Autism Spectrum Disorder (ASD)
Autism spectrum disorder (ASD) is a neurodevelopmental condition defined by deficit in interaction and social communication and stereotyped and repetitive patterns of behavior, interest, or activities (American Psychiatric Association, 2022). Symptoms must occur early in the developmental stages, leading to clinically substantial deficits in social, occupational, or other relevant aspects of the person’s life.
Signs and Symptoms According to DSM-IV
The signs and symptoms of ASD are broadly classified into two broad classes: deficits in social communication and restricted and repetitive behaviors.
Social Communication Deficits
These are as follows:
- Deficits in social-emotional reciprocity
- Deficits in nonverbal communication
- Deficits in developing, maintaining, and understanding relationships
Restricted and Repetitive Behaviors
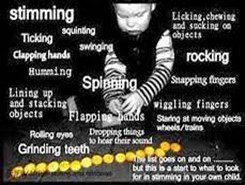
These are:
- Stereotyped or repetitive movements.
- Insistence on sameness; inflexible routines.
- Highly restricted, fixated interests.
- Hyper- or hypo reactivity to sensory input.
Restricted and repetitive behaviors symptoms can be simplified with the mnemonic “SIRI”:
- Stereotyped movements
- Insistence on sameness
- Restricted interests
- Input sensitivity (sensory)
Differential Diagnosis
ASD has numerous differential diagnoses. Below, the table summarizes the most common differential diagnoses.
| Differential diagnoses | Similarities to ASD | Differences from ASD
|
| Social (Pragmatic) Communication Disorder (SCD) | Both SCD and ASD involve deficits in social communication and interaction. | Unlike ASD, there are no restricted or repetitive behaviors present in SCD. |
| Attention-Deficit/Hyperactivity Disorder (ADHD) | Both conditions may present with attention difficulties, impulsivity, and social challenges. | Patients with ADHD do not have restricted interests and repetitive behaviors, which are present in ASD patients. |
| Specific Learning Disorder (SLD) | Both conditions can present academic challenges and require educational interventions. | SLD affects specific academic skills, for example, reading, while ASD involves broader deficits in communication and behavior. |
| Schizophrenia of childhood-onset | Both conditions may present unusual behaviors such as flat affect and social detachment. | While Schizophrenia typically presents with hallucinations and delusions, ASD does not. |
Incidence
ASD approximately affect 1 out of 36 children in the United States (USA), making it one of the most prevalent neurodevelopmental condition. This condition affects Boys more than girls (Napolitano et al., 2022). The incidence has also increased gradually, mainly due to increased awareness, better diagnostic methods, and improved screening programs. These factors have led to increased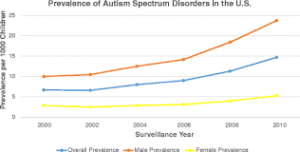 interventions and identification of the condition at an earlier age and across different population groups.
interventions and identification of the condition at an earlier age and across different population groups.
Development and Course
The first clinical manifestations of ASD are usually seen from 18 to 24 months of age, but often, the child is diagnosed at the age of three years and above (Okoye et al., 2023). Some signs and symptoms that may be noticeable at this age include the child avoiding eye contact, not speaking as early as other children, and poor facial expressions, such as smiling. The development process may be marked by considerable variability, and there is evidence that with early, intensive intervention, some progress can be seen during the early years. However, ASD is a life-long disability, and the level of progress highly depends on the timing and quality of intervention.
Prognosis
The prognosis of ASD depends on early intervention measures, cognitive functioning, and having functional speech by five years of age. Children treated early for their behavioral and educational issues are likely to have a better prognosis regarding their autonomy and socialization (Vinen et al., 2022). However, functional outcomes may differ from relatively independent living to totally dependent care for the rest of life. Despite these improvements, most ASD patients face considerable difficulties in social communication and the development of adaptive skills throughout their adulthood.
Culture, Gender, and Age Considerations in ASD
Cultural and socioeconomic differences make minorities get diagnosed with ASD less frequently than other population groups for several reasons, which include limited services, language barriers, and prejudice towards mental health. Another factor is that girls are often less present with the symptoms of autism, and thus, their diagnosis may be delayed or even absent. Also, females tend to hide their symptoms than males, making diagnosis difficult (Estrin et al., 2020). The symptoms are generally apparent at an early age. Still, severe disability is likely not to present until the child is faced with additional social and academic requirements as they progress through childhood.
Pharmacological Management
The pharmacological management of ASD aims to manage symptoms (Maniram et al., 2023). These medications and their side effects are presented in the table below.
| Symptom | Medication | Medication Class | Side effects |
| Irritability and aggression | Risperidone and, Aripiprazole | Second generation antipsychotics | Weight gain and sedation effect. |
| Hyperactivity | Methylphenidate | central nervous system stimulant | Anorexia and insomnia |
| Anxiety | Fluoxetine | selective serotonin reuptake inhibitor | Insomnia and nausea |
Nonpharmacological Management
- Speech and Language Therapy: enhances verbal and non-verbal skills.
- Occupational Therapy: Supports sensory integration and daily skills.
- Applied behavior analysis: to improve behaviors and skills (Gitimoghaddam et al., 2022).
- Parent Training Programs: it promotes consistency in behavior strategies.
- Social Skills Training: Group or individual sessions for peer interaction.
These management strategies can be simplified using the Mnemonic “SOAPS”:
- Speech and language therapy
- Occupational therapy
- Applied behavior analysis therapy
- Parent training
- Social Skills Training
Diagnostics and Labs
Autism spectrum disorder cannot be diagnosed by using any lab test. Instead, diagnosis is made through clinical diagnosis. In diagnosing social communication and behavior patterns, the Autism Diagnostic Observation Schedule (ADOS-2) and the Autism Diagnostic Interview-Revised (ADI-R) are typically utilized by healthcare providers (Lefort-Besnard et al., 2020). Screening tools like the Modified Checklist for Autism in Toddlers (M-CHAT) are initially used in primary care physician practices to identify children at risk.
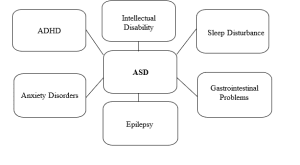
Comorbidities
Common Comorbidities of ASD include:
Legal and Ethical Considerations
- Individuals with Disabilities Education Act (IDEA) – It instructs for special education services (Ojeda & Carugno, 2022).
- Americans with Disabilities Act and Section 504 of the Rehabilitation Act: Ensures accommodations in schools and workplaces.
Pertinent Patient Education Considerations
For Parents:
- Educate on the importance of early interventions
- Encourage the use of visual support aids and structuring play environment
For Individuals with ASD:
- Promote independence through routines
- Develop self-advocacy skills
For Educators:
- Use structured environments and visual schedules
- Provide sensory accommodations
References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (DSM-5-TR). Psychiatry.org; American Psychiatric Association. https://www.psychiatry.org/psychiatrists/practice/dsm
Estrin, G. L., Milner, V., Spain, D., Happé, F., & Colvert, E. (2020). Barriers to autism spectrum disorder diagnosis for young women and girls: A systematic review. Review Journal of Autism and Developmental Disorders, 8(4), 454–470. https://doi.org/10.1007/s40489-020-00225-8
Gitimoghaddam, M., Chichkine, N., McArthur, L., Sangha, S. S., & Symington, V. (2022). Applied behavior analysis in children and youth with autism spectrum disorders: A scoping review. Perspectives on Behavior Science, 45(3), 521–557. https://doi.org/10.1007/s40614-022-00338-x
Lefort-Besnard, J., Vogeley, K., Schilbach, L., Varoquaux, G., Thirion, B., Dumas, G., & Bzdok, D. (2020). Patterns of autism symptoms: Hidden structure in the ADOS and ADI-R instruments. Translational Psychiatry, 10(1). https://doi.org/10.1038/s41398-020-00946-8
Maniram, J., Oosthuizen, F., & Karrim, S. B. (2023). An overview of pharmacotherapy in the management of children with autism spectrum disorder at a public hospital in KwaZulu-Natal. Child Psychiatry & Human Development, 55(6), 1655–1663. https://doi.org/10.1007/s10578-023-01514-z
Napolitano, A., Schiavi, S., La Rosa, P., Rossi-Espagnet, M. C., Petrillo, S., Bottino, F., Tagliente, E., Longo, D., Lupi, E., Casula, L., Valeri, G., Piemonte, F., Trezza, V., & Vicari, S. (2022). Sex differences in autism spectrum disorder: Diagnostic, neurobiological, and behavioral features. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.889636
Ojeda, A. B. B., & Carugno, P. (2022, September 18). Special education. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499857/
Okoye, C., Obialo-Ibeawuchi, C. M., Obajeun, O. A., Sarwar, S., Tawfik, C., Waleed, M. S., Wasim, A. U., Mohamoud, I., Afolayan, A. Y., & Mbaezue, R. N. (2023). Early diagnosis of autism spectrum disorder: A review and analysis of the risks and benefits. Cureus, 15(8). https://doi.org/10.7759/cureus.43226
Vinen, Z., Clark, M., & Dissanayake, C. (2022). Social and behavioural outcomes of school aged autistic children who received community-based early interventions. Journal of Autism and Developmental Disorders, 53(5), 1809–1820. https://doi.org/10.1007/s10803-022-05477-3
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Autism Spectrum Disorder (ASD)
Welcome to Week 8, this week you will create a study guide. You have been assigned a specific neurodevelopmental disorder by your last name.
Autism Spectrum Disorder (ASD)
Create a study guide for your assigned disorder. Your study guide should be in the form of an outline with references, and you should incorporate visual elements such as concept maps, charts, diagrams, images, color coding, mnemonics, and/or flashcards. Be creative! It should not be in the format of an APA paper. Your guide should be informed by the DSM-5 but also supported by at least three other scholarly resources.
Last names begin with the letter’s I-J
Autism spectrum disorder