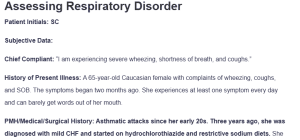
Assessing Respiratory Disorder
Patient Initials: SC
Subjective Data:
Chief Compliant: “I am experiencing severe wheezing, shortness of breath, and coughs.”
History of Present Illness: A 65-year-old Caucasian female with complaints of wheezing, coughs, and SOB. The symptoms began two months ago. She experiences at least one symptom every day and can barely get words out of her mouth.
PMH/Medical/Surgical History: Asthmatic attacks since her early 20s. Three years ago, she was diagnosed with mild CHF and started on hydrochlorothiazide and restrictive sodium diets. She has been on enalapril since last year to manage her worsening CHF. The patient had a motor vehicle accident ten weeks ago. Two weeks after the accident, she experienced post-traumatic seizure and was placed on phenytoin. There have been no reports of convulsions since. The patient has never had any surgeries.
Significant Family History: Father died of kidney failure secondary to hypertension at 59. Mother died at 62 of CHF.
Social History: Negative history of smoking or alcohol use. Uses 4 cups of coffee and 4 diet colas every day.
- Medication List:
- Theophylline SR Capsules 300 mg PO BID
- Albuterol inhaler, PRN
- Phenytoin SR capsules 300 mg PO QHS
- HTCZ 50 mg PO BID
- Enalapril 5 mg PO BID
Review of Symptoms:
General: Reports weight gain. Denies fever or chills.
Integumentary: Denies any skin color changes, lesions, or scars.
Head: Denies any head swelling, lesions, or scars.
Eyes: Denies visual loss, discharge, or eye swelling.
ENT: Denies hearing loss, nasal discharge, or difficulty swallowing.
Cardiovascular: Positive for occasional edema and palpitations.
Respiratory: Positive for SOB, coughing, wheezing, and exercise intolerance.
Swelling in the extremities and seizures.
Gastrointestinal: Reports bloating. Denies irregular bowel movements.
Genitourinary: Positive for frequent urination. Denies dysuria.
Musculoskeletal: Denies muscle pain or joint stiffness.
Neurological: Denies headache.
Endocrine: Denies heat or cold intolerance.
Hematologic: Denies ease of bruising or anemia.
Psychologic: Denies depression or anxiety.
Objective Data:
VS: BP 171/94, HR 122, RR 31, T 96.7 F, Wt 145, Ht 5’ 3”
VS after Albuterol breathing treatment – BP 134/79, HR 80, RR 18
Physical Assessment Findings:
HEENT: Pale, well-developed female. She appears anxious.
Lymph Nodes: No sign of lymph node swelling.
Carotids: Palpable bilatrelly.
Lungs: Bilateral expiratory wheezes.
Heart: Regular and rhythmic heart rate. Positive S1 and S2 sounds.
Abdomen: Soft, non-tender, non-distended on plapation. No abdominal masses.
Rectum: Guaiac negative.
Genital/Pelvic: Unremarkable.
Extremities/Pulses: +1 ankle edema on the right, no bruising, normal pulses.
Neurologic: A&O X3, cranial nerves intact.
Laboratory and Diagnostic Test Results:
- Na – 134 -normal
- K – 4.9 -Normal
- Cl – 100- Normal
- BUN – 21- Normal
- Cr – 1.2- Normal
- Glu – 110-Normal
- ALT – 24-Normal
- AST – 27 -Normal
- Total Chol – 190- Normal
- CBC – WNL
- Theophylline – 6.2
- Phenytoin – 17
- Chest Xray – Blunting of the right and left costophrenic angles
- Peak Flow – 75/min; after albuterol – 102/min
- FEV1 – 1.8 L; FVC 3.0 L, FEV1/FVC 60% (Moderate obstructive lung disease)
Assessment
Differential diagnoses:
- Acute asthmatic exacerbation ICD-10 code J45.901: The hallmark features of asthmatic exacerbation include shortness of breath with subsequent use of accessory muscle of respiration, inability to complete sentences in a single breath, respiratory rate of more than 30 bpm, pulse rate of more than 120 bpm, and a PEF of less than 50%, among known asthmatics (Kostakou et al., 2019). The presence of shortness of breath, a history of asthmatic attacks, a respiratory rate of more than 30 breaths per minute, an inability to complete sentences on a single breath, and a pulse rate of more than 120 bpm warranted this diagnosis.
- Asthma ICD-10 Code J45: The presence of wheezing, shortness of breath, and coughs, alongside a significant history of asthmatic attacks in the clinical case presented, warranted the inclusion of this differential (Ramsahai et al., 2019).
- Bronchiectasis ICD-10 Code J47.9: The presence of these manifestations made bronchiectasis a probable diagnosis.
Diagnosis: The presumptive diagnosis is acute exacerbation of asthma.
Plan of Care:
Diagnostics:
Pulse oximetry: This will help in determining the patient’s blood oxygen levels.
Treatment: The patient will then be nebulized with Albuterol ( dose of 2.5mg/2.5ml) and ipratropium bromide (dose of 0.5mg/2.5ml every 4 hours) while waiting for lab results. If the oxygen saturation is found to be below 88% on pulse oximetry, she will be started on oxygen therapy (Talbot et al., 2024).
Patient education: The patient will be educated on the disease process. She will be told of the environmental triggers of asthmatic attacks and asthma exacerbation and the available therapies. She will also be advised to adhere to the prescribed medication and avoid common triggers for the disease. She will also be told to monitor her symptoms regularly and report to the clinic whenever she notices any symptoms escalation.
Follow-up: The patient is expected to return for follow-up after one to two weeks based on symptoms manifestations. This will help caregivers assess whether the symptoms have been resolved.
References
Kostakou, E., Kaniaris, E., Filiou, E., Vasileiadis, I., Katsaounou, P., Tzortzaki, E., Koulouris, N., Koutsoukou, A., & Rovina, N. (2019). Acute severe asthma in adolescent and adult patients: Current perspectives on assessment and management. Journal of Clinical Medicine, 8(9), 1283. https://doi.org/10.3390/jcm8091283
Ramsahai, J. M., Hansbro, P. M., & Wark, P. A. (2019). Mechanisms and management of asthma exacerbations. American Journal of Respiratory and Critical Care Medicine, 199(4), 423–432. https://doi.org/10.1164/rccm.201810-1931ci
Talbot, T., Roe, T., & Dushianthan, A. (2024). Management of acute life-threatening asthma exacerbations in the intensive care unit. Applied Sciences, 14(2), 693. https://doi.org/10.3390/app14020693
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
SOAP Note Assignment
Click here to download and analyze the case study for this week. Create a SOAP note for disease prevention, health promotion, and acute care of the patient in the clinical case. Your care plan should be based on current evidence and nursing standards of care.
Visit the online library and research for current scholarly evidence (no older than 5 years) to support your nursing actions. In addition, consider visiting government sites such as the CDC, WHO, AHRQ, Healthy People 2020. Provide a detailed scientific rationale justifying the inclusion of this evidence in your plan.
Next determine the ICD-10 classification (diagnoses). The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD–10–CM) is the official system used in the United States to classify and assign codes to health conditions and related information.
Assessing Respiratory Disorder
Click here to access the codes.
Download the SOAP template to help you design a holistic patient care plan. Utilize the SOAP guidelines to assist you in creating your SOAP note and building your plan of care. You are expected to develop a comprehensive SOAP note based on the given assessment, diagnosis, and advanced nursing interventions. Reflect on what you have learned about care plans through independent research and peer discussions and incorporate the knowledge that you have gained into your patient’s care plan. If the information is not in the provided scenario please consider it normal for SOAP note purposes, if it is abnormal please utilize what you know about the disease process and write what you would expect in the subjective and objective areas of your note.
Format
• Your care plan should be formatted as a Microsoft Word document. Follow the current APA edition style. Your paper should be no longer than 3–4 pages excluding the title and the references and in 12pt font.