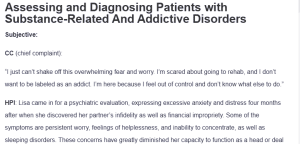
Assessing and Diagnosing Patients with Substance-Related And Addictive Disorders
Subjective:
CC (chief complaint):
“I just can’t shake off this overwhelming fear and worry. I’m scared about going to rehab, and I don’t want to be labeled as an addict. I’m here because I feel out of control and don’t know what else to do.”
HPI: Lisa came in for a psychiatric evaluation, expressing excessive anxiety and distress four months after when she discovered her partner’s infidelity as well as financial impropriety. Some of the symptoms are persistent worry, feelings of helplessness, and inability to concentrate, as well as sleeping disorders. These concerns have greatly diminished her capacity to function as a head or deal with day-to-day tasks and unheard and unmet relational needs. Lisa describes a continuous sense of being overwhelmed and fearful, particularly regarding the idea of entering rehabilitation and being labeled as an addict. She reports that these feelings persist throughout the day and are exacerbated by thoughts of her recent experiences and uncertainty about the future.
Past Psychiatric History
General Statement: Information and record collection documented that Lisa has never undergone any psychiatric treatment or mental health therapy. This is her first time to report any such form of discomfort, though she has not ever been to counseling or therapy in her lifetime. However, she has gone through other forms of hardships.
Caregivers: None
Hospitalizations: Denies any past hospitalization
Medication Trials: None
Psychotherapy or Previous Psychiatric Diagnosis: Denies having undergone psychotherapy and has no prior psychiatric history or diagnosis.
Substance Current Use and History: Admitted to drinking alcohol occasionally with her friends but denied taking other drugs, legal or illegal, including illicit drugs or nicotine
Family Psychiatric/Substance Use History: Lisa did not provide specific details about a family history of psychiatric disorders, substance use, or suicide. However, understanding any family history of mood disorders, anxiety, or substance use disorders could be helpful, as these conditions often have a genetic component (DNP, 2019). Additional inquiry into potential hereditary health issues may be beneficial for her treatment plan.
Psychosocial History: Lisa was raised by her parents. She recently broke up with her partner, Jeremy, due to his cheating and financial misconduct. He has a daughter called Sarah, and she is presently living with friends. The latest breakup has affected her emotionally; she struggles, worries, and feels lonely. Before these events, Lisa was able to manage her business effectively but is now unable to conduct everyday business. In her history, no legal problems, traumatic events, or violence are described.
Medical History:
Illnesses and Surgeries: None
Current Medications: Lisa is not on any prescribed medications, over-the-counter treatments, or homeopathic products. It is important to determine if she uses any supplements that may affect her psychological or physical health.
Allergies: Lisa has no known medication, food, or environmental allergies.
Review of Systems (ROS)
Here’s a more elaborated Review of Systems (ROS) section, providing detailed information under each category:
Review of Systems (ROS)
- GENERAL:
Lisa says she has felt considerably tired, and she blames it on stress emanating from a number of facets of life, including sleeplessness. She only mentions a continuously overwhelming feeling as to her parenting and her inability to maintain financial stability. Even though she says that she has not lost any weight in the last month, she complains of fatigue and lacks motivation to do things she used to do. - HEENT:
Lisa dismisses any ailment relating to headache, change of vision, or loss of hearing. She has no pain at all in the head and neck region, including nasal congestion, sinus pressure, or sore throat. Further, she has no rashes or even skin lesions/itching, which suggests she has no allergy/dermatologic issues. - SKIN:
There are no changes in the skin color or texture, which has prevented Lisa from experiencing any face bruising or cuts. She says her skin looks healthy and elastin, and she has not had recurrent dry skin or itching. - CARDIOVASCULAR:
Lisa says she has never had chest pain, pressure, or palpitations. She has no family or past history of arrhythmia or syncope–fainting spells. Moreover, she has no complaints of shortness of breath while performing her daily activities, and she is still a socially active lady who enjoys her life, meaning she has no symptomatic cardiovascular disease. - RESPIRATORY:
Regarding questions related to respiratory functions, Lisa said she had none. She does not complain of chronic cough, wheezing, or shortness of breath. There is no inflammation of respiratory tract infections, and she has not encountered any serious environmental factors that would compromise respiratory features. - GASTROINTESTINAL:
Lisa reports no alterations in her appetite, nausea, vomiting, diarrhea, or abdominal pain whatsoever. In the latest interview, the woman also mentioned that she does not experience changes in her bowel movement patterns. It is also interesting to note that there are no gastrointestinal complaints that may point to problems ranging from frequent GER to constipation. - GENITOURINARY:
She says she has no troubles with her urinary functions, with no dysuria or frequent or urgent urination. She says that she has a normal menstrual cycle, and there has not been any alteration in her menstrual cycle after giving birth to her daughter. - NEUROLOGICAL:
Despite the above symptoms, Lisa affirmatively responded that have not experienced dizziness, lightheadedness, or fainting spells. To date, there are no sensations of paresthesia/tingle or motor deficit in the limbs. She has never had any seizures or neurological disorders, and her mental status examination seems commendably normal, except she complains of sometimes having trouble focusing due to anxiety. - MUSCULOSKELETAL:
According to her, she does not have any swelling or pain affecting any of the joints or muscles or feel any stiffness. She complains of general tiredness, and while she may not explain it totally to depression or any psychosocial problem, she does not tend to relate it to musculoskeletal disorders. She had no injuries or surgeries to her musculoskeletal system, as can be evidenced by the information below. - HEMATOLOGIC:
At present, she has never been diagnosed with anemia; she has never suffered from such problems as frequent bruising or abnormal bleeding. She has not complained of any problems with her hea; lth regarding blood clotting or frequent infections. - LYMPHATICS:
Lymphadenopathy or other signs of infection are not observed in this case. Neither Lisa has had any lymphatic complications, nor is there a problem with systematic infections or inflammatory ailments. - ENDOCRINOLOGIC:
Lisa denies experiencing symptoms commonly associated with endocrine dysfunction, such as heat or cold intolerance, excessive sweating, or significant changes in appetite. She has not reported any menstrual irregularities that could suggest thyroid dysfunction.
Objective:
Diagnostic results: To extend differential diagnoses for signs in Lisa, laboratory tests and psychological assessments are the next feasible steps. These diagnostics will serve to exclude or confirm the presence of a somatic or a mental disorder that might be causing her emotional disorder.
Toxicology Screening: An alcohol use assessment, in addition to a toxicology screen, is advisable in order to try to determine other substances that may have affected Lisa’s mental health. This will assist in deciding the stage of her alcohol usage and assist in decision-making regarding her therapy.
Liver Function Tests (LFTs): Since alcohol affects the liver, conducting LFTs, that is, AST, ALT, and bilirubin levels, will help to determine the level of alcohol toxicity in the liver. The American Association for the Study of Liver Diseases points out that assessment of liver status is critical in patients with a history of alcohol and other substance use (DNP, 2019).
Depression and Anxiety Screening: The standardized screening checklists that can be used for assessing her severity of anxiety and depression include the Generalized Anxiety Disorder 7-item scale (GAD-7) and the Patient Health Questionnaire-9 (PHQ-9). They are among the most frequently used and endorsed instruments for evaluating mental health disorders in order to practice.
Assessment:
Mental Status Examination: Lisa appeared slightly disheveled and visibly distressed. She is anxious, her affect is appropriate, and she demonstrated symptoms of fear and sadness. Physical: The client’s speech is logical but halting, especially when discussing substance use. The reasoning is present. However, it is dominated by recent social and financial issues. She reports that she has never had symptoms of hallucinations, delusions, or thought disorders. It is also difficult to gain insight as she does not think that she has a problem with alcoholism since she drinks moderately. Stress and possible substance use render judgment questionable and compromise it.
Differential Diagnoses:
- Substance Use Disorder, Alcohol (ICD-10 Code: F10.20)
This diagnosis is evidenced by Lisa’s ongoing alcohol use, which she admits to engaging in occasionally with friends. However, evidence of substance issues can still be seen in her fear of rehab, her denial of her problem, and her overall constant alcohol consumption. Signs of preoccupation with a substance, the need to consume alcohol dependent on the presence of impairment and withdrawal symptoms, and the last sign of denial and applying scopophobia are the main features of an ailment of substance use disorder.
Rationale: Substance use disorder affects many individuals, particularly in response to life stressors, as seen in Lisa’s situation. She has been experiencing these symptoms for several months, indicating that the disorder is significant and likely has developed due to her emotional distress. The lack of withdrawal symptoms to this form of substance use makes it easy to diagnose it as a substance use disorder instead of substance dependence (Nehring & Freeman, 2024).
Pertinent Positives: Ongoing alcohol use, anxiety about rehab, fear of stigma, relationship strain.
Pertinent Negatives: No withdrawal symptoms, no history of treatment for substance use.
- Adjustment Disorder with Anxiety (ICD-10 Code: F43.22)
Lisa’s anxiety and emotional distress are significantly tied to her recent life stressors, including the breakup with her partner and financial instability. The social/emotional upset seen after these stressors correlates with the diagnosis of adjustment disorder, in which symptoms occur due to stressors.
Rationale: While Lisa experiences anxiety, it is directly connected to specific life events rather than a pervasive anxiety disorder. The symptoms are seen in her expressed worry over her parenting and life situation; hence, even though developing anxiety is evident, in this case, the substance use disorder will accompany the anxiety (O’Donnell et al., 2020).
Pertinent Positives: Increased anxiety and emotional distress related to life events.
Pertinent Negatives: Symptoms do not meet the threshold for generalized anxiety disorder; no history of panic attacks.
- Generalized Anxiety Disorder (GAD) (ICD-10 Code: F41.1)
Lisa shows signs of excessive worry about her parenting abilities and the recent breakup, which has caused distress and irritability. She finds herself worrying about minor issues, reflecting characteristics of generalized anxiety disorder.
Rationale: Although anxiety is present, the depressive features related to her substance use and adjustment disorder are more prominent. The absence of physical symptoms commonly associated with GAD, such as muscle tension or panic attacks, reduces the likelihood of this diagnosis being primary (Munir & Takov, 2022).
Pertinent Positives: Excessive worry, irritability, difficulty sleeping.
Pertinent Negatives: No panic attacks, but there is an absence of somatic symptoms like muscle tension.
Main diagnosis: Substance Use Disorder, Alcohol (ICD-10 Code: F10.20)
Justification: Based on the symptoms exhibited by Lisa—ongoing alcohol use, anxiety regarding rehabilitation, and significant impairment in her daily functioning—the most appropriate diagnosis is Substance Use Disorder, Alcohol. Her symptoms, including a reluctance to recognize the severity of her drinking and the associated emotional distress, confirm this diagnosis (Puddephatt et al., 2021). Early intervention is crucial to address her substance use and to prevent further deterioration of her mental health, which could have lasting effects on her relationships and overall well-being.
Reflections:
Reflecting on Lisa’s case, I recognize several aspects that could be approached differently if I were to conduct the session again. The first thing I do would be to foster a relationship of trust with the employees from the onset. Preventing herself from being referred to as an “addict”, Lisa’s main assessment concern is her great levels of anxiety. If the healthcare provider uses motivational interviewing techniques at the beginning of the session, then it may be easier to express herself fluently. This also would enable me to discuss her uncertainty about her treatment to make her less uncomfortable when speaking of her substance abuse and emotional issues.
In terms of legal and ethical considerations, it is crucial to navigate the potential mandatory reporting requirements concerning Lisa’s parenting, particularly regarding her substance use and its impact on her ability to care for her daughter, Sarah. While confidentiality is paramount in mental health treatment, the safety of the child must also be considered. I would need to explore the ethical implications of reporting and the importance of involving social services while respecting Lisa’s autonomy. Furthermore, understanding the stigma associated with substance use in her cultural context is vital. I would approach these topics sensitively, emphasizing support rather than judgment.
Regarding health promotion and disease prevention, I would stress continuity of care that should encompass not only substance use disorder but also the patient’s psychological and physiological state in general Interests. This approach involves briefing her on the effects of substance use on parenting, besides the possible cumulative impact on her health and future. I would also need to know her sociocultural background, as stress, poverty, and recent relationship issues cause anxiety. Perhaps, by offering resources for the support groups with which she can cope with cultural and economic factors, she would have a better chance at healthy healing.
Lastly, I would make sure that the presenting treatment plan respects the cultural aspect of Lisa’s background, focusing particularly on her status as a single mother. Some of the issues it entails are the possibility of hurdles she may experience in her search for care, including transportation and lack of funds, and hunting for actionable techniques to help her gain the capacity to seek assistance.
References
Zakhari, R. (2020). The Psychiatric-Mental Health Nurse Practitioner Certification Review manual. Springer Publishing Company.
Munir, S., & Takov, V. (2022). Generalized anxiety disorder. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441870/
Nehring, S. M., & Freeman, A. M. (2024, March 16). Alcohol use disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK436003/
O’Donnell, M. L., Agathos, J. A., Metcalf, O., Gibson, K., & Lau, W. (2020). Adjustment disorder: Current developments and future directions. International Journal of Environmental Research and Public Health, 16(14), 2537. https://doi.org/10.3390/ijerph16142537
Puddephatt, J., Irizar, P., Jones, A., Gage, S. H., & Goodwin, L. (2021). Associations of common mental disorder with alcohol use in the adult general population: A systematic review and meta-analysis. Addiction, 117(6). https://doi.org/10.1111/add.15735
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
An important consideration when working with patients is their cultural background. Understanding an individual’s culture and personal experiences provides insight into who the person is and where he or she may progress in the future. Culture helps to establish a sense of identity, as well as to set values, behaviors, and purpose for individuals within a society. Culture may also contribute to a divide between specific interpretations of cultural behavior and societal norms. What one culture may deem as appropriate another culture may find inappropriate. As a result, it is important for advanced practice nurses to remain aware of cultural considerations and interpretations of behavior for diagnosis, especially with reference to substance-related disorders. At the same time, PMHNPs must balance their professional and legal responsibilities for assessment and diagnosis with such cultural considerations and interpretations.
For this Assignment, you will practice assessing and diagnosing a patient in a case study who is experiencing a substance-related or addictive disorder. With this and all cases, remember to consider the patient’s cultural background.
TO PREPARE:
- Review this week’s Learning Resources and consider the insights they provide.
- Review the Comprehensive Psychiatric Evaluation template, which you will use to complete this Assignment.
- By Day 1 of this week, select a specific video case study to use for this Assignment from the Video Case Selections choices in the Learning Resources. View your assigned video case and review the additional data for the case in the “Case History Reports” document, keeping the requirements of the evaluation template in mind. (See attached)
- Consider what history would be necessary to collect from this patient.
- Consider what interview questions you would need to ask this patient.
- Identify at least three possible differential diagnoses for the patient.
Assessing and Diagnosing Patients with Substance-Related and Addictive Disorders
BY DAY 7 OF WEEK 8
Complete and submit your Comprehensive Psychiatric Evaluation, including your differential diagnosis and critical-thinking process to formulate primary diagnosis.
Incorporate the following into your responses in the template:
- Subjective: What details did the patient provide regarding their chief complaint and symptomology to derive your differential diagnosis? What is the duration and severity of their symptoms? How are their symptoms impacting their functioning in life?
- Objective: What observations did you make during the psychiatric assessment?
- Assessment: Discuss the patient’s mental status examination results. What were your differential diagnoses? Provide a minimum of three possible diagnoses with supporting evidence, listed in order from highest priority to lowest priority. Compare the DSM-5-TR diagnostic criteria for each differential diagnosis and explain what DSM-5-TR criteria rules out the differential diagnosis to find an accurate diagnosis. Explain the critical-thinking process that led you to the primary diagnosis you selected. Include pertinent positives and pertinent negatives for the specific patient case.
- Reflection notes: What would you do differently with this client if you could conduct the session over? Also include in your reflection a discussion related to legal/ethical considerations (demonstrate critical thinking beyond confidentiality and consent for treatment!), health promotion and disease prevention taking into consideration patient factors (such as age, ethnic group, etc.), PMH, and other risk factors (e.g., socioeconomic, cultural background, etc.).
Resources:
- DSM-5-TR text
- Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan & Sadock’s synopsis of psychiatry (11th ed.). WoltersKluwer.
- Zakhari, R. (2020). The psychiatric-mental health nurse practitioner certification review manual. Springer.