Case Study Analysis – Acute Streptococcal Pharyngitis
In this case study, Susan, a 16-year-old patient, presents with severe sore throat, fever, dysphagia, and visible white spots on her throat. She reports no cough and rhinorrhea. Her physical examination reveals tender cervical lymphadenopathy and tonsillar exudates. These symptoms, along with physical exam findings, are in line with bacterial etiology, especially streptococcal pharyngitis. This paper explores the possible cause of these symptoms, discusses the supporting diagnostic data, suggests the appropriate test, and formulates an effective treatment plan for Susan’s case to assist her and mitigate further transmission.
Most Likely Diagnosis and Pathogen
From the symptoms reported by the patient, together with the clinical findings from the physical exam, the most likely diagnosis is acute streptococcal pharyngitis (strep throat) predominantly caused by Group A Streptococcus (GAS), a gram-positive bacteria pathogen known to cause strep throat in adolescents and young adults. The primary transmission mode of pharyngitis revolves around respiratory contact, especially with an infected person. For instance, respiratory droplets released in the air when an infected person coughs, talks, or sneezes are inhaled. Secondly, transmission through contact with contaminated surfaces and then touching the mouth or nose. However, in this case, Susan denies exposure or contact with infected people; nonetheless, it is important to appreciate the asymptomatic carriers who might present with no noticeable signs and symptoms but are capable of transmitting the infection.
Data Supporting the Diagnosis
Clinical presentations and findings substantiate the choice of acute streptococcal pharyngitis as the diagnosis. To begin with, severe pain when swallowing is the hallmark of streptococcal pharyngitis as a result of tonsillar and pharyngeal tissue inflammation. Secondly, the white exudate on the tonsils serves as a clinical sign of streptococcal pharyngitis, which differentiates it from other possible diagnoses, such as a viral infection and common cold. Thirdly, the small petechiae are common findings in patients with bacterial infections like the GAS. The fourth point in support of strep throat as the diagnosis is the absence of coughing and rhinorrhea, which are present in other respiratory infections but are absent in strep throat. Fifthly, the severe sudden onset accompanied by fever is a characteristic of bacterial infections, unlike viral, which have a gradual onset. In addition to these points, the tender, enlarged anterior cervical lymph nodes are classical features of strep throat that stem from the inflammation of the nodes in response to bacterial infection (Ashurst & Edgerley-Gibb, 2023).
Diagnostic Testing
To ascertain the diagnosis, it is advisable to do a rapid antigen test using a throat swab, which detects the antigens from Group A streptococcus. A positive test confirms the diagnosis. Alternatively, a throat culture may be done, though the results may take 24-48 hours (Mustafa & Ghaffari, 2020).
Treatment Plan
The primary goals that guide the treatment plan involve curing the condition, preventing complications, preventing transmission, and improving the quality of life. My suggested treatment approach involves the use of first-line drugs such as penicillin v or Amoxicillin, which should be taken 500mg twice daily for ten days. Alternatively, a single dose of intramuscular penicillin G benzathine might be used. For cases where the patient has allergies to penicillin, unlike for Susan, cephalosporin and macrolides might be used as effective drugs. Secondly, pain and fever management are key priorities in this treatment plan. To serve this purpose, ibuprofen 200-400 mg or acetaminophen 500 mg can be used to reduce pain, fever, and inflammation. Thirdly, the patient should be taught proper fluid intake to prevent dehydration secondary to fever, as well as rest to facilitate recovery (Mustafa & Ghaffari, 2020). Also, teach the patient to do warm salt water gargles that may reduce symptoms. Lastly, isolation at home should be encouraged for at least 24 hours post antibiotic therapy, and good hygiene practices should be implemented, such as covering up the mouth when coughing, avoiding sharing utensils, and observing hand hygiene to prevent further transmission. Re-evaluation should be done after 48 hours to assess for improvement of the symptoms and rule out resistance and possible complications (Mustafa & Ghaffari, 2020).
References
Ashurst, J. V., & Edgerley-Gibb, L. (2023). Streptococcal pharyngitis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK525997/
Mustafa, Z., & Ghaffari, M. (2020). Diagnostic methods, clinical guidelines, and antibiotic treatment for group A streptococcal pharyngitis: A narrative review. Frontiers in Cellular and Infection Microbiology, 10(10). https://doi.org/10.3389/fcimb.2020.563627
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Case 1
Review the pharyngitis scenarios and determine the most likely cause, including pathogen and mode of transmission. Discuss data that support your decision and treatment strategies.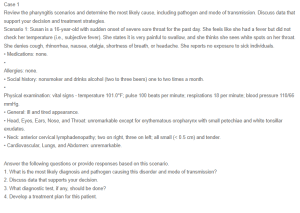
Scenario 1: Susan is a 16-year-old with sudden onset of severe sore throat for the past day. She feels like she had a fever but did not check her temperature (i.e., subjective fever). She states it is very painful to swallow, and she thinks she sees white spots on her throat. She denies cough, rhinorrhea, nausea, otalgia, shortness of breath, or headache. She reports no exposure to sick individuals.
• Medications: none.
•
Allergies: none.
• Social history: nonsmoker and drinks alcohol (two to three beers) one to two times a month.
•
Physical examination: vital signs – temperature 101.0°F; pulse 100 beats per minute; respirations 18 per minute; blood pressure 110/66 mmHg.
• General: ill and tired appearance.
• Head, Eyes, Ears, Nose, and Throat: unremarkable except for erythematous oropharynx with small petechiae and white tonsillar exudates.
• Neck: anterior cervical lymphadenopathy; two on right, three on left; all small (< 0.5 cm) and tender.
• Cardiovascular, Lungs, and Abdomen: unremarkable.
Answer the following questions or provide responses based on this scenario.
1. What is the most likely diagnosis and pathogen causing this disorder and mode of transmission?
2. Discuss data that supports your decision.
3. What diagnostic test, if any, should be done?
4. Develop a treatment plan for this patient.