Disorders of Endocrine Control of Growth and Metabolism
The Importance of the Free T4 Level When Testing for Hypothyroidism
The measurement of the free T4 level is important as T4 is a major thyroid hormone. The total T4 measurement during the hypothyroidism test focuses on the bound and free hormone levels. The TSH stimulates and controls T4 and vice versa. This makes measuring the levels of free T4 an indicator of the risk of developing hypothyroidism. T4 is the primary thyroid hormone made by the thyroid gland. It is, therefore, in an inactive form. The measurement is based on the process of conversion of inactive T4 to the active form T3. T4 requires deiodination through the enzyme deiodinase to remove the iodine molecule (Bayse et al., 2020). This conversion of T4 to T3 makes it usable. However, poor deiodination or conversion of the T4 leads to the availability of free T4 in the blood system, leading to the development of majorly notable hypothyroid symptoms such as the ones manifested by Bertha. The 71-year-old woman shows symptoms like sensitivity to cold temperatures, difficulty concentrating and communication, fatigue, and depression. It should be noted that although TSH influences TSH’s conversion, poor conversion can occur irrespective of normal TSH level. Therefore, measuring the levels of T4 can help indicate poor conversion to the active T3, helping narrow down the causes of the hypothyroid symptoms manifested.
The Indication of the TSH and T4 Test Results in Someone with Primary Hypothyroidism
Primary hypothyroidism is majorly caused by Hashimoto’s thyroiditis, an autoimmune disorder of the thyroid gland that causes the body’s immune system to attack the thyroid (Hirtz et al., 2021). The symptoms of primary hypothyroidism may differ or conflict with other conditions from patient to patient. Therefore, blood tests focus on T4 and TSH levels. The different levels of both hormones can indicate a malfunctioning thyroid, either underactive or overactive.
High levels of TSH indicate an underactive thyroid. An underactive thyroid means that there are lower levels of thyroid hormones, T4 and T3, thus hypothyroidism. Therefore, the pituitary gland initiates an overproduction of TSH in order to stimulate the thyroid gland to improve the levels of T4 and T3. On the other hand, lower levels of TSH indicate an overactive thyroid. This means that the thyroid gland is producing more T4 and T3 hormones. In this case, the pituitary gland produces less TSH to reduce thyroid function.
High or low levels of T4 after a blood test indicate a malfunctioning thyroid, which creates an imbalance between the levels of T4 needed by the body’s systems and the amount the thyroid gland produces. High T4 levels indicate an overactive thyroid when low levels are needed, while low levels indicate an underactive thyroid.
Why Bertha’s Respiratory Rate Was Decreased
A majority of diseases affect the production of thyroid hormone in the body as it controls metabolism and growth and affects other body processes and functions, including respiration (Shahid et al., 2022). The effects of the thyroid hormones on the body systems and control of breathing can be used to explain why Bertha’s respiratory rate decreased. Hypothyroidism will affect how the alveolar opens and ventilates. In Bertha’s case, the hypothyroidism may have caused her alveolar to hypoventilate, which means that her lungs were not opening as required to support respiratory gas exchange. Therefore, for her respiratory rate to reduce, she needed to breathe harder to open up the lungs to support sufficient respiratory gas exchange.
The other reason that affected and reduced Bertha’s respiratory rate is the respiratory muscle weakness that occurs with hypothyroidism. Hypothyroidism may have caused her respiratory muscles, including the diaphragm and intercostal muscles, to have decreased strength due to various reasons, such as reduced blood oxygen and increased carbon monoxide concentration in the blood. The reduced respiratory strength, causing reduced expiratory and inspiratory pressures within the chest cavity and lungs, led her to have reduced respiratory rates. Hypothyroidism may also impact pulmonary functioning due to reduced blood oxygen.
Why Pleural Effusion Might Be Present In a Person with Hypothyroidism
Pleural effusion develops as a result of fluid building up within the lung cavity within the regions of the pleura outside of the lungs. The pleura helps lubricate the chest cavity to allow smooth breathing. For normal tests, pleural effusion can be identified within the pleura. Although rarely, pleural effusion might be present in someone with hypothyroidism due to some factors. For Bertha, pleural effusion might be present as she struggles to improve her alveolar hypoventilation through forced breathing; a few capillaries of the alveoli could have burst or leaked into the lungs or in the pleura. This may lead to the accumulation of blood within the pleural membranes, leading to the development of pleural effusion in patients with hypothyroidism. Throughout the capillary leak, the patient may not show any symptoms of leakage or bleeding, which may further worsen the pleural effusion condition before it can be identified. Besides this explanation, another reason that might lead to the presentation of pleural effusion in a patient is that hypothyroidism affects pulmonary action, which can lead to heart complications.
Factors in Bertha’s History That Leave Her Susceptible To a Myxedematous Coma
Myxedematous coma is an extreme complication of hypothyroidism, which is also related to multiple abnormalities in various organs that alter senses and sensations (Shahid et al., 2022). In patients with hypothyroidism, it can be manifested by multiple physiologic alterations as the body seeks to compensate for the deficiency of the thyroid hormone (Shahid et al., 2022). It develops as the body seeks to control and maintain homeostasis. This makes myxedematous coma a common symptom in patients with hypothyroidism. There are various factors that can be identified from a patient’s history that can determine their susceptibility to myxedematous coma.
In Bertha’s case, her history shows that she lives in cold climatic conditions, as she grew sensitive to cold temperatures after she was done shoveling snow outside their house. Hypothermia is a predisposing factor for developing myxedema coma in patients with hypothyroidism (Shahid et al., 2022). She also had pneumonia last winter, contributing to an increased risk of developing myxedematous coma. Besides these, Bertha has a longstanding case of hypothyroidism and has been taking medications for Hashimoto thyroiditis, which further predisposes her to develop myxedematous coma.
Physiologic Aspects Involved In a Myxedematous Coma
Myxedematous coma can develop as a result of conditions that produce thyroid abnormalities, which affect the body’s capacity for homeostasis. The failure of the thyroid gland to regulate the production of T4 and T3 in patients with hypothyroidism leads to failure to maintain the processes regulated by thyroid activity. For example, neurovascular adaptations, including peripheral vasoconstriction, diastolic rate and pressure, and blood volume. The failure of these neurovascular adaptations leads to chronic peripheral vasoconstriction, reduced diastolic pressure, and reduced blood volume, which risks hypotension. This leads to the inability to maintain homeostasis, leading to myxedema coma in hypothyroid patients.
References
Bayse, C. A., Marsan, E. S., Garcia, J. R., & Tran-Thompson, A. T. (2020). Thyroxine binding to type III iodothyronine deiodinase. Scientific Reports 2020 10:1, 10(1), 1–10. https://doi.org/10.1038/s41598-020-72243-9
Hirtz, R., Föcker, M., Libuda, L., Antel, J., Öztürkb, D., Kiewert, C., Munteanu, M., Peters, T., Führer, D., Zwanziger, D., Hebebrand, J., Thamm, M., & Grasemann, C. (2021). Increased Prevalence of Subclinical Hypothyroidism and Thyroid Autoimmunity in Depressed Adolescents: Results From a Clinical Cross-Sectional Study in Comparison to the General Pediatric Population. The Journal of Clinical Psychiatry, 82(2), 27973. https://doi.org/10.4088/JCP.20M13511
Shahid, M. A., Ashraf, M. A., & Sharma, S. (2022). Physiology, Thyroid Hormone. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK500006/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
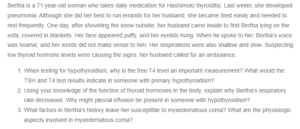
Disorders of Endocrine Control of Growth and Metabolism
Bertha is a 71-year-old woman who takes daily medication for Hashimoto thyroiditis. Last winter, she developed pneumonia. Although she did her best to run errands for her husband, she became tired easily and needed to rest frequently. One day, after shoveling the snow outside, her husband came inside to find Bertha lying on the sofa, covered in blankets. Her face appeared puffy, and her eyelids hung. When he spoke to her, Bertha’s voice was hoarse, and her words did not make sense to him. Her respirations were also shallow and slow. Suspecting low thyroid hormone levels were causing the signs, her husband called for an ambulance.
- When testing for hypothyroidism, why is the free T4 level an important measurement? What would the TSH and T4 test results indicate in someone with primary hypothyroidism?
- Using your knowledge of the function of thyroid hormones in the body, explain why Bertha’s respiratory rate decreased. Why might pleural effusion be present in someone with hypothyroidism?
- What factors in Bertha’s history leave her susceptible to myxedematous coma? What are the physiologic aspects involved in myxedematous coma?