity.
Inclusion and Exclusion Criteria
The selection criteria covered only scholarly English articles published between 2020 and 2025, which focused on the discussion of peer-support intervention for individuals with substance use disorders. Research had to have presented quantitative, qualitative, or mixed results for the participants, including their experiences and results. The review only included research on the feasibility of self-tracking if it was conducted on various population types and service delivery contexts such as clinical, community, and online or digital contexts. On the other hand, studies were excluded if they were review studies, meta-analysis studies, theoretical, or editorials. Lastly, papers that addressed the issue of mental health on the individual or other addictions not linked with peer support for SUD were excluded in order to stay relevant to the research question.
From this search, 12 articles were selected according to relevance, methodological rigor, and the inclusion criteria used. The included studies focused on various patient populations and contexts, such as emergency departments, postnatal wards, adolescent peer support interventions, and digital media. Study characteristics were defined as follows: type of study design, participants’ characteristics, the context in which the study was conducted, methods and tools used, and study limitations.
The self-tracking approach meant listening to the patient’s experiences through the data, making the process more patient-centered and flexible. This captured the actual day-to-day dynamics and highlighted the problems faced and achievements made within a day, something that might not be apparent when using the more traditional assessment tools. These analyses reflected the principles of peer support and a person-centered approach as the data-focused participatory accounts of the participants. Thus, this methodological choice made the results more relevant and credible in substance use recovery.
Results
Article Selection Process
The database search provided 248 articles, of which only peer-reviewed articles were selected. Out of 248 articles, 34 were duplicates, so upon their elimination, 214 titles and abstracts were reviewed. Of these, 156 were excluded because they did not meet the inclusion criteria. A review of the 58 articles indicated that 46 studies could not report outcomes or had inadequate methods. The final review comprised twelve articles that met all criteria for analysis. The 12 studies focused on peer support for individuals with SUD that employed qualitative (n = 9), quantitative (n = 1), and mixed-methods (n = 2) approaches.
Overview Of the Articles
The studies incorporated methodological approaches such as descriptive, qualitative, mixed, and randomized controlled trials (RCTs). Specifically, two RCTs were identified; (Brady et al., 2022) conducted a digital peer intervention, while (Quilty et al., 2022) performed a school-based peer intervention. Some of the studies employed both quantitative and qualitative approaches, which included semi-structured interviews and recruited peer support workers or participants as observed from the articles such as (Brady et al., 2022), (Ibrahim et al., 2022) and (Bingham & Kelley, 2022). This approach is advantageous because it provides quantity and quality by measuring outputs and embraces subjectivities. In their study, Parkes et al. (2022) used a mixed-method approach, which helped to get a more extensive view of whether peer support works for homeless individuals, combining qualitative analysis and quantitative outcomes.
Across the studies, the sample ranges from a focused group of participants numbering from as few as six to twenty participants (Brady et al., 2022), (Gruß et al., 2021) and (Bingham & Kelley, 2022) and large-scale program patient samples of 1785 as in Avalone et al. Target populations included school-going youths, homeless adults, postpartum women, outpatients, and inpatient settings, indicating the versatility of peer support models based on the population. The geographical representation was the United States, Australia, Canada, Egypt, and the United Kingdom, thus increasing the global awareness of how Peer Support works in different healthcare organizations and other cultures.
Assessment tools relied on self-reports (Birrell et al., 2023) and (Quilty et al., 2022), program observation (Avalone et al., 2024) and (Liebling et al., 2020), and interviews for collecting qualitative data (Joo et al., 2022) and (Gruß et al., 2021). The benefits found by many of the studies were increased engagement, a decrease in stigma, and an increase in a positive emotional state. Some limitations included a small sample size, self-reported data, and social desirability. Turuba et al. (2023) found knowledgeably that having peers who assist the youth population ensures that young adults have continuity in service delivery for long-term recovery from SUD.
Themes
Increased Patient Engagement and Follow-up
A common feature of all the studies was that peer support enhanced service attendance and compliance with treatment recommendations. For example, in the Avalone et al. (2024) study, there is an indication that within the seven days following a peer intervention in the emergency departments, a proportion of the patients admitted for detoxification sought treatment services, but the exact percentage was not stated. In the same context, Liebling et al. (2020) noted 4,696 accepted referrals post peer support that was provided by patient navigators to substance use disorder treatment, noting that while such relationships served to facilitate first contact, they were a conduit to after-care as well. It also helped to increase social support for peers, reduce dropouts from care, and improve follow-up among marginalized groups.
Reduced Stigma and Improved Emotional Well-being
Another theme was a change in emotional health and decreased perceived stigma. Brady et al. (2022) and Bingham and Kelley (2022) showed how participants were pleased with coping gains and feelings of belonging due to accepting peers with similar experiences. In Birrell et al. (2023), participants who engaged in the “Mind Your Mate” app experienced a reduction in depressive symptoms with a coefficient (b) of -1.86 with a 95 percent confidence interval ranging from -3.73 to 0.02 and a Cohen’s d effect size of -0.31 which indicated a decrease in their depressive symptoms after one year which implies that the concept of peer support goes further than substance use but covers general well-being. These psychosocial benefits were particularly seen in marginalized groups such as pregnant women (Gruß et al., 2021) or Indigenous patients, where understanding the cultural background and common social identity in the group was an important therapeutic factor.
Harm Reduction
Many of the studies pointed at some of the benefits that can be attributed to harm reduction pertaining to specific services that peers offer. In the case of Parkes et al. (2022), SHARPS recorded lower rates of drug use among homeless people and a steady rise in the prescription of opioids. While the exact percentages were not given, the qualitative interviews highlighted significant improvements in stability and healthcare. Moreover, Gruß et al. (2021) indicated that the use of peer support in the management of pregnant and postnatal women was effective in enhancing coping strategies, treatment adherence, and abstaining from substance use during and after pregnancy. Respondents claimed that the real-life experience of their peer mentors warmed up the environment and made them trust other participants so they could sustain the change.
Discussion and Conclusion
This paper systematically reviewed twelve recent qualitative and quantitative peer-reviewed studies on the implementation and outcomes of peer support programs for people with SUD. The evidence highlighted that peer support enhances recovery by ensuring enhanced involvement, better emotional states, self-harm reduction, and social integration. For example, Avalone et al. (2024) and Liebling et al. (2020) compared the preferences of patients who received peer interventions in the emergency departments and inpatient services, respectively, and the results revealed that they tended to seek or accept detoxification services. This agrees with the notion that peer programs serve more as the recovery interface between the acute phase of care and the long-term treatment of SUD.
One of the shortcomings that most of the studies pointed out was the small sample sizes. Small sample sizes and non-randomized selection of participants reduce the external validity of the study’s results because the participants may not be representative of the population of individuals with SUDs. Furthermore, most of the reviewed studies employed self-report questionnaires that often result in recall and social desirability biases, for example (Ibrahim et al., 2022). However, there were some studies with larger sample sizes, such as (Avalone et al., 2024); there is a need to find even more studies with higher generalizability, such as randomized controlled trials. Therefore, there is clear evidence that peer support is practical in the reviewed literature. However, future studies should address methodological issues such as sampling and using the mixed-methods approach.
Although these limitations have been identified, the mentioned literature strengthens the role of peer support for various patient groups, particularly those in vulnerable or minority groups. Turuba et al. (2023) pointed to ongoing support as one of the key aspects of care delivered by peers. In contrast, Bingham and Kelley (2022) identified cultural relevance as the primary reason Indigenous participants are motivated to engage. Parkes et al. (2022) also poised that homeless individuals receiving peer-led harm reduction support reported reduced substance use and better access to healthcare. The applicability of peer models in various contexts ranging from hospitals to schools and web-based environments suggest their utility and cost-effectiveness in practice facilities that are operational to social work practice.
The findings hold significance for practice and policy. First, peer support should be implemented as a standard part of SUD treatment modalities, and peer workers should be provided with adequate education and certification. Based on Brady et al. (2022), an intervention involving peer support at different workplaces effectively decreased employee’s stigma and improved their coping strategies within the required SUD. Equally, digital peer interventions such as “Mind Your Mate” (Birrell et al., 2023) can assist in expanding coverage of peer support programs. Social work practitioners can deliver and assess such interventions due to their ability to replace or complement clinical practice in encouraging the process of recovery.
Therefore, this systematic review supports the broad notion that peer support programs enhance the recovery process of people with SUDs. In emergency departments, schools, and other youth population programs, peer approaches help to build trust, decrease prejudice, and increase compliance with treatment. Nevertheless, the field could be improved by a larger sample size and empirical evaluations to build generalizable evidence. In summary, peer support is a person-centered modality that is particularly noteworthy because of its compatibility with social work principles and the evidence showing its potential as an adjunct to standard substance use treatment. It is therefore recommended that future research and practice build upon these programs to enhance the effectiveness of the programs across service delivery settings.
References
Avalone, L., Lalane, M., King, C., Pfeiffer, K., Linn-Walton, R., & Barron, C. (2024). Integrating substance use peer support and screening brief intervention and referral to treatment services in the emergency department: A descriptive study of the ED leads program. Addiction Science & Clinical Practice, 19(1). https://doi.org/10.1186/s13722-024-00445-x
Bingham, D., & Kelley, A. (2022). Rethinking recovery: A qualitative study of American Indian perspectives on peer recovery support. Journal of Ethnicity in Substance Abuse, 1–14. https://doi.org/10.1080/15332640.2022.2082620
Birrell, L., Debenham, J., Furneaux-Bate, A., Prior, K., Spallek, S., Thornton, L., Chapman, C., & Newton, N. (2023). Evaluating a peer-support mobile app for mental health and substance use among adolescents over 12 months during the COVID-19 pandemic: Randomized controlled trial. Journal of Medical Internet Research, 25, e45216. https://doi.org/10.2196/45216
Brady, L. A., Wozniak, M. L., Brimmer, M. J., Terranova, E., Moore, C., Kahn, L., Vest, B. M., & Thomas, M. (2022). Coping strategies and workplace supports for peers with substance use disorders. Substance Use & Misuse, 1–7. https://doi.org/10.1080/10826084.2022.2112228
Castaldelli-Maia, J. M., & Bhugra, D. (2022). Analysis of global prevalence of mental and substance use disorders within countries: Focus on sociodemographic characteristics and income levels. International Review of Psychiatry, 34(1), 6–15. https://doi.org/10.1080/09540261.2022.2040450
Earnshaw, V. A. (2020). Stigma and substance use disorders: A clinical, research, and advocacy agenda. American Psychologist, 75(9), 1300–1311. https://doi.org/10.1037/amp0000744
Fortuna, K. L., Solomon, P., & Rivera, J. (2022). An update of peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatric Quarterly, 93(2), 571–586. https://doi.org/10.1007/s11126-022-09971-w
Gruß, I., Firemark, A., & Davidson, A. (2021). Motherhood, substance use, and peer support: Benefits of an integrated group program for pregnant and postpartum women. Journal of Substance Abuse Treatment, 131, 108450. https://doi.org/10.1016/j.jsat.2021.108450
Ibrahim, N., Selim, A., Ng, F., Kasaby, M., Ali, A. M., Eweida, R., Almakki, D., Elaagib, A., & Slade, M. (2022). Experiences of peer support workers supporting individuals with substance use disorders in Egypt: Phenomenological analysis. BMC Health Services Research, 22(1). https://doi.org/10.1186/s12913-022-08393-5
Joo, J. H., Bone, L., Forte, J., Kirley, E., Lynch, T., & Aboumatar, H. (2022). The benefits and challenges of established peer support programs for patients, informal caregivers, and healthcare providers. Family Practice, 39(5), 903–912. https://doi.org/10.1093/fampra/cmac004
Kornfield, M. (2022, May 11). U.S. surpasses record 100,000 overdose deaths in 2021. NCBI. https://www.ncbi.nlm.nih.gov/search/research-news/16178
Liebling, E. J., Perez, J. J. S., Litterer, M. M., & Greene, C. (2020). Implementing hospital-based peer recovery support services for substance use disorder. The American Journal of Drug and Alcohol Abuse, 1–9. https://doi.org/10.1080/00952990.2020.1841218
Parkes, T., Matheson, C., Carver, H., Foster, R., Budd, J., Liddell, D., Wallace, J., Pauly, B., Fotopoulou, M., Burley, A., Anderson, I., & MacLennan, G. (2022). A peer-delivered intervention to reduce harm and improve the well-being of homeless people with problem substance use: The SHARPS feasibility mixed-methods study. Health Technology Assessment, 26(14), 1–128. https://doi.org/10.3310/wvvl4786
Quilty, L. C., Wardell, J. D., Garner, G., Elison-Davies, S., Davies, G., Klekovkina, E., Corman, M., Alfonsi, J., Crawford, A., de Oliveira, C., & Weekes, J. (2022). Peer support and online cognitive behavioral therapy for substance use concerns: Protocol for a randomized controlled trial. BMJ Open, 12(12), e064360. https://doi.org/10.1136/bmjopen-2022-064360
Scannell, C. (2021). Voices of hope: Substance use peer support in a system of care. Substance Abuse: Research and Treatment, 15. https://doi.org/10.1177/11782218211050360
Turuba, R., Toddington, C., Tymoschuk, M., Amarasekera, A., Howard, A. M., Brockmann, V., Tallon, C., Irving, S., Mathias, S., Henderson, J. L., & Barbic, S. (2023). “A peer support worker can really be there supporting the youth throughout the whole process”: A qualitative study exploring the role of peer support in providing substance use services to youth. Harm Reduction Journal, 20(1). https://doi.org/10.1186/s12954-023-00853-3
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Final Systematic Literature Review – Substance Use Disorder (SUD)
Please do write The Final Paper.
Instruction from the professor,
Systematic Literature Review Paper
In this assignment, you will use your knowledge (practice + research) to search for effective practices within your area of interest. The purpose of this assignment is to write a paper that a provider, organization, agency, or community could review to inform their practices or policies.
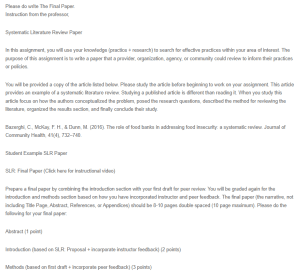
Final Systematic Literature Review – Substance Use Disorder (SUD)
You will be provided a copy of the article listed below. Please study the article before beginning to work on your assignment. This article provides an example of a systematic literature review. Studying a published article is different than reading it. When you study this article focus on how the authors conceptualized the problem, posed the research questions, described the method for reviewing the literature, organized the results section, and finally conclude their study.
Bazerghi, C., McKay, F. H., & Dunn, M. (2016). The role of food banks in addressing food insecurity: a systematic review. Journal of Community Health, 41(4), 732–740.
Student Example SLR Paper
SLR: Final Paper (Click here for instructional video)
Prepare a final paper by combining the introduction section with your first draft for peer review. You will be graded again for the introduction and methods section based on how you have incorporated instructor and peer feedback. The final paper (the narrative, not including Title Page, Abstract, References, or Appendices) should be 8-10 pages double spaced (10 page maximum). Please do the following for your final paper:
Abstract (1 point)
Introduction (based on SLR: Proposal + incorporate instructor feedback) (2 points)
Methods (based on first draft + incorporate peer feedback) (3 points)
Results (9 points) The result section should only describe the results and should not include your opinion or any conclusive statements. Once again review the SLR articles carefully. These are the main parts to the results section, each with a different function:
The results include the number of articles you found so start with that. The reader should understand how you went from initially finding XX articles to 12 articles that you included in your review. (1 point)
Provide an overview of the articles so that a reader can understand the variety of study designs, sampling techniques, measurement tools etc. Use the information from your SLR: Table of Articles to describe and summarize the articles you found (3 points)
This table should be included as Appendix A. You should refer to this table in the text (Example: A summary of the reviewed articles is presented as a table in Appendix A for review). (1 point)
If there are interesting insights from a particular study, you can describe those more specifically. You may create subheadings within the result section as needed.
Finally, provide 2-3 themes that you found across your studies. Remember the table provides findings for each study whereas the narrative you write provides themes for findings across studies. Also don’t just say that intervention was effective. Tell the reader what percentage of participants improved by how much due to a particular intervention. Based on all these findings you can later conclude that the intervention was effective. (4 points)
Use subheadings to organize your themes. Instead of describing and summarizing, you should be integrating and analyzing articles. Use your critical appraisal skills.
Conclusion/Discussion (9 points) The last section is a combination of discussion and conclusion. The goal of this section is to wrap up your paper, re-focus on some of the highlights of what you found, discuss a few limitations, and discuss the implications of your findings (answer your research question from your introduction section!). Make sure that whatever you write in this section is based on something mentioned earlier. For example, in your results section, you might point out that most of the studies were based on a small sample size.
So in your discussion/conclusion section, you can say something like:
“although the studies showed that the intervention was effective, we should note that most of the studies were based on a very small sample size. This is a major limitation because of our inability to generalize the findings. Further research should consider different study designs to ensure they have larger sample sizes. Similarly, practitioners should evaluate the interventions to ensure that it is effective in their unique context.”
This is just an example and written in a general way but shows how to take a finding about sample size, discuss its limitations, and derive implications for both research and practice. In other words, how does this SLR inform social work? Please go through the SLR articles and see how they write their discussion/conclusion section.
Writing: (1 points)
The paper should be well organized with the use of headings and subheadings. Each statement should be properly supported with logical arguments. Paragraphs should have proper transitions such that it is not difficult to follow your thought process. Please edit the paper so that it does not have grammatical errors and difficult to understand sentence structures. Please use APA 7th ed style for citations and references. Also do not use too many quotes. As a rule of thumb, you may only use one quote per paper and only if it is defining something or citing legal language.
This is the “peer review feedback” from the “Peer review paper” you wrote.
Peer Review Feedback
The submitted systematic literature review (SLR) focused on finding what makes peer support programs, for individuals struggling with substance use, effective. A massive component of the healing and recovery journey of sobriety is finding a community that an individual can be vulnerable and honest with-in order to best hold accountability. This peer review will focus on the comprehension of the methodological process of their SLR, accuracy and clarity of the results provided, appropriate and effective connections between the discussion/conclusion, as well as any other supportive feedback the peer had requested.
Methods:
Keywords & Databases:
This section was clear and concise in its informational aspect to relay what databases were utilized, and what search terms were used as well.
Feedback:
There could be a benefit from explaining, briefly and concisely, what Boolean operators were utilized and what the effective results were of using such search methods/mechanisms.
Inclusion & Exclusion:
The criteria for this SLR was clear and comprehensible based upon the transparency of why certain academic writing was excluded and the time frame for which certain journals and articles were reviewed. The explanation of study characteristics were clear and appropriate to understand the writer’s focus for the SLR.
Feedback:
There could be some clarity on why this SLR focusing on reviewing articles with only self-tracked data felt more applicable to the overarching question for the review, rather than obtaining data that was self-tracked, clinically tracked, and/or both self/clinically tracked.
Results:
This section was well-written and precise in the process of narrowing what articles were utilized for the SLR. Relaying what demographics were observed in the articles/studies reviewed and the common themes were concise and relatively specific in descriptions. Some characteristics of participants were unclear.
Feedback:
There could be some specification about the age range of the participants, if there happened to be a median age found. The context of age can help a reader comprehend the effectiveness of a peer group/support system at certain ages, and what a lack of such support at certain age markers (young 20s, mid 50s-60s for example) would impact the recovery and development of safety and sobriety. (Younger populations may increase their uptake of their substance if there is a common lack of support found).
Discussion & Conclusions:
This section seemed to have clear structure and an objective/balanced perspective on the theme of the SLR. Because a big part of SLR’s include the idea of further implications, this section seemed to do a good job in describing clear ideas to better improve on the understanding of how effective peer-support models/groups are to the process of treatment.
Feedback:
There is some sentence structuring that could be conveyed a bit more clearer by condensing the phrasing to better explicitly express the point being made(ie, condensing the sentence about shame and guilt reduction/mutual understandings in the therapeutic relationships). Transitionary phrasing could also help with the flow of the review, when discussing the limitations of some reviews and leading into implications for the future. Additionally, the inclusion of more specific examples or data metrics of works cited could be helpful in impactfully emphasizing the message being conveyed in this review.
Writing, Formatting, and Final Thoughts:
The writing and formatting of this review, so far, seems to be clear and fairly specific in its reporting. There are clear steps written about data collected, and such data is reported upon as best as possible. It does seem like themes are connected between results reported on and the discussion/conclusion. The ending section also relays relevant implications that could be introduced with regard to the theme of this SLR but could benefit from more explicit ideas and data for why such implications are beneficial. Overall this paper seems to have a strong grasp of this important aspect of sobriety and therapy, and is quite intriguing. Nice work 🙂