Aquifer Case Study – Depression and Insomnia
The case is of a 65-year-old female who presented to the clinic on her initial visit with complaints of insomnia for six months that failed to resolve after therapy. She is unable to focus, expresses a lack of interest, and decreased energy. She is a known hypertensive and diabetic. She also has hypercholesterolemia. Assessment findings revealed a 10-pound weight gain over the past year. She demonstrated improvement in her sleep and interest in starting sertraline.
Final Diagnosis
Depression (ICD-10 F32.9) and Insomnia (ICD-10 G47.00): The presumptive diagnosis in the case presented is depression and insomnia comorbidity. The client had a persistent lack of interest, an inability to focus, and depressed energy. These symptoms impacted her social functioning and had been present for over six months. She also had chronic insomnia lasting over six months. These manifestations qualify the diagnosis of depression and insomnia. Depression is a psychiatric illness characterized by persistent depressed mood, loss of interest in things, hopelessness, and irritability (Christensen et al., 2020). As per the fifth edition of the Diagnostc and Statistical Manual for Mental Health Disorders (DSM-V) criteria for diagnosing major depression, these symptoms must have been present for not less than six months and must be affecting the social functioning of an individual (DSM-V, n.d.). Insomnia and weight gain are also apparent in depression. Comorbidities of depression and insomnia are common. According to the American Psychiatric Association guidelines on the diagnosis of depression, a depression-insomnia comorbidity is diagnosed in the presence of depression symptoms and insomnia not alleviated with conventional sedatives (Chan, 2024). This warranted the diagnosis of depression and insomnia.
Differential Diagnoses
Uncomplicated Bereavement ICD-10 Code Z63.4: There are some symptom similarity beween uncomplicated grief and major depressive disorder. These include insomnia, feelings of sadness and anger, a lack of appetite, loss of interest in otherwise enjoyable things, and hopelessness. These symptoms may persist for weeks or months (Cacciatore & Frances, 2022). The persistence of diminished energy, a lack of interest, and insomnia, following the loss of a loved one warranted the inclusion of this differential. Unlike major depression, where depressive episodes are constant, the painful feelings and corresponding manifestations of dullness and loss of interest in uncomplicated bereavements are intermittent (Cacciatore & Frances, 2022). This excluded this diagnosis.
Hypothyroidism ICD-10 Code E03.9: Hypothyroidism is a medical condition characterized by low production of thyroid hormone. Patients with hypothyroidism will commonly manifest with weight gain, depressed mood, fatigue, and sensitivity to cold (Zamwar & Muneshwar, 2023). This differential was included due to the presence of low mood and weight gain. A thyroid panel may be necessary to rule out the diagnosis. Nonetheless, the patient was responsive to the sertraline medication given to her. She also lacked other classical features of hypothyroidism, such as puffiness, skin changes, and cold intolerance. It is thus unlikely that the patient has hypothyroidism.
Diagnostics
Depression diagnosis is arrived at after a thorough history taking. Assessment tools such as the patient health questionnaire (PHQ-9) are valuable in screening for depression in primary care settings. The tools maintain effectiveness in assessing the severity of the disease and can guide the diagnosis process.
Treatment, Education, and Follow-Up
Treatment Plan
The patient will be started on a cognitive behavioral therapy (CBT) program and continued on sertraline. According to the American College of Physicians guidelines on managing depression and insomnia comorbidity, combination therapy utilizing CBT and SSRIs are first line (Qaseem et al., 2023). CBT and SSRI combination is effective in elevating the mood of the patients and promoting sleep. The patient in the case will thus benefit from this therapeutic modality. Sertraline is a selective serotonin reuptake inhibitor (SSRI) that is effective in addressing depressive episodes. It is initiated at doses of 50 mg, administered orally in once-daily dosing. Dose increments of 25 mg at weekly intervals can be necessitated to optimize response.
Education and Follow-Up
The patient will be educated on depressive disorder and its impact on health. She will be advised to take her medications as prescribed and adhere to the CBT program for optimal response. She will also be advised to maintain good sleep hygiene and indulge in physical activity, as exercise elevates mood and may help alleviate depressive episodes (Marx et al., 2022). She should also be told to return to the clinic after one month. Monthly clinical visitation allows healthcare providers to assess the response of their patients to the prescribed medications and make adjustments as necessary.
References
Cacciatore, J., & Frances, A. (2022). DSM-5-TR turns normal grief into a mental disorder. The Lancet Psychiatry, 9(7). https://doi.org/10.1016/s2215-0366(22)00150-x
Chan, L. G. (2024). The comorbidity and associations between depression, cognitive impairment, and sleep after stroke and how they affect outcomes: A scoping review of the literature. Journal of Vascular Diseases, 3(2), 134–151. https://doi.org/10.3390/jvd3020012
Christensen, M. C., Wong, C. M., & Baune, B. T. (2020). Symptoms of major depressive disorder and their impact on psychosocial functioning in the different phases of the disease: Do the perspectives of patients and healthcare providers differ? Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00280
DSM-V. (n.d.). DSM. Psychiatry.org – DSM. https://www.psychiatry.org/psychiatrists/practice/dsm
Marx, W., Manger, S. H., Blencowe, M., Murray, G., Ho, F. Y.-Y., Lawn, S., Blumenthal, J. A., Schuch, F., Stubbs, B., Ruusunen, A., Desyibelew, H. D., Dinan, T. G., Jacka, F., Ravindran, A., Berk, M., & O’Neil, A. (2022). Clinical guidelines for the use of lifestyle-based mental health care in major depressive disorder: World federation of societies for biological psychiatry (WFSBP) and Australasian Society of Lifestyle Medicine (ASLM) Taskforce. The World Journal of Biological Psychiatry, 24(5), 333–386. https://doi.org/10.1080/15622975.2022.2112074
Qaseem, A., Owens, D. K., Etxeandia-Ikobaltzeta, I., Tufte, J., Cross, J. T., & Wilt, T. J. (2023). Nonpharmacologic and pharmacologic treatments of adults in the acute phase of major depressive disorder: A living clinical guideline from the American College of Physicians. Annals of Internal Medicine, 176(2), 239–252. https://doi.org/10.7326/m22-2056
Zamwar, U. M., & Muneshwar, K. N. (2023). Epidemiology, types, causes, clinical presentation, diagnosis, and treatment of hypothyroidism. Cureus. https://doi.org/10.7759/cureus.46241
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
Weekly Directions
• Complete the required Aquifer case studies as assigned each week and take a screenshot of your student summary report at the completion of each case.
• When creating a screenshot of the case summary report, make sure it includes your name, the name or title of the case, and a clear display of the time you spent in the case. PLEASE FOLLOW THE ESSAY LAY-OUT I WILL ATTACH
• Of the two cases assigned, choose one of the two cases and write an essay on the case, per the guidelines below. Please note: BELOW IS MY CASE SCENARIO AND DETAILS
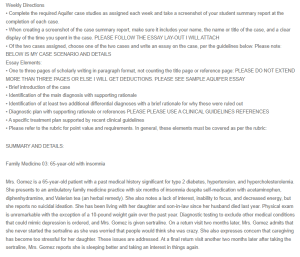
Aquifer Case Study – Depression and Insomnia
Essay Elements:
• One to three pages of scholarly writing in paragraph format, not counting the title page or reference page: PLEASE DO NOT EXTEND MORE THAN THREE PAGES OR ELSE I WILL GET DEDUCTIONS. PLEASE SEE SAMPLE AQUIFER ESSAY
• Brief introduction of the case
• Identification of the main diagnosis with supporting rationale
• Identification of at least two additional differential diagnoses with a brief rationale for why these were ruled out
• Diagnostic plan with supporting rationale or references PLEASE PLEASE USE A CLINICAL GUIDELINES REFERENCES
• A specific treatment plan supported by recent clinical guidelines
• Please refer to the rubric for point value and requirements. In general, these elements must be covered as per the rubric:
SUMMARY AND DETAILS:
Family Medicine 03: 65-year-old with insomnia
Mrs. Gomez is a 65-year-old patient with a past medical history significant for type 2 diabetes, hypertension, and hypercholesterolemia. She presents to an ambulatory family medicine practice with six months of insomnia despite self-medication with acetaminophen, diphenhydramine, and Valerian tea (an herbal remedy). She also notes a lack of interest, inability to focus, and decreased energy, but she reports no suicidal ideation. She has been living with her daughter and son-in-law since her husband died last year. Physical exam is unremarkable with the exception of a 10-pound weight gain over the past year. Diagnostic testing to exclude other medical conditions that could mimic depression is ordered, and Mrs. Gomez is given sertraline. On a return visit two months later, Mrs. Gomez admits that she never started the sertraline as she was worried that people would think she was crazy. She also expresses concern that caregiving has become too stressful for her daughter. These issues are addressed. At a final return visit another two months later after taking the sertraline, Mrs. Gomez reports she is sleeping better and taking an interest in things again.
• Differential diagnosis: Uncomplicated Bereavement ICD-10 Code Z63.4
Hypothyroidism ICD-10 Code E03.9
• Final diagnosis: DEPRESSION (ICD-10 F32.9) AND INSOMNIA (ICD-10 G47.00)
– Depression and insomnia are the final diagnoses for Mrs. Gomez due to the persistence and severity of her symptoms, which include lack of interest, inability to focus, decreased energy, and chronic insomnia lasting six months. These symptoms significantly impacted her daily functioning and quality of life. Additionally, her symptoms improved notably after starting sertraline, an antidepressant, which is effective for treating depression. The chronic nature of her insomnia, despite self-medication, further supports the diagnosis. The combination of these factors—persistent depressive symptoms, chronic insomnia, and positive response to antidepressant treatment—confirms that depression and insomnia are the appropriate final diagnoses.
***WHEN YOU PUT MEDICATION AS TREATMENT. PLEASE MAKE SURE TO PUT THE NAME OF THE MEDICATION, DOSAGE, ROUTE AND FREQUENCY