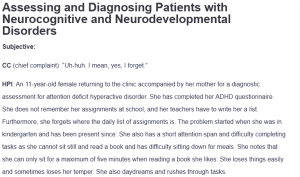
Assessing and Diagnosing Patients with Neurocognitive and Neurodevelopmental Disorders
Subjective:
CC (chief complaint): “Uh-huh. I mean, yes, I forget.”
HPI: An 11-year-old female returning to the clinic accompanied by her mother for a diagnostic assessment for attention deficit hyperactive disorder. She has completed her ADHD questionnaire. She does not remember her assignments at school, and her teachers have to write her a list. Furthermore, she forgets where the daily list of assignments is. The problem started when she was in kindergarten and has been present since. She also has a short attention span and difficulty completing tasks as she cannot sit still and read a book and has difficulty sitting down for meals. She notes that she can only sit for a maximum of five minutes when reading a book she likes. She loses things easily and sometimes loses her temper. She also daydreams and rushes through tasks.
Past Psychiatric History:
- General Statement: The patient has a negative history of any physical health illnesses or head trauma.
- Hospitalizations: Negative.
- Medication trials: Negative.
- Psychotherapy or Previous Psychiatric Diagnosis: The patient has never been diagnosed with any psychiatric illness or had psychotherapy.
Substance Current Use and History: The patient has never taken any substance of abuse.
Family Psychiatric/Substance Use History: The patient has no history of any psychiatric or chronic illness or substance use in her family.
Psychosocial History: The patient lives with her parents in Washington. She has a younger brother.
Other: The patient sleeps for 9-10 hours a night. Her PCP notes that she has proper nutrition.
Medical History:
- Current Medications: The patient is not on any medication.
- Allergies: No known food or drug allergies.
ROS:
- GENERAL: Denies weight loss or weight gain.
- HEENT: Denies loss in hearing or visual functionalities, nasal discharge, or swallowing discomfort.
- CARDIOVASCULAR: Denies palpitations.
- RESPIRATORY: Denies wheezing or shortness of breath.
- GASTROINTESTINAL: Denies inconsistencies in bowel movements.
- NEUROLOGICAL: Denies anxiety or depression.
- MUSCULOSKELETAL: Denies muscle pain or joint swelling.
- ENDOCRINOLOGIC: Denies heat or cold intolerance.
Objective:
Vital signs: T- 97.4 P- 58 R 14 98/62 Ht 4’5 Wt 65lbs
Physical exam:
Cardiovascular exam: Cardiovascular examination is warranted to rule out hyperparathyroidism. Hyperthyroidism may sometimes present with restlessness. Cardiovascular assessment may provide insight into palpitations consistent with hyperthyroidism (Raguthu et al., 2022).
Eye exam: An eye exam is warranted where attention deficit disorders are probable. Vision tests can help rule out vision problems that sometimes mimic attention deficit disorders, such as attention deficit disorder (Hochhauser et al., 2022).
Diagnostic exam: ADHD is a clinical diagnosis made after a thorough history taking. However, different scales exist that aid the diagnosis of the disorders. The Vanderbilt ADHD scale is an example of a diagnostic assessment scale with teacher and parent components. The tool can help aid the diagnosis (Bowling & Nettleton, 2020).
Assessment:
Mental Status Examination: The patient is alert and responsive. She seems restless and fidgets a lot during the interview. When allowed to view pictures on the wall, she runs her eyes from painting to painting multiple times. Her judgment and memory are intact. Her thought process is also logical.
Differential Diagnoses:
- Attention Deficit Hyperactive Disorder (ADHD) ICD-10 Code F90.9: ADHD is a psychiatric condition characterized by developmentally inappropriate levels of inattentiveness, hyperactivity, or impulsivity. Patients with ADHD often present with a short attention span, lack of concentration, forgetfulness, ease of losing things, and difficulty completing tasks. In the ADHD of hyperactivity type, restlessness and irritability are apparent. Per the DSM-V diagnostic criteria, these symptoms must have been present for six months or more (Bowling & Nettleton, 2020). The presence of forgetfulness, short attention span, difficulty completing tasks, ease of losing things, and fidgeting for a period exceeding six months in the case presented made ADHD the probable diagnosis.
- Generalized Anxiety Disorders (GAD) ICD-10 Code F41.1: GAD is a mental health disorder characterized by persistent worry. The presence of restlessness, fidgeting, and difficulty completing tasks warranted the inclusion of this differential (Mishra & Varma, 2023). However, the absence of persistent worrying makes this differential less probable.
- Dysthymic disorder ICD-10 Code F34.1: Dysthymic disorder is a psychiatric illness characterized by a low-level depression that is not as severe as major depressive disorder. Children with the disorder commonly manifest as being irritable or having low moods (Schramm et al., 2020). The presence of irritability warranted the inclusion of this differential. It was, however, ruled out due to the absence of depressive manifestations.
Diagnoses: The presumptive diagnosis is ADHD. The presence of inattentiveness, forgetfulness, fidgeting, and restlessness provide insight into ADHD of combined type. The absence of sustained worry ruled out GAD.
Reflections:
The assessment captured diverse aspects of assessing and diagnosing neurodevelopmental disorders. A legal consideration for the client borders on HIPAA laws on access to children’s health information. In this case, information obtained from individual counseling should only be shared if it is in the child’s best interest. Access to healthcare is a social determinant of health applicable to the case. Caregivers can guarantee acceptable mental healthcare to the patients and their families by engaging them during the design of the therapeutic plan. Further, the interview captured many assessment aspects of substance use disorder. As a point of health promotion, the family should be educated on the disease process and possible interventions to address it.
Conclusively, neurodevelopmental disorders remain a health concern. These disorders cause suffering and functional debilitations across the lifespan. The assessment demonstrated assessment points for persons with ADHD. The patient in the case could benefit from
References
Bowling, Z., & Nettleton, A. (2020). The diagnosis and management of ADHD (attention deficit hyperactivity disorder) in children and young people: A commentary on current practice and future recommendations. BJGP Open, 4(1). https://doi.org/10.3399/bjgpopen20x101043
Hochhauser, M., Aran, A., & Grynszpan, O. (2022). Change blindness in adolescents with attention-deficit/hyperactivity disorder: Use of eye-tracking. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.770921
Mishra, A. K., & Varma, A. R. (2023). A comprehensive review of the Generalized Anxiety Disorder. Cureus. https://doi.org/10.7759/cureus.46115
Raguthu, C. C., Gajjela, H., Kela, I., Kakarala, C. L., Hassan, M., Belavadi, R., Gudigopuram, S. V., & Sange, I. (2022). Cardiovascular involvement in thyrotoxicosis resulting in heart failure: The risk factors and hemodynamic implications. Cureus. https://doi.org/10.7759/cureus.21213
Schramm, E., Klein, D. N., Elsaesser, M., Furukawa, T. A., & Domschke, K. (2020). Review of dysthymia and persistent depressive disorder: History, correlates, and clinical implications. The Lancet Psychiatry, 7(9), 801–812. https://doi.org/10.1016/s2215-0366(20)30099-7
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Neurodevelopmental disorders begin in the developmental period of childhood and may continue through adulthood. They may range from the very specific to a general or global impairment, and often co-occur (APA, 2022). They include specific learning and language disorders, attention deficit hyperactivity disorder (ADHD), autism spectrum disorders, and intellectual disabilities. Neurocognitive disorders, on the other hand, represent a decline in one or more areas of prior mental function that is significant enough to impact independent functioning. They may occur at any time in life and be caused by factors such brain injury; diseases such as Alzheimer’s, Parkinson’s, or Huntington’s; infection; or stroke, among others.
For this Assignment, you will assess a patient in a case study who presents with a neurocognitive or neurodevelopmental disorder.
To Prepare:
- Review this week’s Learning Resources and consider the insights they provide. Consider how neurocognitive impairments may have similar presentations to other psychological disorders.
- Review the Comprehensive Psychiatric Evaluation template, which you will use to complete this Assignment.
- By Day 1 of this week, select a specific video case study to use for this Assignment from the Video Case Selections choices in the Learning Resources. View your assigned video case and review the additional data for the case in the “Case History Reports” document, keeping the requirements of the evaluation template in mind.
- Consider what history would be necessary to collect from this patient.
- Consider what interview questions you would need to ask this patient.
- Identify at least three possible differential diagnoses for the patient.
By Day 7 of Week 10
Complete and submit your Comprehensive Psychiatric Evaluation, including your differential diagnosis and critical-thinking process to formulate primary diagnosis.
Incorporate the following into your responses in the template:
- Subjective: What details did the patient provide regarding their chief complaint and symptomology to derive your differential diagnosis? What is the duration and severity of their symptoms? How are their symptoms impacting their functioning in life?
- Objective: What observations did you make during the psychiatric assessment?
- Assessment: Discuss the patient’s mental status examination results. What were your differential diagnoses? Provide a minimum of three possible diagnoses with supporting evidence, listed in order from highest priority to lowest priority. Compare the DSM-5-TR diagnostic criteria for each differential diagnosis and explain what DSM-5-TR criteria rules out the differential diagnosis to find an accurate diagnosis. Explain the critical-thinking process that led you to the primary diagnosis you selected. Include pertinent positives and pertinent negatives for the specific patient case.
- Reflection notes: What would you do differently with this client if you could conduct the session over? Also include in your reflection a discussion related to legal/ethical considerations (demonstrate critical thinking beyond confidentiality and consent for treatment!), health promotion and disease prevention taking into consideration patient factors (such as age, ethnic group, etc.), PMH, and other risk factors (e.g., socioeconomic, cultural background, etc.).
Assessing and Diagnosing Patients with Neurocognitive and Neurodevelopmental Disorders
submission information
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
- To submit your completed assignment, save your Assignment as WK10Assgn_LastName_Firstinitial
- Then, click on Start Assignment near the top of the page.
- Next, click on Upload File and select Submit Assignment for review.
Resources:
- DSM-5-TR text
- Koch, C. (2016, January 1). Does brain size matter? Scientific American. https://www.scientificamerican.com/article/does-brain-size-matter1/
- Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan & Sadock’s synopsis of psychiatry (11th ed.). WoltersKluwer.
- Zakhari, R. (2020). The psychiatric-mental health nurse practitioner certification review manual. Springer.