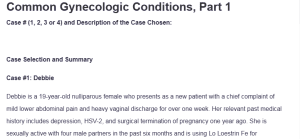
Common Gynecologic Conditions, Part 1
Case # (1, 2, 3 or 4) and Description of the Case Chosen:
Case Selection and Summary
Case #1: Debbie
Debbie is a 19-year-old nulliparous female who presents as a new patient with a chief complaint of mild lower abdominal pain and heavy vaginal discharge for over one week. Her relevant past medical history includes depression, HSV-2, and surgical termination of pregnancy one year ago. She is sexually active with four male partners in the past six months and is using Lo Loestrin Fe for contraception. The patient presents with a complaint of menarche at age nine with regular 28-day cycles that are seven days in duration and require three to four tampons daily: Common Gynecologic Conditions, Part 1.
She has never undergone cervical cancer screening, although she is sexually active. Her social history reveals that she lives with her parents, works as a full-time waitress, and denies alcohol, tobacco, or recreational drug use. Normal physical examination, aside from mucopurulent endocervical exudate, cervical friability, and mild cervical motion tenderness, are indicative of an infectious process that requires prompt evaluation and treatment. The picture is one of sexually transmitted cervicitis, which necessitates complete STI screening and prompt antibiotic therapy to prevent the development of pelvic inflammatory disease and future fertility problems.
| Outline Subjective data.
Identify data provided in your chosen case and any additional data needed. |
Outline
Objective findings.
Identify findings provided in your chosen case and any additional data needed. |
Identify diagnostic tests, procedures, laboratory work indicated.
Describe the rationale for each test or intervention with supporting references. |
Distinguish at least three differential diagnoses.
Describe the rationales for your choice of each diagnosis with supporting references. |
Identify appropriate medications, treatments or other interventions associated with each differential diagnosis.
Describe rationales and supporting references for each.
|
Explain key
Social Determinants of Heath (SDoH) for your chosen case. |
Describe collaborative care referrals and patient education needs for your chosen case.
Describe rationales and supporting references for each.
|
| The subjective data reveals a 19-year-old female presenting with mild lower abdominal pain and copious vaginal discharge lasting over one week.
Her sexual history is significant for multiple partners (four in six months) without documented STI screening. Previous medical history includes depression managed with unknown medications, confirmed HSV-2 diagnosis, and surgical pregnancy termination one year ago. She has never received cervical cancer screening despite being sexually active. Current contraceptive use includes Lo Loestrin Fe since her pregnancy termination. The patient denies alcohol, tobacco, or recreational drug use and works full-time as a waitress while living with her parents. Her last menstrual period was two weeks prior and reported as normal. |
Physical examination findings include normal vital signs with a BMI of 18.9 kg/m². The patient appears well-developed and well-nourished in no acute distress.
Abdominal examination reveals a soft, non-tender abdomen without masses or hepatosplenomegaly. Gynecological examination demonstrates no external lesions or erythema, however, mucopurulent endocervical exudate is visible within the endocervical canal. The cervix appears friable upon examination, and mild cervical motion tenderness is present. Notably, there is no uterine tenderness, adnexal tenderness, or palpable masses, which helps differentiate from more severe pelvic inflammatory conditions. |
Essential diagnostic testing includes nucleic acid amplification testing (NAAT) for Chlamydia trachomatis and Neisseria gonorrhoeae from the endocervical specimen obtained during examination (Workowski et al., 2021).
Additional STI screening should encompass syphilis serology (RPR or VDRL), HIV testing, and hepatitis B surface antigen, given her high-risk sexual behavior. Wet mount microscopy and KOH preparation of vaginal discharge should be performed to evaluate for bacterial vaginosis, trichomoniasis, and candidiasis. Complete blood count with differential may be indicated if systemic infection is suspected. Pregnancy testing should be conducted despite recent normal menses and current contraceptive use. Cervical cytology (Pap smear) is recommended given her age and sexual activity history, though treatment should not be delayed pending results (Schuiling & Likis, 2022). |
Chlamydial Cervicitis:
The primary differential diagnosis is chlamydial cervicitis, supported by mucopurulent discharge, cervical friability, and mild cervical motion tenderness in a sexually active young woman with multiple partners. Gonococcal Cervicitis: Secondary consideration includes gonococcal cervicitis, which presents similarly and often co-occurs with chlamydial infection. Pelvic Inflammatory Disease (PID): The third differential diagnosis encompasses pelvic inflammatory disease (PID), though the absence of significant uterine or adnexal tenderness makes this less likely but still possible, given the cervical motion tenderness and risk factors present. |
Chlamydial Cervicitis:
For suspected chlamydial cervicitis, first-line treatment includes azithromycin 1g orally as a single dose or doxycycline 100mg orally twice daily for seven days, with azithromycin preferred for compliance concerns (Centers for Disease Control and Prevention, 2021). Gonococcal Cervicitis: If gonococcal infection is suspected or confirmed, treatment requires ceftriaxone 250mg intramuscularly as a single dose plus azithromycin 1g orally for dual therapy addressing potential resistance patterns. Pelvic Inflammatory Disease (PID): For confirmed or suspected PID, outpatient treatment includes ceftriaxone 250mg IM plus doxycycline 100mg orally twice daily for 14 days with metronidazole 500mg orally twice daily for 14 days to cover anaerobic organisms (Workowski et al., 2021). Partner notification and treatment are essential for all sexually transmitted infections to prevent reinfection and transmission. |
Social determinants significantly impacting Debbie’s health include her young age and potential lack of comprehensive sexual health education, evidenced by multiple sexual partners without consistent STI screening (Fanslow et al., 2019).
Her employment as a waitress may indicate lower socioeconomic status, potentially affecting healthcare access and health literacy. Living with her parents at age 19 while working full-time also suggests financial constraints that may impact her ability to access regular healthcare services. Her history of depression may influence health-seeking behaviors and medication compliance. The absence of higher education (not attending college) may correlate with limited health knowledge and resources. Geographic factors and transportation access from her work schedule could create barriers to follow-up care and partner notification processes. |
Collaborative care should include referral to a mental health provider for depression management, particularly given the potential psychosocial impact of STI diagnosis and sexual health concerns.
Partner services coordination through local health department resources is essential for contact tracing and treatment of sexual partners to prevent reinfection cycles. Patient education must emphasize proper medication compliance, including completion of full antibiotic courses, even if symptoms resolve early. Comprehensive safer sex counseling should address consistent condom use, regular STI screening recommendations, and discussion about reducing the number of concurrent sexual partners (Lockwood, 2019). Schedule a follow-up appointment in one week to assess treatment response and ensure symptom resolution. Provide written information about her STI diagnosis, treatment, and prevention strategies. Discuss the importance of routine gynecological care, including annual cervical cancer screening and contraceptive counseling, to ensure optimal reproductive health outcomes. |
References
Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines, 2021. MMWR Recommendations and Reports, 70(4), 1-187. https://www.cdc.gov/mmwr/volumes/70/rr/rr7004a1.htm
Curry, S. J., Krist, A. H., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., … & US Preventive Services Task Force. (2018). Screening for sexually transmitted infections: US Preventive Services Task Force recommendation statement. JAMA, 320(16), 1678-1687. https://jamanetwork.com/journals/jama/fullarticle/2697704
Schuiling, K. D., & Likis, F. E. (2022). Gynecologic health care (4th ed.). Jones and Bartlett Learning.
Workowski, K. A., Bachmann, L. H., Chan, P. A., Johnston, C. M., Muzny, C. A., Park, I., … & Webber, J. J. (2021). Sexually transmitted infections treatment guidelines, 2021. MMWR Recommendations and Reports, 70(4), 1-187. https://pubmed.ncbi.nlm.nih.gov/34292926/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Common Gynecologic Conditions, Part 1
Case studies provide the opportunity to simulate realistic scenarios involving patients presenting with various health problems or symptoms. Such case studies enable nurse learners to apply concepts, lessons, and critical thinking to interviewing, screening, and diagnostic approaches, as well as to the development of treatment plans.
For this Case Study Assignment, you will once again choose 1 of 4 case study scenarios and review the case study scenario to obtain information related to a gynecologic exam and determine differential diagnoses, diagnostics, and develop treatment and management plans.
Resources
- Be sure to review the Learning Resources before completing this activity.
- Click the weekly resources link to access the resources.
Common Gynecologic Conditions, Part 1
To prepare:
- Review the 4 case studies in this week’s Learning Resources. Select one of the cases to prepare your written assignment.
- Review the Learning Resources for this week and specifically review the clinical guideline resources specific to your chosen case study.
Assignment Instructions:
- Use the Case Study Template from the Learning Resources to complete the assignment. Your submission must include a brief case write-up, followed by the fully completed template, which must be integrated into the document rather than submitted separately.
- Include a title page, a case summary in your own words, the completed template, and a reference page formatted in APA style.
NOTES:
- This is a case study assignment. The instruction requires selecting one of the four case studies and developing a workup using the attached template.
- Please see the attached Grading rubric outlining how the points will be awarded