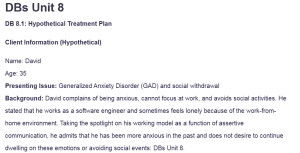
DBs Unit 8
DB 8.1: Hypothetical Treatment Plan
Client Information (Hypothetical)
Name: David
Age: 35
Presenting Issue: Generalized Anxiety Disorder (GAD) and social withdrawal
Background: David complains of being anxious, cannot focus at work, and avoids social activities. He stated that he works as a software engineer and sometimes feels lonely because of the work-from-home environment. Taking the spotlight on his working model as a function of assertive communication, he admits that he has been more anxious in the past and does not desire to continue dwelling on these emotions or avoiding social events: DBs Unit 8.
Goal: David will improve emotional regulation and increase social engagement.
Objective 1: David will develop coping strategies for managing anxiety
- Intervention 1. a: David will learn and practice mindfulness techniques, such as deep breathing and progressive muscle relaxation, for 10 minutes daily.
- Intervention 1.b: David will track his anxiety triggers and document his emotional responses in a journal for two weeks.
- Intervention 1.c: Using the cognitive behavioral therapy methods, David will be able to challenge and re-attribute the negative cognition implicated in anxiety. (Curtiss et al., 2021).
- Intervention 1.d: David will undergo exposure therapy in a structured manner through exposure to threatening stimuli.
Objective 2: David will build and maintain a support system
- Intervention 2. a: David will identify at least one friend or family member to connect with weekly via phone or video chat.
- Intervention 2.b: David will explore and join at least one online or in-person interest-based group within the next month.
- Intervention 2.c: David will participate in role-playing exercises to practice initiating conversations in social settings.
Objective 3: David will establish a structured self-care routine
- Intervention 3. a: David will set a consistent sleep schedule and aim for at least 7 hours per night.
- Intervention 3.b: David will engage in physical activity for at least 30 minutes three times per week to reduce stress.
- Intervention 3.c: David will reduce caffeine intake and track the effects of diet on his anxiety symptoms.
- Intervention 3.d: David will schedule monthly check-ins with a mental health professional to assess progress (Chia et al., 2023).
Reflection on the Treatment Planning Process
Designing this treatment plan meant that David’s specific deficits and motivation to change had to be considered significantly. It was necessary to develop specific goals that are under empirically supported strategies for dealing with anxiety. What I liked about the plan was that the goals were specific and divided into smaller tasks that made me feel that it was more doable. This process helped reshape my perception of the importance of personalized therapy and the feasibility of the implemented interventions (Wright et al., 2022).
References
Chia, F., Huang, W.-Y., Huang, H., & Wu, C.-E. (2023). Promoting healthy behaviors in older adults to optimize health-promoting lifestyle: An intervention study. International Journal of Environmental Research and Public Health, 20(2), 1628. https://doi.org/10.3390/ijerph20021628
Curtiss, J. E., Levine, D. S., Ander, I., & Baker, A. W. (2021). Cognitive-behavioral treatments for anxiety and stress-related disorders. Focus, 19(2), 184–189. https://doi.org/10.1176/appi.focus.20200045
Wright, B., Tindall, L., Scott, A. J., Lee, E., Biggs, K., Cooper, C., Bee, P., Wang, H.-I., Gega, L., Hayward, E., Solaiman, K., Teare, M. D., Davis, T., Lovell, K., Wilson, J., McMillan, D., Barr, A., Edwards, H., Lomas, J., & Turtle, C. (2022). One-session treatment compared with multisession CBT in children aged 7–16 years with specific phobias: the ASPECT non-inferiority RCT. Health Technology Assessment, 26(42), 1–174. https://doi.org/10.3310/ibct0609
DB 8.2: Determinants of Relapse
Relapse is a significant concern in addiction and mental health recovery. Three key determinants that I believe are most likely to contribute to relapse include emotional triggers, social influences, and lack of coping skills.
Environmental Determinants
Factors such as family, social circle, workplace, or any place that increases the likelihood of use of substances or relapse situation can greatly influence relapse. Activating ecological contexts of substance use and spending time with friends who still use substances will also cause cravings. For instance, an identified patient with alcohol addiction going to a family function where there is the same substance is likely to be challenged and give in and take a drink again (Kabisa et al., 2021).
Behavioral Determinants
In this case, if a person does not establish healthy ways of handling stress, it is likely he or she might revert back to previous habits. Continuing on the same lifestyle patterns and practices that were associated with drug use, such as visiting places where the person used to use drugs or associating with people who use, will put the person at a higher risk of relapse. For instance, an adult child who had a heroin addiction problem for several years would easily turn to drugs again if he or she continued to associate with former friends (Stevens & Smith, 2018).
Cognitive Determinants
Beliefs that one can have “just one drink” or the notion that using once is not dangerous are some of the primary relapse precipitants. These irrational beliefs can dampen the spirits and, therefore, cause the individual to lose his/her resolve to quit taking alcohol. For instance, an ex-drunk may think that he needs to take alcohol because he had a tiring day; this leads to relapse (Lima et al., 2022). Therapeutic management, adoption of healthy coping mechanisms, and managing the triggers are the keys to preventing relapse.
Conclusion
Knowledge of these determinants ensures that suitable intervention measures are applied, such as skilled management of feelings and impulses, people support, and rational behavioral approaches. Thus, it is imperative for those in recovery to try to understand and manage these factors if they seek to avoid relapse.
References
Kabisa, E., Biracyaza, E., Habagusenga, J. d’Amour, & Umubyeyi, A. (2021). Determinants and prevalence of relapse among patients with substance use disorders: Case of Icyizere Psychotherapeutic Centre. Substance Abuse Treatment, Prevention, and Policy, 16(1), 1–12. https://doi.org/10.1186/s13011-021-00347-0
Lima, R. A., Soares, F. C., van Poppel, M., Savinainen, S., Mäntyselkä, A., Haapala, E. A., & Lakka, T. (2022). Determinants of cognitive performance in children and adolescents: A populational longitudinal study. International Journal of Environmental Research and Public Health, 19(15), 8955. https://doi.org/10.3390/ijerph19158955
Stevens, P. W., & Smith, R. L. (2018). Substance use counseling: Theory and practice (6th ed.). Pearson.
DB 8.3: Models of Relapse Prevention
Three primary models of relapse prevention—the Disease Model, Developmental Models, and Cognitive-Behavioural/Social Learning Model—offer different perspectives on why relapse occurs and how it should be managed.
Disease Model
The Disease Model conceptualizes addiction as a chronic, progressive condition similar to diabetes or heart disease (Heilig et al., 2021). According to this model, people with addiction have a baseline, so relapse is considered a part of the disease progression. Relapse is managed in this perspective through continuous treatment, 12-step programs, and complete abstinence.
Example. Medical and peer support, such as that provided by Alcoholics Anonymous (AA), would be the main interventions that a human service provider implementing this model would use when treating clients to manage their condition.
Developmental Models
Developmental models view relapse through a lifespan perspective, suggesting that individuals experience different vulnerabilities at different stages of life. Some of the factors that influence the rates of relapse include childhood trauma, transitional phases within the life cycle, and changing roles. These areas are crucial in the developmental model as they focus on achieving certain milestones and developing resilience (Stevens & Smith, 2018). For instance, a provider implementing this model could assist a young adult in recovery by addressing stress related to securing new employment or living independently.
Cognitive-Behavioral/Social Learning Model
This model posits that relapse is a learned behavior that can be prevented through skill-building and cognitive restructuring (Larimer et al., 2024). In portraying the relapse process, it focuses on self-efficiency, strategies, and the environmental cues that lead to relapse. Relapse is posed as a high-risk event in which an individual lacks the necessary coping mechanisms. An example of such a provider utilizing this model can be to employ cognitive-behavioral therapy (CBT) to assist clients in identifying high-risk triggers and responding to them differently to avoid relapse.
Conclusion
The success rate of all the models is very high in preventing the relapse of substance abuse. The Disease Model focuses on abstaining from using drugs and seeking medical help, the Developmental Model takes into account age, developmental issues, and other pressures, and the Cognitive-Behavioral Model is based on learning skills. A relapse prevention plan may contain aspects from all three models as an ideal framework for an extended recovery timeline.
References
Heilig, M., MacKillop, J., Martinez, D., Rehm, J., Leggio, L., & Vanderschuren, L. J. M. J. (2021). Addiction as a brain disease revised: Why it still matters, and the need for consilience. Neuropsychopharmacology, 46(46), 1–9. https://doi.org/10.1038/s41386-020-00950-y
Larimer, M. E., Palmer, R. S., & Marlatt, G. A. (2024). Relapse prevention: An overview of marlatt’s cognitive-behavioral model. Alcohol Research & Health, 23(2), 151. https://pmc.ncbi.nlm.nih.gov/articles/PMC6760427/
Stevens, P. W., & Smith, R. L. (2018). Substance use counseling: Theory and practice (6th ed.). Pearson.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
DB 8.1
Developing a comprehensive treatment plan is an extensive process. Each treatment setting has a different format and requirements of what should be included for meeting the agency’s needs. As demonstrated in your readings, a great deal of specific information is required. In looking at the samples provided in your reading, please build your own hypothetical using the same model below.
Please develop your own and do not replicate the information below related to Susan used in the example. Think of your own goals, objectives, and interventions that could be used. Give it your best try based on the reading. Please also share how this process was for you after completing your treatment plan.
Goal: Susan will enjoy positive mood.
Objective 1. Susan will increase her social network.
Intervention 1.a. Susan will identify at least one acquaintance with whom she would be willing to initiate some form of social contact.
Intervention 1.b. Through role-plays, visualizations, and cognitive reframing, Susan will develop the confidence to initiate social contact with at least one identified person.
Intervention 1.c. Susan will explore social groups in her area and identify those which she would consider joining.
Intervention 1.d. Susan will examine negative self-messages that inhibit her from joining groups.
Objective 2. Susan will decrease her alcohol consumption.
Intervention 2.a. Susan will identify behaviors that contribute to increased alcohol consumption, including the identification of evening activities that do not allow for alcohol use.
Objective 3. Susan will exercise at least three times per week.
Intervention 3.a. Susan will identify physical activities she has enjoyed in the past.
Intervention 3.b. Susan will identify at least one person she feels would be interested in joining her in some form of physical activity.
Intervention 3.c. Through role-plays, visualizations, and cognitive strategies, Susan will develop the confidence to ask at least one identified person to join her in some physical activity.
Intervention 3.d. Susan will consult with her primary care provider (PCP) regarding her overall health before beginning an exercise program.
Objective 4. Susan will learn to manage depressive symptoms.
Intervention 4.a. Susan will read psychoeducational material regarding depression and its management.
Intervention 4.b. Susan will consult with her physician regarding her identified symptoms of depression.
Intervention 4.c. Susan will explore the pros and cons of talking about her experiences of loss and their relationship to her depression.
NOTE: You must make at least 1 substantial posting answering the topic above in addition to 2 substantial replies. In order to qualify for a grade over a 79 for this discussion topic, you should have at least 1 contribution by Wed. at midnight for this specific topic. You must participate in this discussion board forum (making postings/replies on all of the discussion boards for this unit) at least 3 days per unit. You also must use APA style in your postings and replies so please use in-text references and provide a reference to give proper credit to the authors.
DBs Unit 8
DB 8.2
- Your text discusses several determinants of relapse. Of those mentioned, please pick at least 3 and discuss why you believe that these determinants are “the most likely” in your opinion to contribute to relapse. Please provide your thoughts and examples in detail.
NOTE: You must make at least 1 substantial posting and 2 substantial replies to this thread. You must participate in the Unit discussion board (making postings/replies) at least 3 days per unit to qualify for full credit and also have at least 1 posting by Wednesday at midnight. You also must use APA style in your posting and replies so please use in-text references and provide a reference to give proper credit to the authors.
DB 8.3
- Your text discusses the Disease Model, Developmental Models, and Cognitive-Behavioral/Social Learning Model in thinking about relapse prevention. Please summarize each model briefly in your own words. How might a human service provider conceptualize relapse differently using each model? Please be sure to include your thoughts in your summary of each and provide examples.
NOTE: You must make at least 1 substantial posting and 2 substantial replies to this thread. You must participate in the Unit discussion board (making postings/replies) at least 3 days per unit to qualify for full credit and also have at least 1 posting by Wednesday at midnight. You also must use APA style in your posting and replies so please use in-text references and provide a reference to give proper credit to the authors.
Readings:
- Please read Stevens & Smith’s (2018) Chapter 6.
- Please read How to Develop a Treatment plan by clicking:
- Treatment Plan.docx (Attached)
- Please read Using the WDEP System by clicking: